 Research Article
Research Article
Virtual Versus Face-To-Face Neuropsychological Assessment: A Pilot Study Towards Its Benefits and Its Limitations
María Josefina Gonzalez Aguilar* and Lucía Daniela Leguizamón
Facultad de Ciencias Biomédicas, Universidad Austral, Argentina
María Josefina Gonzalez Aguilar, Facultad de Ciencias Biomédicas, Universidad Austral, Argentina
Received Date:October 19, 2021; Published Date:October 28, 2021
Abstract
During the COVID-19 pandemic many people – especially older adults – had drastically decreased their visits to health centers, causing a new concern among the professionals: if these patients were not assisting physically to their doctors, who is watching over their health, diagnosis, and follow-ups? Novel cognitive and emotional concerns are frequent in older adults and must be seen by a specialist who can determine whether these complaints may be compatible with a neurologic or psychiatric disorder. In this context, during the pandemic telemedicine services had been replacing and compensating some of these demands. Teleneuropsychology (TNP) is the application of virtual methods with neuropsychological aims, to assess or treat patients with suspected of confirmed cognitive impairment. Several studies from around the world are showing TNP and face-to-face (FTF) assessments are similar, and TNP approaches may be reliable and accurate, but this type of data is scarce in the Latin America region.
The objective of this pilot study is to analyze the differences in TNP and FTF assessments, and to describe the pros and cons reported by the participants. For this purpose, 20 healthy adults were assessed in 2 instances (virtual and physical meeting) with a selection of classic neuropsychological tasks. After their last session, they answered an ad-hoc survey reporting the main benefits and concerns regarding both approaches. The results of this study show that no significant differences were found between TNP and FTF performance. The main benefits reported from the FTF session were the real-time interaction and feedback, while the main benefits reported from the TNP session were the flexibility, comfort, and the travel-time they saved. In the other hand, the main concerns reported from the FTF session were that it was more time-consuming and less flexible to arrange the session, while the main concerns with the TNP session were associated to technological potential problems and the lack of a direct eye contact. In conclusion, this study is aligned with previous research and provides empirical local evidence of the usefulness of virtual approaches in health-related services.
Keywords:Telemedicine; Teleneuropsychology; Neuropsychological assessment; COVID-19
Abbreviations:TNP = Teleneuropsychology. FFT = Face-to-face.
Introduction
The use of telemedicine to distribute medical services regardless the location is not new, but due to the COVID-19 pandemic and the consecutive lockdown measures, the offer of this type of assistance has grown rapidly. The health emergency policies required that most of the people (especially older adults) had to stay at home and avoid face-to-face (FTF) contact with others, including medical centers and health professionals. These circumstances led to veer from a physical contact to a virtual contact with family, friends, work colleagues and health professionals, making telemedicine not only just an alternative but a mandatory way to assess and follow the patients [1,2]. Telemedicine is a tool originally created as a way to help people living in geographically isolated areas, offering the possibility to connect this people with specialized health professionals without the limitations of transport and time consumption [3]. In this way, its benefits were mainly the reduction of the economic cost, a reduced loss in time and the access to health services no matter the physical location [4]. Specifically, teleneuropsychology (TNP) is the application of telemedicine methods for neuropsychological objectives of patients with suspected of confirmed cognitive damage. Thus, TNP is known for the use of audiovisual tools to carry out neuropsychological assessments and treatments [5].
Since the beginning of the COVID-19 pandemic, most countries adopted restrictive measures that promoted to stay at home and avoid non-urgent visits to health centers. An Argentinian study [6] compared the outpatient visits to one of the most renowned neurological centers in the country during the first weeks of the 2020 lockdown and the same period during 2019, and the results were drastic: diagnostic tests dropped a 60% and the cognitive neurology area suffered a 66% drop in patients visits. While severe neurological cases still assisted to health centers, patients with minor complaints stayed at home and avoided the hospital. These results replicated in many parts of the world [7-9]. These patients with apparent minor complaints (e.g., cognitive, or emotional complaints) may represent an at-risk group that was not assessed and treated at an opportune time. Older adults are a particularly affected group due to the pandemic: not only they were the first who should not get infected with the COVID-19 virus but also, they lacked medical assistance for these suspected minor complaints, such as novel cognitive failures or higher levels of depression, anxiety, and isolation [10-11]. In this context, telemedicine in general (and TNP in particular) has become a critical tool to aid and provide a follow-up assistance to these vulnerable groups [12-14].
Although TNP is a relatively new area which is quickly developing, several studies had shown this approach may be reliable to produce valid neuropsychological assessments [15-21]. A recent systematic review analyzed the reliability of traditionally FTF neuropsychological assessment used in a telemedicine context with Alzheimer’s Disease patients [22], concluding that widely used screening tools and other neuropsychological tests resulted in general reliability and enough accuracy. In this way, this study affirms that performing virtual assessments is accepted and appreciated by patients and their families, and therefore may be useful to provide a personalized follow-up in the treatment of cognitive disorders. Another recent study [23] analyzed the acceptance and concerns associated to TNP assessment, concluding that this approach is satisfactory, especially during the COVID-19 pandemic while limitations should be addressed, as technological concerns may arise.
Although there is valuable information that supports TNP as a trustworthy method to assess people in a virtual mode, evidence of these type of studies is scarce in Latin America. In this context, the objective of this study is to analyze preliminary results of the similarities and differences between TNP and FTF neuropsychological assessments, as well as address the benefits and limitations perceived by the participants.
Methods
A pilot study with 20 healthy young adults (age X= 28.2; SD= 5.18 / educational level in years X=16.1; SD=2.92; 80% female) was carried out to analyze the differences between TNP and FTF neuropsychological assessment, as part of a first step before assessing older adults with these same procedures. The selected neuropsychological tests for this study were the Signoret battery for mnesic efficiency (serial and logical episodic memory subtests), the digit span test (forward and backwards), the Boston naming test (short version of 12 stimuli), verbal fluencies (semantic and phonological tasks) and the matrix reasoning subtest of the WAIS IV. The participants were assessed in both ways (FTF and TNP) in a random order (10 participants started with TNP and then FTF, and the other 10 participants started with the FTF session and did the TNP session afterwards), to avoid a correlation between the performance and the order of administration of the tests. Participants were assessed with at least 5 weeks of difference, to minimize memory effects in the selected tasks. To analyze the benefits and concerns informed by the participants, an ad-hoc survey was conducted after their second session, where they were openly asked which were the pros and cons, they perceived in both type of meetings (FTF and TNP). In this adhoc survey, participants were asked what they liked most about the TNP and FTF session, and what were their main concerns or discomforts associated with both type of sessions. A descriptive and qualitative analysis was done to study their answers. To analyze the differences between FTF and TNP in neuropsychological performance a dependent sample Student t-test was conducted, and differences were considered statistically different with a p value < .05.
Results
As Table 1 shows, no statistically significant differences (p>.05) were found in the performance of the selected neuropsychological tests between the virtual (TNP) and traditional (FTF) neuropsychological assessment in the present sample.
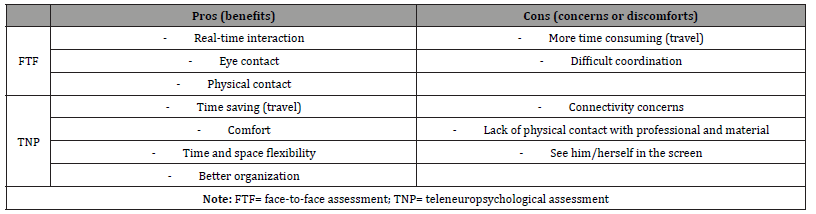
The Table 2 summarizes the descriptive and qualitative analysis of the ad-hoc survey done after the last session. This preliminary analysis revealed that participants liked the FTF session because they could interact with the professional in a real-time situation, without delays or audio problems. They also highlighted that real eye contact and having the possibility of touching the material (e.g., the visual stimuli, booklets, etc.) felt beneficial for their performance. In the other hand, participants reported that the FTF session was far more time consuming, informing concerns about time, traffic, or transport problems, and that coordinating the time of the session were both parts could physically assist was more difficult. Moreover, the participants reported that the benefits of the TNP session were that presented more flexibility in terms of time to schedule the meeting, they may organize better to assist to the assessment and continue with their daily activities. Also, they reported that they could do it from the comfort of their homes, saving time associated with travel. In terms of their main worries regarding TNP, they reported potential connectivity concerns (e.g., being alert of their Wi-Fi connection), the lack of physical eye-contact with the professional and the possibility to touch the materials, and the added stress of seeing themselves in the screen.
Table 1:Difference analysis between FTF and TNP sessions in the neuropsychological assessment.
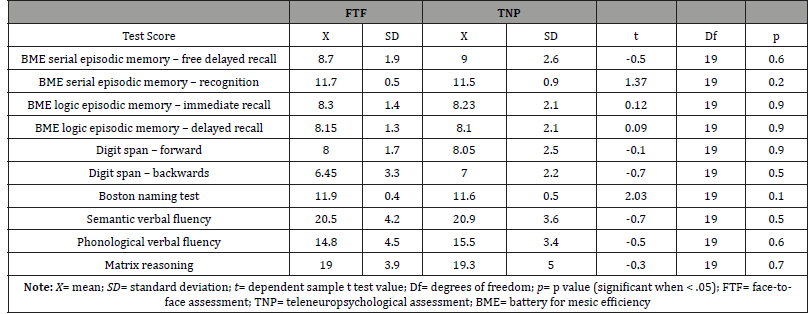
Table 2:Summary of the pros and cons perceived by the participants with the ad-hoc survey.
Discussion and Conclusion
This preliminary pilot study shows that a TNP approach may be as reliable as a FTF approach, allowing access to health-related services (such as a neurocognitive assessment) to people that cannot physically reach a specialist, or prefer to be assessed by a particular specialist who is not in their hometown. These conclusions are aligned with previous findings [15-21]. During the last two years, telemedicine services expanded their frontiers rapidly due to the COVID-19 pandemic and the associated restrictions, to give an answer to patients who could not physically assist to a health center [3,4,12-14]. Future studies should address and profoundly analyze the concerns reported by the participants associated to virtual health sessions, as the conclusions of the present study are in line with previous research in other countries [23]. It seems that virtual approaches for educational, social and health reasons had come to stay [1], and TNP appears to be part of this upcoming technological era.
Acknowledgments:
None.
Conflict of interest:
None.
References
- Gonzalez Aguilar MJ (2021) Neuropsychological Assessment in Times of Social Distancing: What Can Telemedicine Offer to Older Adults? Glob J Aging Geriatr Res 1(4): 1-4.
- Adams JL, Myers TL, Waddell EM, Spear KL, Schneider RB (2020) Telemedicine: A valuable tool in neurodegenerative diseases. Current geriatrics reports 9(2): 72-81.
- Tachakra S, Lynch M, Newson R, Stinson A, Sivakumar (2000) A comparison of telemedicine with face-to-face consultations for trauma management. Journal of telemedicine and telecare 6(1): 178-181.
- Kosterink SM, Huis int Veld RMHA, Cagnie B, Hasenbring M, Vollenbroek Hutten MMR (2010) The clinical effectiveness of a myofeedback-based teletreatment service in patients with non-specific neck and shoulder pain: a randomized controlled trial. Journal of Telemedicine and Telecare 16(6): 316-321.
- Bilder RM, Postal KS, Barisa M, Aase DM, Cullum CM, et al. (2020) Inter Organizational Practice Committee recommendations/guidance for teleneuropsychology in response to the COVID-19 pandemic. Archives of Clinical Neuropsychology: The Official Journal of the National Academy of Neuropsychologists 35(6): 647-659.
- Calandri IL, Hawkes MA, Marrodan M, Ameriso SF, Correale J, et al. (2020) The impact of an early strict nationwide lockdown on the pattern of consultation for neurological diseases. Journal of the Neurological Sciences 418: 117084.
- Tam CCF, Cheung KS, Lam S, Wong A, Yung A, et al. (2020) Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 13(4): e006631.
- Cohen B and Shaw D (2020) Cardiac Arrest Deaths at Home in New York City. Have Increased by a Startling 800%.
- Krumholz HM (2020) Where have all the heart attacks gone? New York Times.
- Krendl AC and Perry BL (2021) The Impact of Sheltering in Place During the COVID-19 Pandemic on Older Adults’ Social and Mental Well-Being. The Journals of Gerontology: Series B 76(2): 53-58.
- Killgore WDS, Cloonan SA, Taylor EC, Dailey NS (2020) Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry research 290: 113-117.
- Allegri R and Sevlever G (2020) Invited commentary: the elusive paradox: the woods behind the trees. Neurology Blogs.
- Hatcher Martin JM, Adams JL, Anderson ER, Bove R, Burrus TM, et al. (2020) Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology 94: 30-38.
- Moo LR, Gately ME, Jafri Z, Shirk SD (2020) Home-Based Video Telemedicine for Dementia Management. Clin. Gerontol 43: 193-203.
- Ciemins EL, Holloway B, Coon PJ, McClosky Armstrong T, Min SJ (2009) Telemedicine and the mini-mental state examination: Assessment from a distance. Telemedicine Journal and E-Health: The Official Journal of the American Telemedicine Association 15(5): 476-478.
- DeYoung N and Shenal BV (2019) The reliability of the Montreal Cognitive Assessment using telehealth in a rural setting with veterans. Journal of Telemedicine and Telecare 25(4): 197-203.
- Galusha Glasscock JM, Horton DK, Weiner MF, Cullum CM (2015) Video teleconference administration of the Repeatable Battery for the assessment of Neuropsychological Status. Archives of Clinical Neuropsychology: The Official Journal of the National Academy of Neuropsychologists 31(1): 8-11.
- McEachern W, Kirk A, Morgan DG, Crossley M, Henry C (2008) Reliability of the MMSE administered in-person and by telehealth. The Canadian Journal of Neurological Sciences. Le Journal Canadien Des Sciences Neurologiques 35(5): 643-646.
- Menon AS, Kondapavalru P, Krishna P, Chrismer JB, Raskin A, et al. (2001) Evaluation of a portable low cost videophone system in the assessment of depressive symptoms and cognitive function in elderly medically ill veterans. The Journal of Nervous and Mental Disease 189(6): 399-401.
- Turkstra LS, Quinn Padron M, Johnson JE, Workinger MS, Antoniotti N (2012) In-person versus telehealth assessment of discourse ability in adults with traumatic brain injury. The Journal of Head Trauma Rehabilitation 27(6): 424-432.
- Vahia IV, Ng B, Camacho A, Cardenas V, Cherner M et al. (2015) Telepsychiatry for neurocognitive testing in older rural Latino adults. The American journal of geriatric psychiatry: official journal of the American Association for Geriatric Psychiatry, 23(7): 666-670.
- Carotenuto A, Traini E, Fasanaro AM, Battineni G, Amenta F (2021) Tele-Neuropsychological Assessment of Alzheimer’s Disease. Journal of Personalized Medicine 11(8): 688.
- Parsons MW, Gardner MM, Sherman JC, Pasquariello K, Grieco JA, et al. (2021) Feasibility and acceptance of direct-to-gome tele-neuropsychology services during the COVID-19 pandemic. Journal of the International Neuropsychological Society 6: 1-6.
-
María Josefina Gonzalez Aguilar, Lucía Daniela Leguizamón. Virtual Versus Face-To-Face Neuropsychological Assessment: A Pilot Study Towards Its Benefits and Its Limitations. Glob J Aging Geriatr Res. 1(4): 2021. GJAGR.MS.ID.000520.
-
Telemedicine; Tele neuropsychology; Neuropsychological assessment; COVID-19.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






