Research Article
Research Article
Factors Associated with the time to Breast Feeding Cessation among children aged one to four Years in a Rural area in Democratic Republic of Congo
Olivier Mukuku1*, Patricia Lukusa Mishika2, Loriot K Mudisu1, Kristel N Tshibanda1, Augustin M Mutombo, Stanislas O Wembonyama3 and Oscar N Luboya1,2,3
1Institut Supérieur des Techniques Médicales de Lubumbashi, Lubumbashi, Democratic of Republic Congo, Central Africa
2School of Public Health, University of Lubumbashi, Lubumbashi, Democratic of Republic Congo, Central Africa
3Department of Pediatrics, Faculty of Medicine, University of Lubumbashi, Lubumbashi, Democratic of Republic Congo, Central Africa
Olivier Mukuku, Institut Supérieur des Techniques Médicales de Lubumbashi, Lubumbashi, Democratic of Republic Congo, Central Africa.
Received Date: July 19, 2019; Published Date: July 31, 2019
Abstract
Objective: To identify the factors associated with the breastfeeding cessation before 12 months age in Tshamalale village in the Democratic Republic of Congo.
Methods: This is a cross-sectional study of the feeding practices of children aged 1 to 4 years in the village of Tshamalale. It took place from April 1st to 30th, 2013.
Results: All of our respondents (n=200) reported breastfeeding their children. Early initiation of breastfeeding was performed in 37% of cases. The mean duration of exclusive breastfeeding was 4.0±1.6 months (range: 1 day and 12 months) and the mean age of breastfeeding was 17.37±4, 70 months (range: 3 to 28 months). 85% (140/174) of respondents reported that they stopped breastfeeding their children between 13 and 24 months of age. Late initiation to breastfeeding (OR=3.24 [1.18-8.92]) and child’s sibling rank first (OR=3.45 [1.18-10.10]) were factors that significantly associated to breastfeeding cessation before the age of 12 months.
Conclusion: The study shows that there is an urgent need for mothers’ education on breastfeeding and weaning recommendations in Tshamalale.
Keywords:Breastfeeding; Cessation; Factors associated; Child
Introduction
Breastfeeding provides many health benefits by protecting the mother and child. Optimal breastfeeding is one of the most effective preventive health measures against diarrheal diseases and infant mortality. Studies indicate that breast milk protects infants against infectious and chronic diseases [1,2]. Globally, 60% of infant and young child deaths occur as a result of inappropriate infant feeding practices and infectious diseases, two-thirds of which are attributable to poor breastfeeding practices [2]. Infant feeding practices may have a negative effect on children’s growth and development, particularly in developing countries where access to basic health services is not sufficient [3]. In developing countries, feeding practices are very often inadequate and inconsistent with World Health Organization (WHO) recommendations and are the main factors affecting the physical growth and mental development of the child [4]. Poor nutritional status in early childhood also affects health in adulthood [5]. Nutritional status is the best indicator of child well-being and, indirectly, the well-being of the community.
The Democratic Republic of Congo (DRC) is one of five countries in the world (India, Nigeria, Pakistan and China) with a high death rate among children under 5 and malnutrition is one of the leading causes of death in these countries [6]. Despite the WHO recommendation, the maintenance of breastfeeding after the first year of the child’s life is practiced by few women, being more common in low-income countries, where the prevalence of BF at 12 months and 24 months is higher than 90% and 60%, respectively. According to the recent Demographic and Health Survey conducted in the DRC, almost all children are breastfed (98%), but only 52% of children are breastfed within one hour of birth and only 48% of children are exclusively breastfed until the age of 6 months. It also reports that half of the children are breastfed for a period of 21.8 months [7]. The aim of this study was to identify the factors associated with the breastfeeding cessation before 12 months in the village of Tshamalale in the DRC.
Methods
Study setting
We conducted our investigation in the village of Tshamalale around the city of Lubumbashi in the province of Haut-Katanga in the southeastern of DRC. This village is bounded by the Kassapa district (in the North), the Mupundu and Mwita villages (in the South), the Golf and Kalubwe districts (in the East) and the villages of Kyaluwaya and Poleni (in the West). In 2005, this village had 3600 inhabitants but currently the number is not known and the area either.
Study design and period
This is a cross-sectional study of feeding practices of children aged 1 to 4 years in Tshamalale village around the city of Lubumbashi. It took place from April 1 to May 1, 2013. A motherchild couple was considered per household and 200 households were randomly selected in this village. The data were collected on the basis of a pre-established and pretested questionnaire.
Study variables
Variables studied were: The socio-demographic characteristics of the respondents and their children: maternal age, mother’s level of education, child’s age, child’s sex and sibling rank of the child; Child feeding practices: time of breastfeeding initiation (considered early when the child is put into the baby within one hour of birth), duration of exclusive breastfeeding (considered early when the exclusivity of breastfeeding lasts less than 6 months), time of introduction of complementary foods (considered early when the introduction of solid, semi-solid or soft foods is made before the age of 6 months), time of breastfeeding cessation (considered early when this arrest was made before the age of 12 months), use of infant formula milk [8].
Statistical analyzes: The various data collected were analyzed using STATA 12 software. The analysis and interpretation used the calculation of the proportion, the mean and the standard deviation (SD). The Chi-square test of Pearson or the exact Fischer test when recommended was used for frequency comparison (expressed as a percentage). The odds ratio (OR) is presented with a 95% confidence interval. The materiality threshold was set at p <0.05.
Ethical considerations: The recruitment was anonymous. In addition, women included in the study are recruited only after their prior consent. The information collected was analyzed in strict confidentiality. At the end of the interview, the shortcomings noted in the interviews regarding child feeding practices were corrected through the health education provided by us.
Results
Socio-demographic characteristics of the respondents and their children
The mean age of the respondents was 29.09±6.36 years (range: 17 to 43 years). 47% of the respondents were aged between 20 and 29, and 59% (118/200) of them had at least a secondary level (Table 1).
Table 1: Socio-demographic characteristics of our sample.
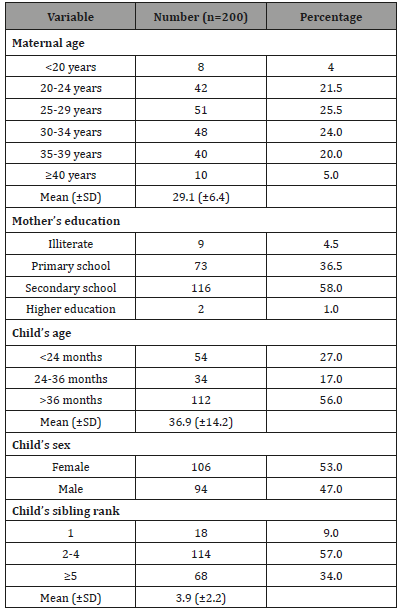
The mean of child’s age was 36.94±14.24 months (range: 12 to 60 months). Twenty-seven percent of children were under 24 months of age and in 53% of cases (106/200) the children of our respondents were female.
Regarding the child’s sibling rank, 9% of them were first born; the mean rank in the siblings was 3.90±2.16 (range: 1 to 12).
Child feeding practices
All of our respondents reported breastfeeding their children, which is a 100% breastfeeding rate. At the time of the survey, 26 women (13%) said they were still breastfeeding their children. Early initiation of breastfeeding is performed in 37% of cases and in 60% of cases, children were breastfed between the 1st and 24th hours after birth (Table 2).
Table 2: Infant feeding practices of children in Tshamalale.
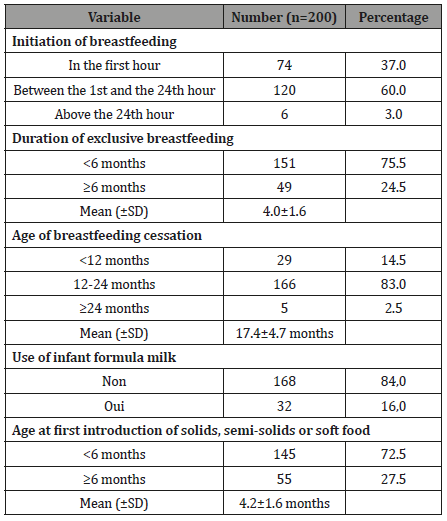
The mean duration of exclusive breastfeeding was 4.0±1.6 months (range: 1 day to 12 months), and almost a quarter of children were breastfed exclusively for at least 6 months.
The mean age of breastfeeding cessation was 17.37±4.70 months (range: 3 and 28 months). 80.5% (140/174) of mothers reported that they stopped breastfeeding their children between 13 and 24 months of age. Sixteen percent of respondents reported giving their children infant formula milk in combination or not with breast milk. The mean age of introduction of infant formula milk into the child’s diet was 3.48±2.22 months.
The mean age of introduction of complementary foods was 4.20±1.59 months (range: 1 to 12 months). 72.5% (55/200) of the respondents reported introducing a complementary food before 6 months and in all cases, the cereal derivatives constituted the complementary food.
Factors associated to breastfeeding cessation before 12 months of age
Child’s sibling rank had a significant influence on breastfeeding cessation before 12 months of age. Compared with other children, breastfeeding was stopped earlier (i e, at <12 months) in first-born babies (33.3% versus 12.6%; OR = 3.45 [1.18-10.10]) (Table 3).
Table 3: Facteurs influençant larrêt de lallaitement maternel avant lâge de 12 mois à Tshamalale.
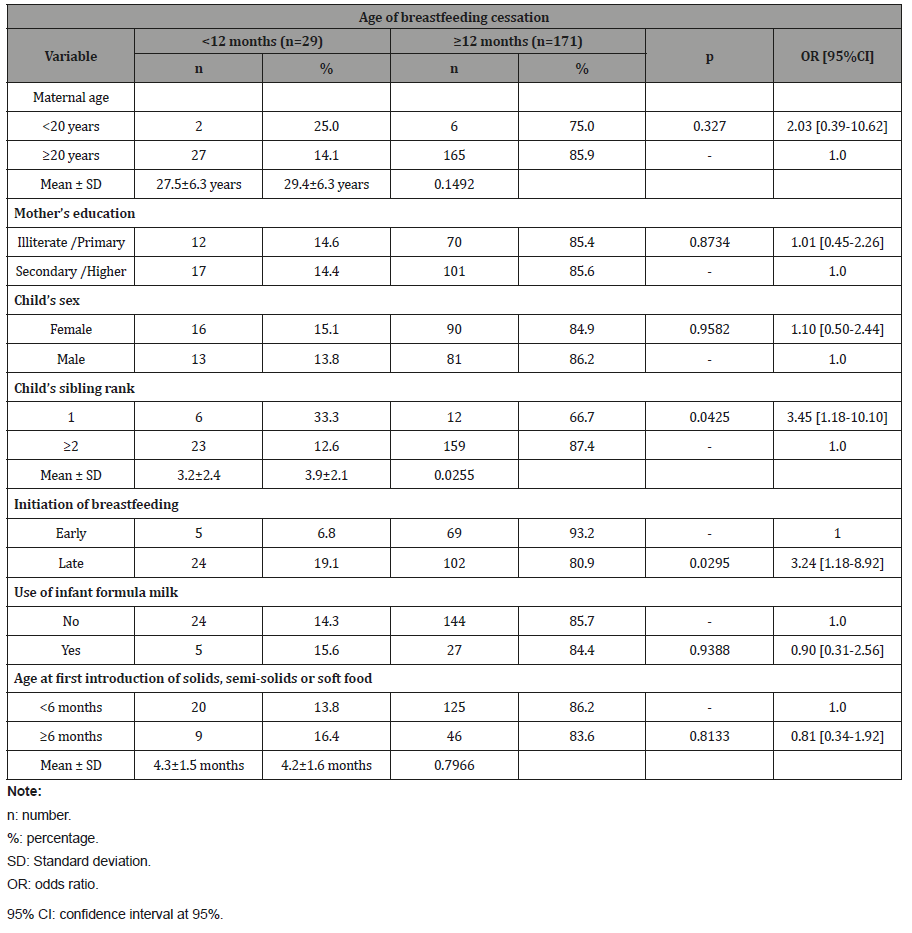
In studying the influence of child feeding practices on the continuation of breastfeeding, we found that late initiation to breastfeeding (that is, after the first hour after delivery) was significantly associated with early breastfeeding cessation. We found that breastfeeding after the first hour of birth reduces the overall duration of breastfeeding (OR = 3.24 [1.18-8.92]).
Discussion
Breastfeeding rate
The breastfeeding rate in our study was 100% among our respondents. Epidemiological data show large differences concerning breastfeeding rates between the continents and even between countries of the same continent. In Africa, Gamgne- Kamga (Cameroon) and Sepou (Central African Republic) had breastfeeding rates of 99.48% [9] and 96.5% [10] respectively. In Northeastern Brazil, we find similar trends where Neusa [11] found a rate of 99% of mothers who breastfed their newborn [11] and the United Arab Emirates where Radwan reported 98 % [12].
In Europe, the breastfeeding rate (at maternity exit) was 98% in Sweden while it was 69% in the United Kingdom [13]. In France, between 53 and 58% of newborns were initially breastfed [14,15]. In the same country, the rate of breastfeeding can also vary according to the environment (urban and rural) [7]. Thus, in 2008, a study conducted in China by Liqian found a low breastfeeding rate of 62.8% in urban areas compared to 83.4% in rural areas [16].
Early initiation into breastfeeding
About one in three children (37%) had first breastfeeds in the first hour after delivery. According to WHO recommendations, the child must be breastfed within 60 minutes of birth [4]. Gamgne- Kamga, in her study, found that 78.4% of her respondents breastfed their babies within 24 hours after delivery [9]. In Gambia, a survey of 324 lactating women in 12 villages reported a breastfeeding rate of nearly 40% within 24 hours of delivery and explained this was due to poor women’s knowledge of colostrum. These women regarded colostrum as bad milk and even as pus for some of them who prefer expressing the breast in order to evacuate the colostrum until the milk changes color and becomes white [17].
Breastfeeding cessation
In our study, the mean age of children at breastfeeding cessation was 17.37 months. This age was shortened in Siyou’s study, where breastfeeding cessation occurred around 9.2 months on average [18]. This study finds the first born in siblings and late initiation to breastfeeding as negatively associated factors in the continuation of breastfeeding. As noted in previous studies [19], we found that breastfeeding duration increases with the child’s sibling rank and that the last child is often the one who breastfed the longest. Indeed, with the experience they gain, mothers gain confidence in their abilities and there are fewer barriers to prolonged breastfeeding. They take the insurance to stand up to bad advice, especially that of some health professionals. In general, first-born breastfeeding is used as a reference afterwards to breastfeed at least as much as the following children [19].
A study conducted in Lubumbashi and surrounding areas reported that breastfeeding duration was significantly longer for rural women (17.9 months on average) than urban women (16.4 months on average) [20]. The same is true in the Demographic and Health Survey (DHS-DRC II) which reported that children are breastfed longer in rural areas (median of 22.7 months) than in urban areas (20 months); and that the median duration of breastfeeding decreased as the level of living of the household increased (22.9 months for children from low socioeconomic households to 18.5 months for those with socio-economic level) [7]. In contrast, Noirhomme-Renard, in a review of the literature, pointed out that socio-economically advantaged women breastfed longer than women with low socioeconomic status [21].
In the Gamgne-Kamga’s study, breastfeeding cessation was earlier for married women and women with high levels of education [9]. Nlend, on the other hand, found that the mother’s age negatively affected the duration of breastfeeding in general [22]. Ben-Slama, in his study, reported the child’s lack of time and refusal of the breast as the main justifications given by the mothers surveyed who stopped breastfeeding early [23].
According to Thulier and Whalen, the incidence and duration of breastfeeding depend on the combination of several factors including physical, behavioral, social and economic factors [24,25]. Lauzon-Guillain adds the parental impression of the child’s needs, that is, the perception that the child is completely satisfied with breast-feeding [26].
However, according to the recommendations of the American Academy of Pediatrics, WHO and UNICEF, children must be exclusively breastfed for up to six months and continue until the age of two, and that from six months, this breast milk must be supplemented by the introduction of an appropriate complementary food [4,27]. We found no difference in breastfeeding duration by sex of the child. This observation is identical to that reported in DHS-DRC II [7].
Conclusion
The results showed that the child’s sibling rank (first-born) and delayed initiation to breastfeeding were the factors that negatively influenced the continuation of breastfeeding after 12 months of age in Tshamalale village. To improve breastfeeding practices, programs at the national level will be needed, but with focus on target groups with insufficient breastfeeding practices.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Jackson KM, Nazar AM (2006) Breastfeeding, the Immune Response, and Longterm Health. J Am Osteopath Assoc 106(4): 203-207.
- (2003) World Health Organization. Global Strategy for Infant and Young Child Feeding. Geneva, Switzerland: A joint WHO/UNICEF statement. Geneva: WHO.
- Mukuku O, Mutombo AM, Kamona LK, Lubala TK, Mawaw PM, et al. (2019) Predictive Model for the Risk of Severe Acute Malnutrition in Children. Journal of Nutrition and Metabolism.
- (2001) World Health Organization. Report of the expert consultation on the optimal duration of exclusive breastfeeding. Geneva: WHO.
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, et al. (2008) For the Maternal and Child Undernutrition Study Group. Maternal and Child Undernutrition: Consequences for Adult Health and Human Capital. Lancet 371: 340-357.
- Liu L, Oza S, Hogan D, Perin J, Rudan I, et al. (2015) Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 385: 430-440.
- Ministère du Plan et Suivi de la Mise en œuvre de la Révolution de la Modernité (MPSMRM), Ministère de la Santé Publique (MSP) et ICF International, 2014. Enquête Démographique et de Santé en République Démocratique du Congo 2013-2014. Rockville, Maryland, MPSMRM, MSP et ICF International, USA.
- (2009) Organisation Mondiale de la Santé. Indicateurs pour évaluer les pratiques d’alimentation du nourrisson et du jeune enfant: Première partie-Dé Washington, DC: OMS, USA.
- Gamgne Kamga B (2009) Etude des connaissances et pratiques des mères sur l'allaitement maternel à l'hôpital provincial et à la PMI de Bafoussam, Cameroun. Thèse de doctorat en médecine, Institut supérieur des sciences et de la santé de Bangangté.
- Sepou A, Yanza MC, Nguembi E, Tetpa G, Ngbale R (2001) Quelle valeur l'allaitement maternel a-t-il en milieu urbain et semi urbain centrafricain? Santé 11 (2): 85-9.
- Neusa M, Pedro I, Marilia C (2001) Breastfeeding and early weaning practices in Northeast Brazil: A longitudinal study. Pediatrics 108 (4): e66.
- Radwan H (2013) Patterns and determinants of breastfeeding and complementary feeding practices of Emirati Mothers in the United Arab Emirates. BMC Public Health 13: 171.
- Graffy J, Taylor J, Williams A, Eldridge S (2004) Randomised controlled trial of support from volunteer counselors for mothers considering breast feeding. BMJ 328(7430): 26.
- Turck D (2005) Allaitement maternel: les bénéfices pour la santé de l'enfant et de sa mè Archives de pédiatrie 12 (S3): 145-165.
- Cattaneo A, Yngve A, Koletzko B, Guzman LR (2005) Protection, promotion and support of breast-feeding in Europe: current situation. Public Health Nutr 8(1): 39-46.
- Liqian Qiu, Zhao Y, Binns CW, (2008) A cohort study of infant feeding practices in city, suburban and rural areas in Zhejiang Province, PR China. Int Breastfeed J 3: 4.
- Semega Janneh IJ, Bohler E, Holm H, Matheson I, Holmboe Ottesen G (2001) Promoting breastfeeding in rural Gambia: combining traditional and modern knowledge. Health Policy Plan 16(2): 199-205.
- Siyou H (2006) Pratiques de diversification alimentaire des nourrissons par les mères consultant au centre mère et enfant de la Fondation Chantal Biya à Yaoundé. Mémoire de spécialisation en pé Faculté de Médecine et des Sciences Biomédicales, Université de Yaoundé 1, Caméroun.
- De Bruyn ML (2013) Expériences de femmes autour de l'allaitement maternel prolongé. Thèse de Médecine, Université de Caen, France.
- Lubala TK, Mukuku O, Mutombo AM, Lubala N, Nawej FN, et al. (2016) Infant feeding practices in urban and rural southern Katanga communities in Democratic Republic of Congo. Journal of Medical Research 2(3): 65-70.
- Noirhomme Renard F, Noirhomme Q (2009) Facteurs associés à un allaitement prolongé au-delà de trois mois: une revue de la litté Journal de Pédiatrie et de Puériculture 22: 112-120.
- Nlend A, Wamba G, Same Eboko C (1997) Alimentation du nourrisson de 0 à 36 mois en milieu urbain camerounais. Méd Afr Noire; 44 (1): 47-51.
- Ben Slama F, Ayari I, Ouzini F, Belhadj O, Achour N (2010) Allaitement maternel exclusif et allaitement mixte: connaissances, attitudes et pratiques des primipares. Eastern Mediterranean Health Journal 16(6): 630-36.
- Thulier D, Mercer J (2009) Variables associated with breastfeeding duration. J Obstet Gynecol Neonatal Nurs 38(3): 259-268.
- Whalen B, Cramton R (2010) Overcoming barriers to breastfeeding continuation and exclusivity. Curr Opin Pediatr 22(5): 655-663.
- de Lauzon Guillain B, Wijndaele K, Clark M, Acerini CL, Hughes IA, et al. (2012) Breastfeeding and Infant Temperament at Age Three Months. PLoS ONE 7(1): e29326.
- Gartner LM, Morton J, Lawrence RA, Naylor AJ, O’Hare D, et al. (2005) Breastfeeding and the use of human milk. Pediatrics 115(2): 496-506.
-
Olivier Mukuku, Patricia Lukusa Mishika, Loriot K Mudisu, Kristel N Tshibanda, Augustin M Mutombo, et al. Factors Associated with the time to Breast Feeding Cessation among children aged one to four Years in a Rural area in Democratic Republic of Congo Glob J Nutri Food Sci. 2(2): 2019. GJNFS.MS.ID.000533.
-
Breast feeding Cessation, Children, Factors associated, Child, health benefits, mother, diarrheal diseases, breast milk protects, chronic diseases, adulthood, analysis, complementary foods, infant formula milk, child feeding practices, health education
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.