 Research Article
Research Article
Comparison of the Effects of Foam Rolling and Instrument-Assisted Soft Tissue Mobilization Methods on Iliotibial Band Tightness
Gokhan Maras1* and Gamze Gülsün Pala2
1Selçuk University Kulu Faculty of Health Sciences Department of Physiotherapy and Rehabilitation, Konya, Turkey
2Amasya University, Department of Physical Therapy and Rehabilitation, Amasya, Turkey
Corresponding AuthorGokhan Maras, Selçuk University Kulu Faculty of Health Sciences Department of Physiotherapy and Rehabilitation, Dinek Neighbourhood Kulu/Konya, Turkey
Received Date:July 31, 2025; Published Date:August 06, 2025
Introduction
The iliotibial band (ITB), or iliotibial tract, is a structure formed by the thickening of the tensor fasciae latae on the lateral aspect of the thigh. The ITB originates superiorly at the level of the greater trochanter and inserts distally at the Gerdy tubercle on the anterolateral surface of the tibia [1]. At the level of the lateral femoral condyle, there is contact between the ITB, the underlying epicondyle, and the origin of the lateral collateral ligament. This unique anatomical relationship plays an important role in maintaining stability on the lateral aspect of the knee joint [1, 2]. Owing to its role in stabilizing the knee joint, the iliotibial band (ITB) is subjected to increased tension during repetitive flexion and extension movements, which may, over time, contribute to structural damage. The literature frequently reports various ITBrelated injuries, particularly among athletic individuals [1-3].
The most common ITB-related pathologies include ITB syndrome (ITBS), Morel-Lavallée lesions, external hip syndrome, traumatic tears, iliotibial insertional tendinosis and peritendonitis, avulsion fractures of the Gerdy tubercle, and Segond fractures. The occurrence of such a wide variety of ITB injuries poses a significant risk factor, particularly for athletes [1]. ITB syndrome (ITBS) is a common clinical condition characterized by sharp, localized, lateral knee pain experienced mostly at around 30° of knee flexion during repetitive knee flexion-extension movements. ITBS is reported to be responsible for 10% of all lower extremity overuse syndromes seen in runners [4] and 24% of all overuse syndromes seen in cyclists [5]. It may be necessary to take a break from activities from time to time due to pain [5]. Patients with ITBS often experience decreased hip adduction, likely due to insufficient flexibility of the ITB. Therefore, a treatment that can increase hip adduction and reduce pain may be beneficial [6]. In ITB-related pathologies, such as ITBS stretching, pain-relieving techniques, and other conservative treatments are often used as first-line treatment [6]. Assessing ITB tension, which can cause many different types of lesions, is a clinically important issue. The first clinical test for ITB assessment was developed by Ober and later modified and updated by Kendall [7,8].
Tension in soft tissues causes increased sensitivity in the affected areas [9]. As the tension level in the ITB increases, sensitivity in the tissue increases, leading to changes in the pain threshold. The lowest pressure level that causes pain is defined in the literature as the pressure pain threshold (BPT) [10]. This threshold can be measured quantitatively using a device called an algometer [11]. Foam rolling (FR) is a technique that has gained significant popularity in recent years. Research shows that FR can increase range of motion (ROM) without decreasing strength and power performance [12,13]. It is also suggested that it can accelerate the recovery process from post-exercise muscle damage [12,14]. Foam rolling is frequently used for therapeutic purposes in the treatment of various soft tissue pathologies; however, it should be emphasized that the scientific evidence supporting this use is limited [15]. FR is used as a complement to manual therapy to improve range of motion (ROM) and relieve pain-related symptoms [16,14]. Applied to the ITB, FR is a widely preferred adjunctive method for treating conditions such as patellofemoral pain syndrome [17], runner’s knee [18], and hip bursitis [19]. Recently, FR has become a popular practice among the general population, becoming a part of pre-workout routines to increase range of motion, facilitate spontaneous soft tissue mobilization, contribute to the pre-exercise warm-up process, and reduce symptoms related to muscle soreness [14,16,20,21].
Systematic reviews have aimed to evaluate the effects of foam rolling on post-exercise muscle recovery and performance, particularly with respect to range of motion (ROM) [22,23]. Findings showed that one week of foam rolling increased hip extension ROM, but this effect returned to baseline after one week. Participants reported a decrease in pain after the treatment. However, pain reduction was observed in both the treated and untreated legs, suggesting that mechanisms beyond myofascial release may be involved in the pain reduction [24,25,22]. However, there is also evidence supporting the role of myofascial release, suggesting that this technique may contribute to the relief of pain associated with ITBS [26]. Instrument-assisted soft tissue mobilization (IASTM) is performed by clinicians using specialized tools made from various shapes and materials to mechanically relieve fascial restrictions or adhesions [27]. This technique also induces microtrauma in the target tissue, initiating an inflammatory process. This process stimulates collagen production and contributes to the remodelling of disorganized collagen fibres, helping to reduce pain and increase range of motion (ROM) [27]. IASTM is reported to be more effective when applied to acute or chronic injuries characterized by decreased flexibility and muscle strength. Due to its significant biomechanical advantages and potential clinical benefits in shortening and reducing stiffness in hypertonic muscles, this method is widely preferred by many manual therapists today to improve soft tissue mobility [28]. The therapeutic benefits of IASTM application occur in a short time; increase in range of motion and decrease in pain and hypertonicity are observed [29]. In this study, our aim was to investigate the effects of IASTM and FR methods on joint range of motion and pressure pain threshold in individuals with ITB tightness and to compare them with each other.
Our aim in this study was to investigate the immediate and 6-week effects of IASTM and FR methods on joint range of motion and pressure pain threshold in individuals with ITB strain and to compare them with each other.
Materials and Methods
Subjects
Thirty (13 female, 17 male) adult volunteers with ITB tightness were included in this study. Exclusion criteria included history of hip, knee, or lumbar spine surgery; history of autoimmune disease including fibromyalgia or rheumatoid arthritis; history of lower extremity skin lesions; ankle instability; lower extremity hyperalgesia; hematoma; varicose veins; skin infection; current participation in a stretching program or use of a foam roller within the past six weeks; and pregnancy. Approval for the study was received from the Amasya University Ethics Committee and signed consent was obtained from all participants.
Study Design
Participants were randomly assigned to two groups using a randomization program: IASTM (n = 15) and FR (n = 15). Participants received three sessions of IASTM and FR per week for 6 weeks. Participants did not participate in any other exercise program during the study. The same investigator performed all sessions, and the assessments were performed by another investigator blinded to each other. Passive hip adduction range of motion and pressure pain threshold assessments were performed for all participants. The Ober Test was used to assess hip adduction range of motion, and a digital algometer (Lafayette Instruments, Lafayette, Indiana) was used to assess pressure pain threshold. Measurements were taken at three different time points within the scope of the study: before the first session, immediately after the session, and within 48 hours following the last session. Before all assessments, participants completed a 3-minute warm-up protocol on a stationary bicycle at a self-determined pace. Following the warm-up, range of motion (ROM) and pressure pain threshold (PPT) were measured, with the order of assessments maintained constant. All assessments were performed in the same order and under standardized conditions for each participant. As part of the intervention protocol, each participant underwent 5 minutes of instrument-assisted soft tissue mobilization (IASTM) and foam rolling (FR) techniques. Before these sessions, participants completed a 3-minute warm-up exercise using the same method.
Randomization and Blinding
The randomization process was conducted using a blocking method. All measurements were performed by a single researcher. The IASTM and FR protocols applied to the intervention groups were also conducted by the same researcher. The researcher conducting the assessments and the researcher conducting the interventions worked independently and were unaware of each other’s roles.
Ober’s Test
The Ober test is a clinical assessment method used to determine the level of flexibility of the iliotibial band (ITB), which extends from the tensor fasciae latae muscle to the anterolateral region of the tibia [3,8]. During the test, the subject is positioned in a sidelying position with the lower extremity in 90° flexion. The examiner stands behind the subject and passively abducts and extends the upper leg while simultaneously stabilizing the pelvis with one hand to ensure pelvic stability. Following this movement, the upper leg is released, allowing gravity to guide it toward the table. The degree to which the leg approaches the table is considered a parameter reflecting the level of tension in the iliotibial band.
An inclinometer is used for measurement; this device is placed slightly above the lateral femoral condyle and measures the angle between the femur and the horizontal plane. This angle is called the “Ober test inclination angle.” Lower angle values indicate greater tension in the ITB [30, 8]. Maintaining a stable position during the test is a significant challenge. Therefore, a second researcher provided support during the measurement process to ensure accurate reading of the inclinometer. Furthermore, to increase the consistency of the assessments, all measurements were performed by the same expert.
Pressure Pain Threshold
Since individuals with ITB tightness often report pain approximately 3 cm superior to the lateral femoral condyle, measurements were performed at this anatomical location [31]. The pressure pain threshold (PPT) of the ITB was assessed using a digital algometer (Lafayette Instruments, Lafayette, Indiana). Participants were positioned in a lateral position with both lower extremities in full extension during measurement. Before application, participants were briefed on the device’s operation. A 1 cm diameter hard rubber tip was placed over the measurement point, and pressure was gradually increased. Participants were asked to answer “yes” at the first sensation of pain or discomfort. Two measurements were taken for each measurement point, 30 seconds apart; the results were recorded in N/cm2 and the average calculated [32]. Reliability was ensured by the same investigator performing all assessments. Each measurement was repeated three times, and the average of these three values was used in the analysis.
IASTM
Participants in the IASTM group were positioned in a sidelying position with the affected side facing up, with their knees held at approximately 30° of flexion. During the intervention, the practitioner applied the IASTM instrument using a stroking technique, touching the skin along the iliotibial band from the greater trochanter to Gerdy’s tubercle, parallel to the tissue and at a 45° angle. Eight to 12 slow and controlled scraping movements were performed on the same anatomical area. The intensity of the IASTM application was adjusted to provide moderate mechanical stimulation to the fascial tissue, but was kept within a range that would not cause excessive pain to the participant. The duration of the application was limited to 5 minutes. A lubricating cream was applied to the area before the procedure to reduce friction between the skin and the instrument and prevent potential skin irritation.
FR
Participants in this group underwent the previously described foam rolling procedure for the ITB [33]. Participants were positioned with their bodies parallel to the floor, and the foam roller was placed between their thighs and the floor. Pressure was applied to the roller using their body weight; if necessary, the pressure level was adjusted by balancing with the hands and feet. The roller was positioned perpendicular to the long axis of the left thigh and aligned with the targeted tissue (ITB) area. The participant rolled the foam roller back and forth across the area extending from the greater trochanter to the lateral femoral epicondyle. The technique was then continued with short, kneading-like movements across the treated area, returning to the starting position with a single, uninterrupted movement. This cycle was repeated for 45 seconds, followed by a 15-second rest. A total of five repetitions were performed. Throughout the exercise, the researcher provided feedback on correct technique to the participants as needed.
Statistical Analysis
Analysis of the collected data was performed using the Statistical Package for the Social Sciences (SPSS) program, version 22.0 (SPSS Inc., Chicago, IL, USA). The normality of the distribution of numerical variables was assessed using the Shapiro-Wilk test and appropriate graphical techniques. Descriptive statistics for normally distributed numerical variables were reported as mean ± standard deviation (X±SD). Descriptive data for the dominant extremity were expressed as percentages. All variables were determined to be normally distributed. ANOVA for repeated measures was used to examine the differences in range of motion (ROM) and pressure pain threshold (PPT) measurements between the groups. When the sphericity assumption was not met, analysis was performed using the Greenhouse-Geisser correction. The following limitations were used for the effect size (η²): η² < 0.06: small effect, 0.06 ≤ η² < 0.14: moderate effect, η² ≥ 0.14: high effect [34]. Post-hoc power analysis of the study was performed using G*Power 3.1 software. Based on the analysis results, the power of the study was calculated as 80% if there were at least 14 participants in each group (28 people in total). In this calculation, the effect size ranged from 0.31 to 0.52, and the significance level was taken into account with a 5% margin of error (α=0.05) for the most predictive variable (e.g., flexibility or ROM). As a precaution against possible data loss, the sample size was increased by 15%, and a total of 30 participants (15 people for each group) were included. The level of statistical significance was set at p<0.05.
Results
A total of 30 participants were included in this study. The mean age of the participants was 30.93±7.21 years, and the mean body mass index (BMI) was 23.15±2.74 kg/m². When the distribution of the participants’ dominant side was examined, it was determined that only one individual was left-handed, while the remaining 29 participants were right-handed. No statistically significant differences were found between the groups in terms of age, height, body weight, BMI, or dominant side variables (p>0.05). Participant demographics are presented in Table 1.
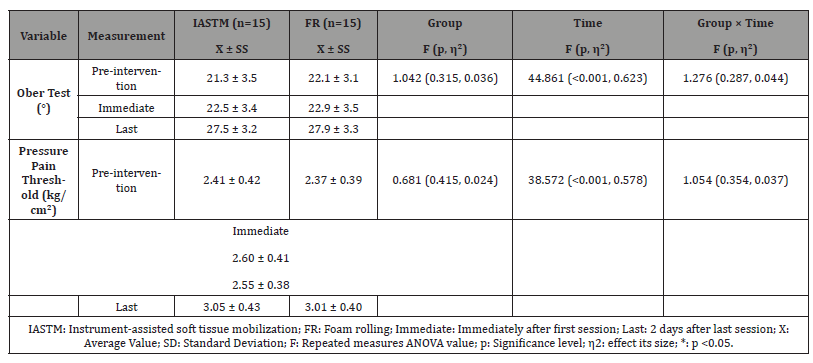
In the pre-intervention assessment, no statistically significant difference was found between the groups in terms of Ober inclination angles (p: 0.543). The time effect was found to be statistically significant (F (2,56) = 44.861, p < 0.001, η² = 0.623), indicating that both IASTM and FR applications led to significant improvements in Ober angle. However, the comparison between the groups did not reveal a significant difference (F (1,28) = 1.042, p = 0.315, η² = 0.036). Furthermore, the time × group interaction was not significant (F (2,56) = 1.276, p = 0.287, η² = 0.044). These findings indicate that the two groups showed similar levels of improvement and the difference between them was not statistically significant. Pressure Pain Threshold (kg/cm²). The time effect was found to be significant for both groups (F (2,56) = 38.572, p < 0.001, η² = 0.578), demonstrating that the interventions were effective in increasing the pain threshold. However, the difference between the groups was not significant (F (1,28) = 0.681, p = 0.415, η² = 0.024), and the group × time interaction was not statistically significant (F (2,56) = 1.054, p = 0.354, η² = 0.037). Therefore, both methods significantly increased the pain threshold, but neither method was superior to the other (Table 2).
Table 1:Demographic characteristics of the groups.
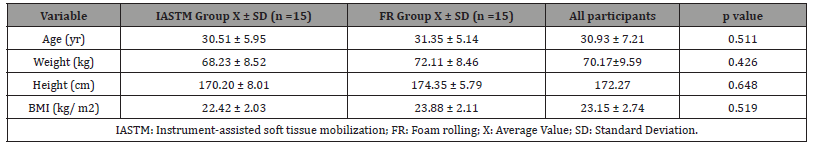
Table 2:A comparison of IASTM and FR groups pre, immediate and last intervention.
Discussion
The aim of this study was to investigate and compare the effects of IASTM and FR applications on hip adduction angle and pressure pain threshold in individuals with ITB tightness. The Ober test is a well-established clinical assessment tool frequently employed to evaluate ITB tightness [35]. As ITB stiffness increases, lateral mobility of the lower limb becomes restricted, leading to a reduction in hip adduction and consequently a decrease in the Ober inclination angle. In the present study, all intervention groups demonstrated improvements in hip adduction range of motion (ROM) after a six-week protocol. Notably, these gains were more pronounced in the groups receiving myofascial release (MFR) interventions, particularly those undergoing instrument-assisted soft tissue mobilization (IASTM).
These findings are consistent with those reported by Simatou et al [36]., who examined the effects of IASTM, foam rolling (FR), and static stretching applied to the non-dominant myofascial lateral lines of university students. Their results revealed increased hip adduction ROM across all groups, with the most significant enhancement observed in the IASTM group. Such outcomes support the hypothesis that MFR techniques, when combined with exercise, yield greater improvements in ROM than exercise or stretching alone [37]. The greater ROM observed in the IASTM group is likely attributable to physiological adaptations in the fascia and surrounding musculature induced by the intervention. Although ITB stretching on its own may provide clinical benefits, numerous studies suggest that combining it with MFR techniques leads to superior treatment efficacy by facilitating deeper fascial release and improved tissue mobility.
With respect to pain modulation, the current study found that pressure pain threshold (PPT) significantly improved in both the IASTM and FR groups, while the control group exhibited no notable change. The effect sizes of PPT improvement were large and comparable between the two intervention groups, suggesting that the observed analgesic benefits are primarily due to the application of MFR techniques rather than exercise alone [37]. Furthermore, in a study involving male football players with ITB tightness, increases in joint range of motion and pressure pain threshold (PPT) were observed in both the IASTM and foam rolling (FR) intervention groups. However, the inclusion of only male football players was acknowledged as a limitation of the study [38]. Supporting this, a randomized controlled trial by Kim et al. involving participants with short hamstrings found that a single IASTM session produced greater increases in PPT compared to other interventions [22]. However, to date, no studies have specifically investigated the effect of IASTM on PPT in the ITB region. The findings of the present study are therefore novel and suggest that the increase in PPT in the IASTM group may be due to a reflexive reduction in fascial tension elicited during treatment.
Similarly, a significant increase in pressure pain threshold (PPT) was observed in the FR group. This finding may be attributed to the longer duration and consistent application protocol of the FR intervention used in this study, compared to previous studies employing shorter protocols. Although both IASTM and FR techniques have been shown to enhance PPT across various anatomical regions, this study is the first to investigate the acute and six-week effects of IASTM and FR interventions on joint range of motion and PPT in individuals with ITB tightness, regardless of gender. As such, it provides novel insights to the existing body of literature.
Conclusions
Six weeks of IASTM and FR therapy in individuals with iliotibial band tightness was found to increase hip adduction angle and pressure pain threshold. However, no significant difference was observed between the two treatments in terms of ROM and pressure pain threshold. Therefore, it is believed that IASTM and FR therapy will positively impact ROM and pressure pain threshold parameters in individuals with iliotibial band stiffness. Clinicians can use this information to develop targeted and effective treatment plans for individuals with ITB tightness and improve overall function using either technique.
Conflict of Interest
The authors have no conflicts to report.
References
- Flato R, Passanante GJ, Skalski MR, Patel DB, White EA, et al. (2017) The iliotibial tract: imaging, anatomy, injuries, and other pathology. Skeletal Radiol 46(5): 605-622.
- Strauss EJ, Kim S, Calcei JG, Park D (2011) Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg 19(12): 728-736.
- Aderem J, Louw QA (2015) Biomechanical risk factors associated with iliotibial band syndrome in runners: a systematic review. BMC Musculoskeletl Disord 16(1): 356.
- Jakobsen B, Kroner K, Schmidt S, Kjeldsen A (1994) Prevention of injuries in long-distance runners. Knee Surg Sports Traumatol Arthrosc 2(4): 245-249.
- Holmes JC, Pruitt AL, Whalen NJ (1993) Iliotibial band syndrome in cyclists. Am J Sports Med 21(3): 419-424.
- Beals C, Flanigan D (2013) A review of treatments for iliotibial band syndrome in the athletic population. J Sports Med 2013(1): 367169.
- Ober FR (1935) Back strain and sciatica. Journal of the American Medical Association, 104(18): 1580-1583.
- Reese NB, Bandy WD (2003) Use of an inclinometer to measure flexibility of the iliotibial band using the Ober test and the modified Ober test: differences in magnitude and reliability of measurements. J Orthop Sports Phys Ther 33(6): 326-330.
- Hamstra-Wright KL, Jones MW, Courtney CA, Maiguel D, Ferber R (2020) Effects of iliotibial band syndrome on pain sensitivity and gait kinematics in female runners: A preliminary study. Clin Biomech 76:105017.
- Fischer AA (1987) Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain 30(1): 115-126.
- Van der Heijden RA, Rijndertse MM, Bierma-Zeinstra SM, van Middelkoop M (2018) Lower pressure pain thresholds in patellofemoral pain patients, especially in female patients: a cross-sectional case-control study. Pain Med 19(1): 184-192.
- Beardsley C, Škarabot J (2015) Effects of self-myofascial release: a systematic review. J Bodyw Mov Ther 19(4): 747-758.
- MacDonald GZ, Penney MD, Mullaley ME, et al. (2013) An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. J Strength Cond Res 27(3): 812-821.
- Pearcey GE, Bradbury-Squires DJ, Kawamoto J-E, Drinkwater EJ, Behm DG, et al. (2015) Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. J Athl Train 50(1): 5-13.
- Wilke J, Vogt L, Banzer W (2018) Immediate effects of self-myofascial release on latent trigger point sensitivity: a randomized, placebo-controlled trial. Biol sport 35(4): 349-354.
- MacDonald GZ (2013) Foam rolling as a recovery tool following an intense bout of physical activity. Memorial University of Newfoundland.
- Green S (2005) Patellofemoral syndrome. Journal of bodywork and movement therapies 9(1): 16-26.
- Fredericson M, Wolf C (2005) Iliotibial band syndrome in runners: innovations in treatment. Sports Med 35(5): 451-459.
- Strauss EJ, Nho SJ, Kelly BT (2010) Greater trochanteric pain syndrome. Sports Med Arthrosc Rev 18(2): 113-119.
- Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, et al (2008) Three-dimensional mathematical model for deformation of human fasciae in manual therapy. Journal of Osteopathic Medicine, 108(8): 379-390.
- Sheffield K, Cooper N (2013) The Immediate Effects of Self-Myofascial Release on Female Footballers. SportEX Dynamics (38).
- Cheatham SW, Kolber MJ, Cain M, Lee M (2015) The effects of self‐myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. Int J Sports Phys Ther 10(6): 827-838.
- Wilke J, Müller A-L, Giesche F, Power G, Ahmedi H, et al. (2020) Acute effects of foam rolling on range of motion in healthy adults: a systematic review with multilevel meta-analysis. Sports Med 50(2): 387-402.
- Aboodarda S, Spence A, Button DC (2015) Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC Musculoskelet Disord 16(1): 265.
- Cavanaugh MT, Döweling A, Young JD, Quigley PJ, Hodgson DD, et al. (2017) An acute session of roller massage prolongs voluntary torque development and diminishes evoked pain. Eur J Appl physiol 117(1): 109-117.
- Pepper TM, Brismée J-M, Sizer Jr PS, Kapila J, Seeber GH, et al. (2021) The immediate effects of foam rolling and stretching on iliotibial band stiffness: a randomized controlled trial. Int J Sports Phys Ther 16(3): 651-661.
- Ercole B, Antonio S, Ann DJ, Stecco C (2010) How much time is required to modify a fascial fibrosis? J Bodyw Mov Ther, 14(4): 318-325.
- Fowler S, Wilson JK, Sevier TL (2000) Innovative approach for the treatment of cumulative trauma disorders. Work, 15(1): 9-14.
- Baker RT, Hansberger BL, Warren L, Nasypany A (2015) A novel approach for the reversal of chronic apparent hamstring tightness: a case report. Int J Sports Phys Ther 10(5): 723-733.
- Ferber R, Kendall KD, McElroy L (2010) Normative and critical criteria for iliotibial band and iliopsoas muscle flexibility. J Athl Train 45(4): 344-348.
- Patel DR, Villalobos A (2017) Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Transl Pediatr 6(3): 190-198.
- Fabio Antonaci M, Sand T, Lucas G A (1998) Pressure algometry in healthy subjects: inter-examiner variability. Scand J Rehab Med 30(1): 3-8.
- Okamoto T, Masuhara M, Ikuta K (2014) Acute effects of self-myofascial release using a foam roller on arterial function. The J Strength Cond Res 28(1): 69-73.
- Gignac GE, Szodorai ET (2016) Effect size guidelines for individual differences researchers. Personality and individual differences 102: 74-78.
- Willett GM, Keim SA, Shostrom VK, Lomneth CS (2016) An anatomic investigation of the ober test. Am J Sports Med 44(3): 696-701.
- Simatou M, Papandreou M, Billis E, Tsekoura M, Mylonas K, et al. (2020) Effects of the Ergon® instrument-assisted soft tissue mobilization technique (IASTM), foam rolling, and static stretching application to different parts of the myofascial lateral line on hip joint flexibility. J Phys Ther Sci 32(4): 288-291.
- Cheatham SW, Lee M, Cain M, Baker R (2016) The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc 60(3): 200-211.
- Unuvar BS, Demirdel E, Gercek H (2024) The effects of different myofascial release techniques on pain, range of motion, and muscle strength in athletes with iliotibial band tightness: a randomized controlled study. J Sport Rehabil 33(7):531-541.
- Kim D-H, Lee JJ, Hyun You J (2018) Effects of instrument-assisted soft tissue mobilization technique on strength, knee joint passive stiffness, and pain threshold in hamstring shortness. J Back Musculoskelet Rehabil 31(6): 1169-1176.
-
Gokhan Maras* and Gamze Gülsün Pala.Comparison of the Effects of Foam Rolling and Instrument-Assisted Soft Tissue Mobilization Methods on Iliotibial Band Tightness. Glob J Ortho Res. 5(2): 2025. GJOR.MS.ID.000607.
-
Iliotibial band; foam rolling; instrument-assisted soft tissue mobilization; pressure pain threshold; range of motion
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






