 Research Article
Research Article
Exploring the Treatment of Noncatheterized Urinary Tract Infections in Nursing Home Patients
Harkirat S Bal*
Department of Nursing, California State University, Fresno, USA
Harkirat S Bal, Department of Nursing, California State University, Fresno, USA.
Received Date: June 23, 2021; Published Date: July 13, 2021
Abstract
Antibiotic overuse is an ongoing problem, causing widespread antibiotic resistance. This research conducted a retrospective chart review in two nursing homes during a 9-month period to determine appropriate antibiotic use with 105 residents treated for UTIs. Only 31 (29.6%) received appropriate treatment based on the McGeer criteria. Furthermore, 48 (45.7%) residents did not show symptoms and 46 (43.8%) lacked microbiologic evidence in their urine reports. Despite the introduction of antibiotic stewardship in the nursing homes, providers were treating presumed UTIs with antibiotics. This study found a substantial disparity between the antibiotic stewardship program and providers’ diagnoses of UTI.sensitivity to aging, it was determined that the participants were moderately sensitive.
Keywords: Antibiotics; Asymptomatic Bacteriuria; Geriatrics; Infections; Inappropriate Treatment; Mcgeer Criteria; Nursing Homes; UTI
Introduction
Urinary tract infection (UTI) is the second most common nosocomial infection in long-term care facilities (LTCFs), and the incidence of asymptomatic bacteriuria (ASB) is higher than symptomatic UTIs in LTCFs [1]. Identifying UTIs in the elderly population is challenging because of chronic comorbidities, including dementia, aphasia, or other communication barriers. The current guidelines from the Infectious Disease Society of America (IDSA) are that asymptomatic UTIs should not be treated [2].
The two major sets of guidelines for assisting providers in diagnosing and treating symptomatic UTIs are the McGeer criteria and Loeb criteria.1 McGeer issued the first guidelines for managing UTIs in the LTCFs in 1991. Unfortunately, providers often mistreat asymptomatic UTIs in LTCFs. Inappropriate use of antibiotics does not improve survival or symptoms and often results in recurrent multidrug-resistant bacteria infections [1].
Background and Significance
Over 1.4 million residents are living in U.S. nursing homes [3]. As our nation’s population ages, the burden of UTIs in elderly patients residing in LTCFs is expected to grow. About one-third of hospitalizations of patients from LTCFs are due to UTIs [1]. There is a need to improve nursing home practices for appropriate treatment selection, initiation, and duration of therapy for UTIs. Inappropriate prescribing of antibiotics results in recolonization and increases the incidence of Clostridium difficile and the risk of antibiotic resistance [4]. Despite the introduction of antibiotic stewardship programs (ASPs) in nursing homes, the use of antibiotics to treat suspected UTIs persist.
Purpose of the Study
The purpose of this study was to conduct a retrospective chart review to determine if nursing home staff were following the recommended practice guidelines for initiating antibiotic treatment of UTIs by using the McGeer criteria.
Methods
Human Subjects Protection
The administrators at both facilities approved the study. Approval from the Fresno State Institutional Review Board was obtained prior to the study. A waiver of individual informed consent was received before accessing Private Health Information (PIH) because no personal identifiers were included in the database.
Setting
To prevent bias, the author did not conduct the study at his workplace. Two nursing homes in central California agreed to participate. The first nursing home was a 176-bed for-profit facility with an average census of 150; the second nursing home was a 140- bed for-profit facility with an average census of 130. Both of the facilities were located in a city with a population of 133,010. Both of the nursing homes were under the same parent company, as such, they both used the same electronic charting system. Both of these facilities had implemented an ASP based on the McGeer criteria.
Population and Sample
The inclusion criteria included geriatric patients over the age of 50, admitted to the nursing facility, without an indwelling catheter in place or a catheter that had been removed more than two days prior to the onset of the symptoms, where the day of catheter removal was day one. The sample size was 105 patients of mixed age, gender, and ethnicity. The Chi-Square test power calculation was used to estimate the sample size. If the antibiotic was ordered for UTI, that patient became part of the sample to investigate further the appropriateness of antibiotic use based on the McGeer criteria. If a patient was diagnosed with multiple UTIs during the look-back period, each episode was considered a separate event. Patients with indwelling catheters and patients under palliative hospice care were excluded. Also, patients admitted from acute hospitals with antibiotics were excluded from the study. If the antibiotic was started in the ER and the patient was sent back to the facility, the case was included because the facility was responsible for followup with the urine culture.
Data Collection Method
A retrospective chart review of two nursing homes was based on data from August 2018 through December 2018. The look-back period was 9 months and included medical records for all patients who received antibiotics for presumed UTIs. The review included provider progress notes, nursing notes for signs and symptoms of UTI, laboratory evaluation (such as UA or CBC), provider’s orders, medication administration sheets, infection log sheet, and the MDS assessment. The chart audit also included relevant demographic information, functional status, ADL scale, and cognitive status. The decision was based on the standardized tool (using the McGeer’s criteria). According to the McGeer’s criteria [5], for residents without an indwelling catheter, both criteria 1 and 2 must be present.
• a. At least 1 of the following sign or symptoms subcriteria.
• b. Acute dysuria or acute pain, swelling or tenderness of the testes, epididymis or prostate. OR
• c. Fever or leukocytosis and at least 1 of the following urinary tract subcriteria.
• Acute costovertebral angle pain or tenderness.
• Suprapubic pain.
• Gross hematuria.
• New or marked increase in incontinence.
• New or marked increase in urgency.
• New or marked increase in frequency.
d. In the absence of fever or leukocytosis, then two or more of the following localizing urinary tract subcriteria.
• Suprapubic pain.
• Gross hematuria.
• New or marked increase in incontinence.
• New or marked increase in urgency.
• New or marked increase in frequency.
e. And either of the following microbiologic subcriteria.
f. At least 105 cfu/mL of no more than two species of microorganisms in a voided urine sample. OR
g. At least 102 cfu/mL of any number of organisms in a specimen collected by in-and-out catheter.
Data Analysis Method
For the statistical analysis, this researcher counted (i) how many patients were diagnosed with UTIs appropriately using McGeer criteria, (ii) whether the patient was prescribed appropriate antibiotics based on the urine culture report, (iii) whether providers made appropriate changes to treatment once urine cultures and sensitivity reports were available (such as discontinue antibiotic if culture is negative or change antibiotic if it is resistant to the bacteria).
Results
A total of 183 patients’ medical records were reviewed. Of those records, 34 cases were excluded due to the presence of indwelling Foley catheters, 19 cases were excluded due residents being under hospice services, and 25 cases were excluded as these residents were admitted with antibiotics from the acute hospitals. In total, 105 records across Nursing Home 1 (n = 46) and Nursing Home 2 (n = 59) were reviewed for documentation of a presumed UTI. For this study, 105 cases were analyzed, and the unit of analysis was patient cases.
Patient Characteristics
Within both nursing homes, 85 (81%) of the cases were women, with a mean age of 83.44 (SD = 9.76). Most of the patients were classified as White (n = 79, 75.2%). Only one (1%) patient was Black and 25 (23.8%) were Hispanic. Most of the patients (n = 71, 67.6%) needed extensive assistance based on their ADL scores (3- 4).
Descriptive statistics for patient characteristics stratified by nursing homes are presented in Tables 1, 2, and 3. A series of chisquare, Mann-Whitney U, and independent t-test analyses were used to examine patient characteristics across the two nursing homes for similarities and differences.
The chi-square tests of independence examined if each categorical variable was similar across the two nursing homes for association [6]. The independent-samples t-test determined differences between the mean ages of patients between Nursing Home 1 and Nursing Home 2. Two Mann-Whitney U tests determined difference between the patients’ cognition status (brief interview for mental status) and functional status (ADLs) between Nursing Home 1 and Nursing Home 2. A value of 05 was set to determine significance. A series of analyses demonstrated that patient characteristics across the two nursing homes were similar (see Table 1), with the exception of patients in Nursing Home 2 having a significantly higher mean age (see Tables 1, 2, & 3; p = .008).
Table 1:McGeer’s Criteria for Residents Without an Indwelling Catheter.
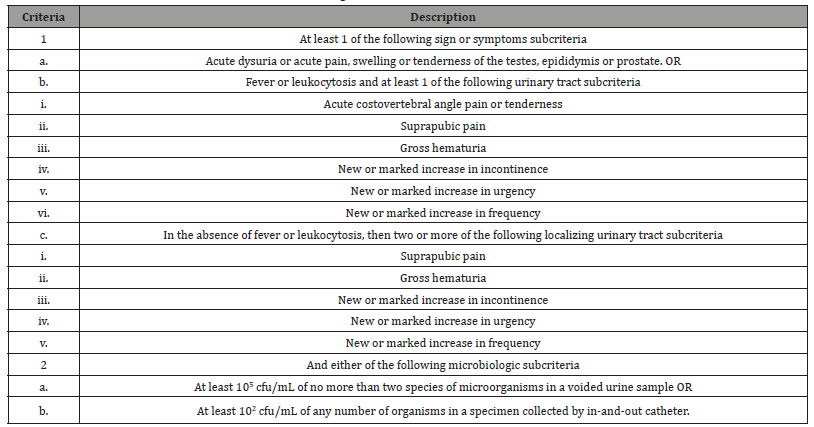
Table 2:Patient Demographics Disaggregated by Nursing Home.
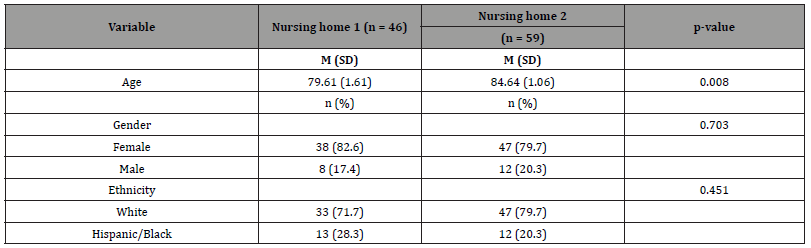
Table 3:Patient BIMS and ADLs Disaggregated by Nursing Home.
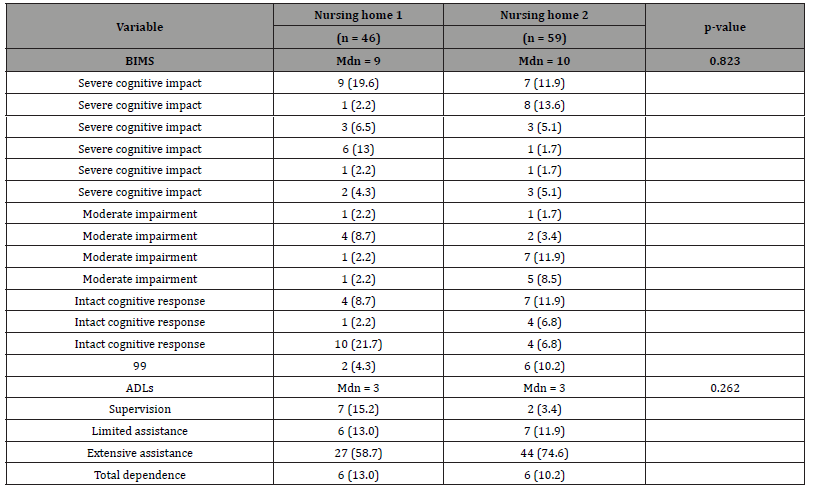
Table 4:Patient Disorders Disaggregated by Nursing Home.
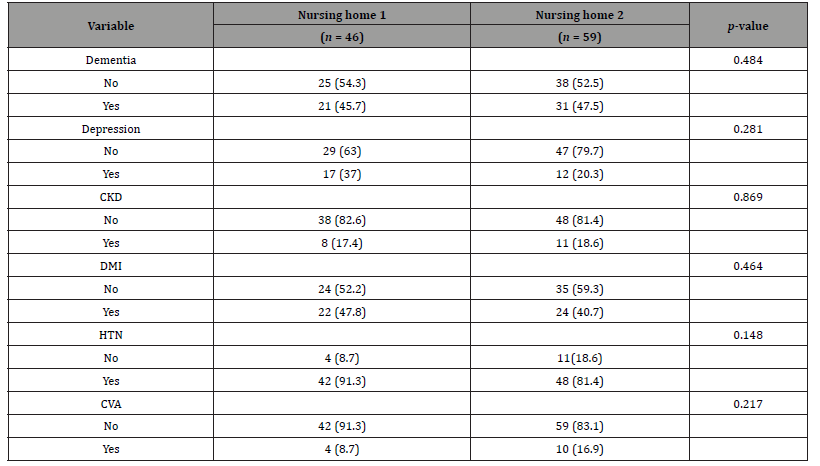
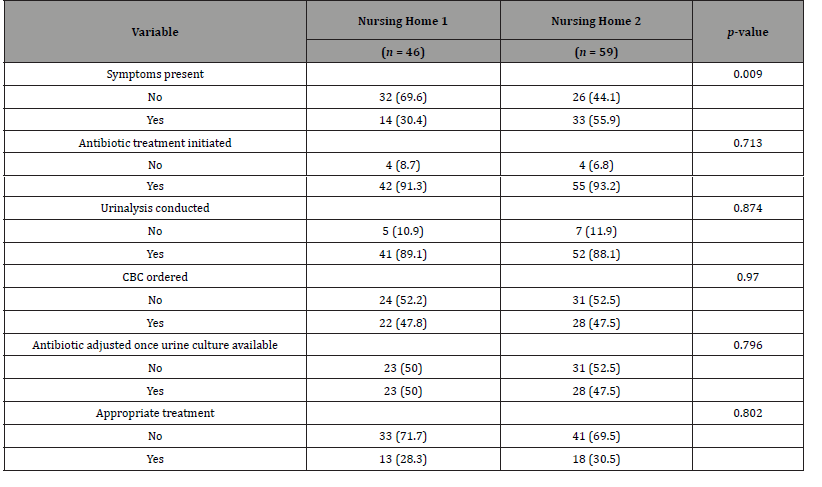
Table 5:Patient Symptoms, Testing, Treatment Disaggregated by Nursing Home.
Discussion of Results
Of the 105 patients across both nursing homes, 47 (44.8%) patients exhibited symptoms, 93 (88.5%) patients had a urinalysis obtained, 85 (81%) had positive preliminary urinalysis, and 59 (56.2%) eventually had positive results of urine cultures. Only 32 (30.47%) met the McGeer criteria for appropriate antibiotic treatment based on the chart review; however, antibiotic treatment was initiated in 97 (92.3%) of the patients. Twenty-nine (90.6%) of the patients who met the McGeer criteria received antibiotic treatment. Of the 73 (69.5%) patients who did not meet the McGeer criteria, antibiotic treatment was used with 68 (93.2%).
In examining the 97 patients who were given antibiotics, 44 (45.4%) showed symptoms, 80 (82.5%) had positive urinalysis (Note: only 93 of the patients who received antibiotic treatment had a urinalysis conducted), and 56 (57.7%) eventually had positive results of urine cultures. CBC testing was conducted on 50 (47.6%) of the patients. The chi-square test for independence indicated no significant association between urinary incontinence and positive urine culture. After receiving the urine culture report, only 51 (48.6%) residents’ antibiotic prescriptions were adjusted appropriately. In sum, only 31 (29.5%) residents received appropriate treatment and 74 (70.5%) of all the residents (n = 105) received inappropriate treatment by the study criteria established.
Nursing Home 1
Within Nursing Home 1, 46 patients were started on antibiotics for presumed UTI. Of the 46 patients whose charts were reviewed, 14 (30.4%) exhibited symptoms and 13 (28.3%) met the McGreer criteria. However, antibiotic treatment was initiated with 42 (91.3%). Therefore, 28 (66.7%) patients received antibiotic treatment without symptoms and 29 (69%) patients received antibiotic treatment without meeting the McGreer criteria.
Of all 46 patients whose charts were reviewed, CBC testing was conducted on 22 (47.8%) and urinalysis was conducted on 41 (89.1%) patients. Thirty-five (76.1%) patients had positive urinalysis results and 23 (50%) had positive cultures. Twentythree (50%) patients’ antibiotics were adjusted once the urine culture reports were available. Within Nursing Home 1, 33 (71.7%) of the 46 patients received inappropriate treatment according to the criteria established.
Nursing Home 2
Results were similar in Nursing Home 2, where 33 (55.9%) patients exhibited symptoms and 19 (32.2%) met the McGreer criteria; however, antibiotic treatment was initiated with 55 (93.2%) of the patients. Therefore, 22 (40%) received antibiotic treatment without symptoms and 36 (65.45%) received antibiotic treatment without meeting the McGreer criteria.
Of all 59 patients whose charts were reviewed, CBC testing was conducted with 28 (47.5%) and urinalysis was conducted with 52 (88.1%) patients. Fifty (84.7%) of the patients had positive preliminary reports; however, only 36 (61%) patients had positive urine cultures. Twenty-eight (47.5%%) patients’ antibiotics were adjusted once their urine cultures were available. In sum, within Nursing Home 2, 41 (69.5%) of the 59 patients received inappropriate treatment according to the criteria established. The only difference between the two Nursing Homes was that a larger proportion of patients in Nursing Home 2 exhibited symptoms (see Table 3; p = .009).
Comparisons of Patients’ Symptoms, Testing, and Treatment between Nursing Home 1 and Nursing Home 2
Table 5 demonstrates the patients’ symptoms, testing, and treatment for UTI in Nursing Homes 1 and 2. The Chi-square test of independence demonstrated that patients’ testing and treatment across the two nursing homes was similar. For chi-square analyses, the assumption that cell frequencies would be greater than five was met for all but one variable (antibiotic treatment initiated); therefore, the findings that included the variable of antibiotic treatment initiated should be interpreted with caution. The only difference between the two Nursing Homes was that a larger proportion of patients in Nursing Home 2 exhibited symptoms (see Table 3; p = .009).
Surprisingly, none of the patient characteristics (age, gender, ethnicity, cognitive status, functional status, and diagnosis) were correlated with inappropriate or appropriate initiation of antibiotics. There was no significant association between being urinary incontinent and positive urine culture. Further, none of the patient characteristics individually explained the classification of inappropriate or appropriate initiation of antibiotic treatment. This study shows that patient characteristics may not have influenced decisions about the initiation of antibiotic treatment or its appropriateness.
Summary of Findings
A retrospective chart review in two nursing homes in Central California was conducted to determine the appropriate use of treatment of UTIs. The inclusion criteria were any patient started on antibiotics for presumed UTI. The exclusion criteria were indwelling Foley catheters, and hospice services. The data were collected based on the McGeer criteria. The chi-square test of independence was used to analyze the data. A total of 105 patients across both nursing homes was studied. Only 32 patients met the McGeer criteria for appropriate antibiotic treatment. However, antibiotics were prescribed to 97 patients. The study showed that the providers failed to appropriately prescribe antibiotics based on urine culture reports. The study also showed that the providers did not make appropriate changes to the treatment once urine culture and sensitivity reports were available (such as discontinue antibiotic if culture is negative or change antibiotic if it is resistant to the bacteria).
Implications for Practice
There are clear opportunities to improve prescribing habits when initiating treatment for UTI. To change old prescribing habits is a difficult task and implementing change has always been challenging for any organization. In today’s complex healthcare system, providers are expected to stay current with the guidelines to provide care using evidence-based practice. As with any new change, providers can resist new guidelines, yet their “buy-in” is vital for smooth implementation [7]. The time has come to better prepare for the ever-changing healthcare industry. The following steps should be taken to minimize the unnecessary use of antibiotics:
• Signs and symptoms of UTI should be documented before antibiotic is initiated or urinalysis is ordered.
• A facility infection control committee should establish the use of approved criteria for standard of care.
• Every effort should be made to obtain the clean catch to avoid a contaminated sample and possibly unnecessary antibiotics.
• Director of Nursing and the Director of Staff Development should provide ongoing in-services to staff regarding educating the patient, family members, and reporting appropriate signs and symptoms to the providers.
• Once the urine culture report comes back, providers should appropriately make medication changes as indicated.
• Every effort should be made to minimize empiric treatment, such as increasing hydration, urinary analgesics, etc.
Limitations
Not all nurses completed the progress notes with equal accuracy. It is possible that patients could have been experiencing the signs and symptoms of UTIs, which would prompt the collection of the urine sample; however, such information was not documented in the medical records. Unknown in this study were the origins of clean catches (voided urine samples, bedpans, hat placed in the toilet, or wet briefs). This indicates that the urinalysis could have been performed on a contaminated urine sample. The McGeer’s criteria are excellent for patients who can express their needs; however, they do not provide information for dementia or confused patients with lower BIMS. This was a limitation. One could not generalize the results of this study to the entire population of LTCFs because this study was conducted in only two nursing homes under one corporation in one city. The medical records may have been subject to bias based on characteristics associated with the recorder corporation culture and purpose of the chart.
Recommendations for Research
Future studies should examine more closely whether inappropriate antibiotics prescriptions are discipline-specific (MDs, DOs, NPs, and PAs). Future investigations should include a qualitative study (e.g., case study) that examines provider perceptions about barriers to effectively treat asymptomatic UTIs, which may provide insight into interventions that could increase compliance with antibiotic stewardship.
Conclusions
Despite the introduction of antibiotic stewardship in the nursing homes, antibiotics remain the first line of treatment for suspected UTIs. This study found a substantial disparity between the antibiotic stewardship and providers’ diagnoses of UTIs. About 70% of residents received antibiotics for asymptomatic UTIs in both nursing homes. It is important to not prescribe antibiotics for asymptomatic UTIs because doing so may cause more harm, side effects, Clostridium difficile infection, and development of antimicrobial resistance [4].
Conflict of Interest
None.
Financial support
None.
References
- Genao L and Buhr GT (2012) Urinary tract infections in older adults residing in long-term care facilities. The Annals of Long-Term Care: JAMDA 20(4): 33-38.
- Rotjanapan P, Dosa D and Thomas K (2011) Potentially inappropriate treatment of urinary tract infections in two Rhode Island nursing homes. Arch Intern Med. 2011;171(5): 438-453.
- (2015) Center for Medicare and Medicaid Services. Nursing home data compendium.
- Monette J, Miller MA, Monette M, Laurier C, Boivin JF, et al. (2007) Effect of an educational intervention on optimizing antibiotic prescribing in long-term care facilities. Journal of American Geriatrics Society 55(8): 1231-1235.
- (2018) California Department of Public Health. Infection Surveillance in Skilled Nursing Facilities. California Department of Public Health.
- Warner RM (2013) Applied statistics: From bivariate through multivariate techniques.
- Bozak MG (2003) Using Lewin’s force field analysis in implementing a nursing information system. Comput Inform Nurs 21(2): 80-85.
-
Harkirat S Bal. Exploring the Treatment of Noncatheterized Urinary Tract Infections in Nursing Home Patients. Glob J Aging Geriatr Res. 1(4): 2021. GJAGR.MS.ID.000516.
-
Biogerontology; DNA Repair; Epigenetic; Genetics Factors
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






