 Research Article
Research Article
Risk Factors for Falls and Fear of Falling Among Older Patients with Cancer
Kuang-Yi Wen*, Kristine Swartz, Tingting Zhan and Andrew Chapman
Division of Population Science, Department of Medical Oncology Sidney Kimmel Cancer Center, Thomas Jefferson University, USA
Kuang-Yi Wen, Division of Population Science, Department of Medical Oncology Sidney Kimmel Cancer Center, Thomas Jefferson University, USA
Received Date:March 19, 2024; Published Date:March 25, 2024
Abstract
Introduction: Cancer is a disease of the elderly with more than 60% of all cancers diagnosed in adults aged 60 or older. Falls pose a substantial
risk for older cancer patients leading to hip fractures, traumatic brain injury, and are the leading cause of injury-related hospitalizations in persons
aged 60 and older. This risk is due to aging changes compounded by the effect of cancer and cancer therapy. This report aims at understanding risk
factors for falls and the perception of fear of falling (FOF) among older patients with cancer.
Methods: As a single-site, retrospective cohort study, data was derived from 250 geriatric oncology patients from Senior Adult Oncology Center
at Jefferson Health. The primary endpoints are the number of falls in the preceding 12 months and FOF as part of a self-reported fall screening.
Multivariate logistic regression model was used to identify the independent risks factors by including patients’ age, sex, race/ethnicity, BMI,
polypharmacy, cancer types, ECOG scores, timed up and go (TUG) test, ADL, IADL, Mini-Cog, and Geriatric Depression Scale (GDS) for each endpoint
separately.
Results: The majority were white (63.65%), females (60%) with a mean age of age 77.6. The most common cancer diagnosis was hematologic
malignancies (41.0%). TUG was abnormal in 89 patients (43.2%), impaired Mini-Cog in 52 (22.7%) patients, Impaired ADL in 73 (30.2%) patients,
Impaired IADL in 134 (55.4%) patients. Polypharmacy was positive in 245 patients. 64 (32.0%) had moderate to severe depression by GDS. We have
found that the risk of FOF is higher in patients with abnormal TUG scores (OR= 5.88, 95% CI =2.87 ~ 12.62, p=0.00). The risk of falling was increased
in abnormal ADL group (OR= 2.75, 95% CI = 1.51-5.02, p = 0.001).
Conclusion: We have found that among patients aged 65 and older FOF was related to abnormal TUG scores and the risk of falling was increased
in abnormal ADL group. Further implementation of systematic screening is crucial in fall prevention and our results suggest the TUG and ADL should
be used in an initial screening modality for elderly cancer patient as well as subsequent treatment visits due to the rapidly devolving functional
status from cancer treatments.
Introduction
Falls are common in older adults and a leading cause of injury, injury-related disability, and injury-related death [1,2]. The incidence of falls among adults aged 65 and older is estimated to be around 28%-35% [3,4]. About 50% of falls result in injury, and 10%-11% result in major injuries, including fractures. Other complications include the loss of mobility in part through fear of falling, admission to long-term care facility, and depression [5]. Among the risk factors of falls is the history of falling, gait or balance abnormalities and medical conditions or medication side effects of polypharmacy or use medication in general [6,7]. other factors as tripping hazards, inadequate lighting, or the absence or improper use of assistive devices [8]. Fear of falling (FOF) on its own is concerning as it can lead to less physical activity, avoidance of activities, depression, decreased social contact and lower quality of life which impact both physical and mental health and an increased risk of future falls [9].
Falls occur in cancer patients due to the complexities of the disease and its treatment [10] and are more common in older adults with cancer than community dwelling older adults [10]. It is an underreported phenomenon as only one out of 10 self-reported recent falls by older patients with cancer are appropriately documented in the health care records [11]. Current evidence shows that a history of falls, white race [12] and ADL status [13] are the most commonly identified risk factors of falls among older adults with cancer. This could be due to chemotherapy induced peripheral neuropathy (CIPN) [14] and correlates with increasing numbers of chemotherapy cycles and certain chemotherapeutic agents like taxanes, platinum based chemotherapeutic agents and vinca alkaloids [13,15]. Other associated functional declines that complicate the risk of falls can coexist as balance deficits, lower limb strength impairments and an increased falling frequency [16-18]. Additionally, increased fall risk may lead to FOF, which reportedly affects more than half of patients with CIPN [19]. Worse function, greater disability, and higher numbers of falls as well as symptoms of CIPN last for several years after chemotherapy [20]. These data indicate the patients receiving commonly used chemotherapy agents present with FOF in addition to the symptom of CIPN during and after treatment and patients were likely to restrict their activities to prevent falling even when injuries do not occur. The purpose of this article is to provide a better understanding of risk factors of falls and FOF among elderly cancer patients sampled from the Senior Adult Oncology Center (SAOC) at Jefferson Health.
Methods
Sample: This study was approved by the Institutional Review Board of Thomas Jefferson University. This is a retrospective cohort study; data was derived from 250 geriatric oncology patients from the SAOC at Jefferson Health. Each patient undergoes a comprehensive geriatric assessment that entails assessments from a geriatrician, oncologist, pharmacist, social worker and a dietician.
Measures: The Geriatric Depression Scale (GDS) is a validated screening instrument for depression in older cancer patients (cite). The total items score ranges from 0-15 with higher scores indicating greater severity depression. A cut of 5 was used for this study with 0-5 and above 5 standing for “no to mild” and “moderate to severe” depression [21].
Minicog: The Mini-Cog is a simple, effective, easily administered screening tool that can uncover cognitive impairment in its earliest stages. Scores were categorized as normal (more than or equal 3) or abnormal (less than 3) [22]. Activities of daily living (ADL) [23] assesses basic self-care functions the items used are bathing and showering, dressing, transferring, feeding, toileting. Instrumental Activities of Daily Living (IADL) [23] is measuring functional status that is most early affected by mild cognitive disorders (use of telephone, shopping, food preparation, housekeeping or handiwork, laundry, medication administration and managing finances).
A subject was considered as dependent (on ADL or IADL) if he/ she could not perform at least one activity of the scale without a given level of assistance, as defined by the authors of the scale. Each item was measured on the following scale (Independent, needs assistance or Independent) based on the OARS multidimensional functional assessment questionnaire. ADLs only include selfreported mobility items and the ASCO recommends adding objective measures to assess physical function during CGA in older cancer patients. Thus, we also include Timed up and go (TUG) [24] a screening test that is a sensitive and specific measure of probability for falls among older adults. Cut of values used considered the TUG normal if completed in less than or equal to 10 seconds and abnormal more than 10 seconds.
Polypharmacy was defined as more than five medications prescribed. The primary endpoints are the number of falls in the preceding 12 months and FOF as part of a self-reported fall screening. Falls screening: as part of the geriatric assessment at SAOC, patients are screened for falls as follows “Do you worry about falling? Have you fallen at any time in the past 12 months?” The output of these two screening questions were used as the endpoints in the outcome analysis.
Data Analysis
Descriptive statistics included socio-demographic information, cancer diagnosis by site results is summarized as means (M), standard deviation (SD) and ranges (R). The analysis for fear of falls is based on 180 subjects and for falls for 240 subjects by fitting a multivariable logistic model using R. Backward stepwise variable selection for the multivariable model by Akaike information criterion (AIC) is performed using R package MASS. Multivariate logistic regression model included the following variables age, sex, race/ethnicity, BMI, polypharmacy, cancer types, ECOG scores, Timed up and go (TUG) test, GDS scores, Mini-Cog, for each endpoint separately. The results are expressed in terms of the odds ratio including 95% confidence intervals.
Results
The characteristics of the patients are shown in (Table 1). The cohort constituted 242 cancer patients with a mean age of 77.6 (805), the majority were white (63.65%), and female 60%. The most common cancer diagnosis were hematologic malignancies (41.0%), breast (19%) genitourinary (13%), lung (12.5%), gastrointestinal (12%). Mean BMI was 27.7 (5.9), ECOG ranged from 0-3, with 66 (28.3%) had an ECOG of 2 or 3. Concerning functional status 73 (30.2%) patients had impaired ADL, and 134 (55.4%) had impaired IADL. Impaired mobility according to TUG in 89 patients (43.2%) patients. Impaired Minicog in 52 (22.7%) patients. 64 (32%) patients reported moderate and severe depression according to the GDS scores. Prior fall 65/249 (26.1%) % and FOF 65/235 (28.9%) were reported in our sample.
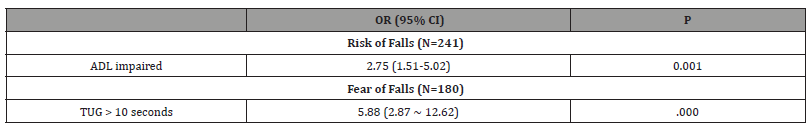
Results from multivariable logistic regression analyses conducted separately for falls/no falls in prior 12 months and FOF are in table 2 as OR with 95% confidence intervals (CI)., controlling for age, race, BMI, cancer type, ECOG and including ADL, IADL, TUG, Minicog, GDS, and polypharmacy as predictors. (See Table 2). The likelihood of falling was increased in abnormal ADL group (OR= 11.45, 95% CI = 2.62-63.81, p=0.003). We have found that likelihood of having FOF is higher in patients with abnormal TUG scores (OR= 6.1, 95% Ci =2.97-13.04, p=0.00).
Table 1:Demographic and characteristics.
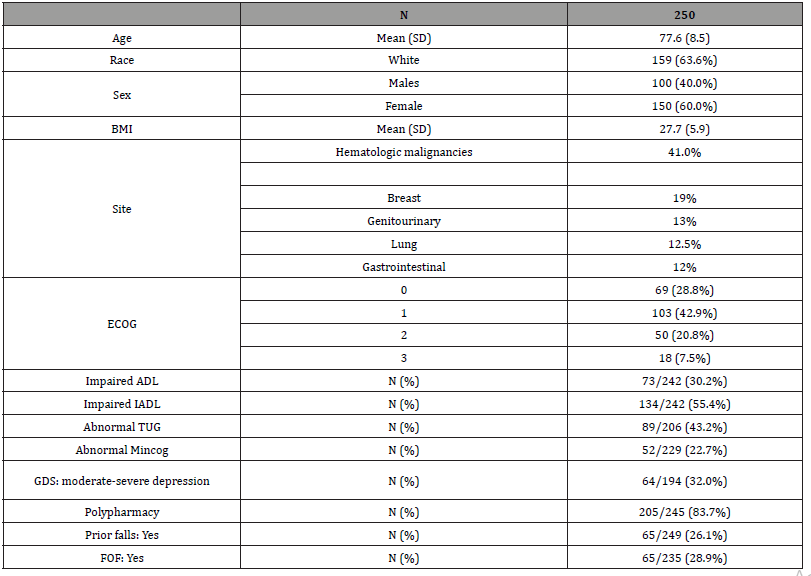
Table 2:Results for multivariable logistic regression for falls and FOF.
Discussion
The majority of cancer diagnoses and morbidity occurs in patients aged 65 and over, elderly patients are an understudied population that is projected to significantly increase over the next 20 years [25]. Falls are preventable [10] and risk factors can be mitigated in this report we aimed to identify the risk factors for falls and the perceived FOF for patients of the senior adult oncology center at Jefferson health. Our data show that 26% of our sample had at least one prior fall and 28.9% reported FOF, similar to the prevalence of falls and FOF in community-dwelling older adults [3,4]. We have also found that in our older cancer patient sample the odds of falling were associated with abnormal ADL and that abnormal TUG was associated with perceptions of FOF. Our results align with previous studies that show that dependence in ADL is associated with greater risk for falls for both elderly cancer and non-cancer populations, with estimates ranging from a 40% to nearly five-fold increased odds of falls [26-28]. FOF can lead to reduced balance performance, limited activity levels, restricted social participation and compromised quality of life [29]. Multiple strategies have been used to address FOF; a systematic review report that exercise interventions associated with small-to-moderate reduction in FOF at end of treatment in analysis of 24 trials with 1,692 non oncology adults; future research should examine the potential adaptation of such exercise interventions for older cancer patients to minimize FOF and improve activity levels.
Older patients with cancer can have their functional status deteriorating either due to progression of disease and/or concurrent effects of cancer treatment. This deterioration is rapidly dynamic; one in five older patients develop new impairments in their ADL between the first and second cycles of chemotherapy [30]. Studies show that cancer patients receiving either taxanes or platinum agents are more likely to experience at least one fall during chemotherapy [13,15]. Falls were associated with increased chemotherapy cycle number, CIPN, and muscle weakness, as well as loss of balance [13,14]. These results are consistent with other studies that reported diminished physical function, including muscle weakness and loss of balance, were predictive of falls in osteoporotic elderly cancer patients [20].
Higher TUG duration is associated with FOF which aligns with the general consensus that the TUG is very sensitive and specific for determining which individuals are at greater risk for falls. For cancer patients the results however vary from a study by Shabbir et. al. found that TUG predicted risk of falls for prostate cancer patients on androgen deprivation therapy [31]. On the other hand, Hoppe et al. in a study looking at elderly cancer patients found no significant association between TUG time and prospective falls for an elderly cancer population 70 years and above of age [30]. Generally according to the American Geriatrics Society fall prevention in community-dwelling older adults entails a multifactorial intervention that addresses multiple risk factors identified during the risk assessment and intervening using multiple modalities like exercise, environment modification, supplements and medication review among other modalities [32]. In an institutional setting multifactorial interventions may slightly reduce the number of falls overall but not the number of older adult inpatients who experience ≥ 1 fall in hospital, evidence however is limited, and it is unclear if this methodology applies to elderly cancer patients with their rapidly changing status during treatment. To our knowledge no such tailored guidelines exist in the literature as regards frequency of and types of assessments.
Tools specifically targeting falls in elderly cancer patients need to be utilized in a streamlined and methodological approach. Further implementation of systematic screening is crucial in fall prevention and our results suggest the TUG and ADL should be used in an initial screening modality for elderly cancer patient as well as subsequent treatment visits due to the rapidly devolving functional stats from subsequent cancer treatments. Thus, assessment and management of fall is of top priority due to the potential serious implications, disease trajectory and survival. Falls are preventable and risk factors can be mitigated through targeted interventions, like strength and balance exercises, medication review, and cognitive function [33]. Using proper assessments can help identify underlying causes and individuals at risk for falls.
Limitations
There are several limitations to our study. The falls are recalled retrospectively thus subject to recall bias. As mentioned previously, falls are generally underreported that leads to potential lower estimates. The sample is limited as the study is based on a single site and might have failed to significantly detect other factors like age, race and nutritional status as some other studies have reported an association with risk of falls. Our data did not include complete chemotherapeutic information or related adverse events limiting the ability for stratification by chemotherapeutic agents.
Conclusion
We have found FOF was related to abnormal TUG scores and the risk of falling was associated abnormal ADL. Our results suggest the TUG and ADL should be used in an initial screening modality for elderly cancer patients as well as subsequent treatment visits due to the rapidly devolving functional status from cancer treatments. Falls are preventable and risk factors can be mitigated through targeted interventions tackling multiple disciplines. Using proper assessments can help identify underlying causes and individuals at risk for falls.
Acknowledgement
This project was supported by NCI 1R21CA258200 and 5P30CA056036.
Conflict of Interest
No Conflict of Interest.
References
- Bergen G, Stevens MR, Burns ER (2016) Falls and Fall Injuries Among Adults Aged ≥65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep 65(37): 993-998.
- Close JC, Lord SR, Antonova E J, Martin M, Lensberg B, et al. (2012) Older people presenting to the emergency department after a fall: a population with substantial recurrent healthcare use. Emerg Med J 29(9): 742-747.
- Bolland MJ, Grey A, Reid IR (2016) Vitamin D supplements do not prevent falls. Bmj 353: i3005.
- Cigolle CT, Ha J, Min LC, Lee PG, Gure TR, et al. (2015) The epidemiologic data on falls, 1998-2010: more older Americans report falling. JAMA Intern Med 175(3): 443-445.
- Vieira ER, Palmer RC, Chaves PH (2016) Prevention of falls in older people living in the community. Bmj 353: i1419.
- Friedman JH (2009) Re: Practice parameter: assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 72(4): 382.
- Thurman DJ, Stevens JA, Rao JK (2008) Practice parameter: Assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 70(6): 473-479.
- Letts L, Moreland J, Richardson J, Coman L, Edwards M, et al. (2010) The physical environment as a fall risk factor in older adults: Systematic review and meta-analysis of cross-sectional and cohort studies. Aust Occup Ther J 57(1): 51-64.
- Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE, et al. (2008) Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing 37(1): 19-24.
- Wildes TM, Dua P, Fowler SA, Miller JP, Carpenter CR, et al. (2015) Systematic review of falls in older adults with cancer. Journal of Geriatric Oncology 6(1): 70-83.
- Guerard EJ, Deal AM, Williams GR, Jolly TA, Nyrop KA, et al. (2015) Falls in Older Adults With Cancer: Evaluation by Oncology Providers. Journal of Oncology Practice 11(6): 470-474.
- Sandra L Spoelstra, Barbara A Given, Debra L Schutte, Alla Sikorskii, Mei You, et al. (2013) Do older adults with cancer fall more often? A comparative analysis of falls in those with and without cancer. Oncol Nurs Forum 40(2): E69-E78.
- Cesari M, Landi F, Torre S, Onder G, Lattanzio F, et al. (2002) Prevalence and risk factors for falls in an older community-dwelling population. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 57(11): M722-M726.
- Tofthagen C, Overcash J, Kip K (2012) Falls in persons with chemotherapy-induced peripheral neuropathy. Supportive Care in Cancer 20(3): 583-589.
- Ward PR, Wong MD, Moore R, Naeim A (2014) Fall-related injuries in elderly cancer patients treated with neurotoxic chemotherapy: a retrospective cohort study. Journal of Geriatric Oncology 5(1): 57-64.
- Visovsky C (2006) Muscle strength, body composition, and physical activity in women receiving chemotherapy for breast cancer. Integrative cancer therapies,5(3): 183-191.
- Wampler MA, Topp KS, Miaskowski C, Byl NN, Rugo HS, et al. (2007) Quantitative and clinical description of postural instability in women with breast cancer treated with taxane chemotherapy. Archives of physical medicine and rehabilitation 88(8): 1002-1008.
- Winters-Stone KM, Nail L, Bennett JA, Schwartz A (2009) Bone Health and Falls: Fracture Risk in Breast Cancer Survivors With Chemotherapy-Induced Amenorrhea. Paper presented at the Oncology nursing forum. 36(3): 315-325.
- Yamamoto S, Fujikawa N, Asano K, Toki M, Takao A, et al. (2020) Assessment of fall-related self-efficacy: characteristics that influence the perception of patients with chemotherapy-induced peripheral neuropathy. Asia-Pacific journal of oncology nursing 7(2): 190-195.
- Winters-Stone KM, Horak F, Jacobs PG, Trubowitz P, Dieckmann NF, et al. (2017) Falls, Functioning, and Disability Among Women With Persistent Symptoms of Chemotherapy-Induced Peripheral Neuropathy. J Clin Oncol 35(23): 2604-2612.
- Stone LE, Granier K L, Segal DL (2019) Geriatric Depression Scale. D Gu, ME Dupre (Eds.), Encyclopedia of Gerontology and Population Aging pp: 1-8.
- Limpawattana P, Manjavong M (2021) The Mini-Cog, Clock Drawing Test, and Three-Item Recall Test: Rapid Cognitive Screening Tools with Comparable Performance in Detecting Mild NCD in Older Patients. Geriatrics (Basel) 6(3): 91.
- Edemekong PF, Bomgaars DL, Sukumaran S, Schoo C (2022) Activities of Daily Living. Encyclopedia of the Neurological Sciences: 47-48.
- Bohannon R W (2006) Reference Values for the Timed Up and Go Test: A Descriptive Meta-Analysis. Journal of Geriatric Physical Therapy 29(2): 64-68.
- Berger NA, Savvides P, Koroukian SM, Kahana EF, Deimling GT, et al. (2006) Cancer in the elderly. Trans Am Clin Climatol Assoc 117: 147-155; discussion: 155-146.
- Bylow K, Dale W, Mustian K, Stadler WM, Rodin M, et al. (2008) Falls and physical performance deficits in older patients with prostate cancer undergoing androgen deprivation therapy. Urology 72(2): 422-427.
- Overcash J (2007) Prediction of falls in older adults with cancer: a preliminary study 34(2): 341-346.
- Shumway-Cook A, Brauer S, Woollacott M (2000) Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical therapy 80(9): 896-903.
- Liu TW, Ng GYF, Chung RCK, Ng SSM (2018) Cognitive behavioural therapy for fear of falling and balance among older people: a systematic review and meta-analysis. Age and Ageing 47(4): 520-527.
- Hoppe S, Rainfray M, Fonck M, Hoppenreys L, Blanc JF, et al. (2013) Functional decline in older patients with cancer receiving first-line chemotherapy. Journal of Clinical Oncology 31(31): 3877-3882.
- Hussain S, Breunis H, Timilshina N, Alibhai SMH (2010) Falls in men on androgen deprivation therapy for prostate cancer. Journal of Geriatric Oncology 1(1): 32-39.
- (2011) Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 59(1): 148-157.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, et al. (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev (9): Cd007146.
-
Kuang-Yi Wen*, Kristine Swartz, Tingting Zhan and Andrew Chapman. Risk Factors for Falls and Fear of Falling Among Older Patients with Cancer. Glob J Aging Geriatr Res. 3(1): 2024. GJAGR.MS.ID.000553.
-
Comorbidity; Elderly; Prevalence.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






