 Research Article
Research Article
Public Views About Nutrition and Brain Health: A Survey of Older Adults in New Zealand
Yoram Barak1*, Hanafi Ahmad Damanhuri2 and Anna Rita Atti3
1Otago University Medical School, Department of Psychological Medicine, Dunedin, New Zealand
2Department of Biochemistry Faculty of Medicine, the National University of Malaysia, Kuala Lumpur, Malaysia
3Department of Biomedical and Neuromotor Sciences, University of Bologna, Italy
Yoram Barak, Otago University Medical School, Department of Psychological Medicine, Dunedin, New Zealand.
Received Date:February 01, 2024; Published Date:February 08, 2024
Abstract
Background: “Loss of memory” is a major concern for older adults. We evaluated nutrition and dementia awareness among New Zealand older
adults.
Methods: Telephone survey was completed with 1,005 respondents, mean age 64.02 years (range: 50-74), more women (n=518, 51.5%),
mostly European (n=921, 91.6%) and educated (n=347, 34.5%, university graduates or post-graduates). Respondents answered two open-ended
questions: ‘What do you believe are the 3 factors that will increase or decrease the chances of a person experiencing memory problem in older age?’
Results: The frequently cited risk factors were poor nutrition (27%) and alcohol abuse (23%). The frequently cited protective factor was
healthy nutrition (39.6%). Common misconceptions were underestimation of risk with less than 1% of participants recognizing diabetes, obesity, or
high serum cholesterol as risk factors for dementia.
Conclusions: Older adults are misinformed about the role of nutrition in brain health but do not underestimate its’ protective potential.
Keywords:Brain Health; Nutrition; Alcohol; Literacy
Introduction
In the coming decades dementia will become a global public health priority [1,2]. A prestigious report suggesting that major modifiable risk factors account for approximately 45% of all cases of Alzheimer’s disease (AD) led to calls for preventive action from national academies and scientific commissions recognizing the crucial impact of prevention in managing AD [3]. Public perceptions of the central nervous system, brain health, potential preventive health benefits, and psychosocial effects on diseases of the brain are little researched and understood. Knowledge and understanding of brain health remain low in many countries. Developing brain health literacy in the community, especially communicating knowledge about primary prevention is highly desirable. The media is a powerful mediator for communicating knowledge about brain health to the public. However, media portrayal of ageing and dementia is often imbalanced [4].
Beliefs about AD and scientific understanding of AD influence the perceived threat of AD in older adults. Education programs and interventions that nurture exposure to AD factual knowledge, particularly for those with limited education, can help reduce the negative public view of AD [5]. Moreover, data from the European Health Literacy Survey demonstrated increased odds of adopting healthy lifestyle associated with understanding disease prevention and health promotion information [6]. Public health policy makers should thus consider the findings that almost 1 in 2 Europeans had insufficient or problematic health literacy on a large recent survey and thus take measures to improve health literacy in order to accomplish positive behavioral change [7]. A report issued by the CDC and the Alzheimer’s Association [8] in the USA recommended with high significance to “determine how diverse audiences think about cognitive health and its association with lifestyle factors.”
Little is known about what drives older adults’ motivation to change their behavior. In a large and carefully designed public health campaign physical activity and healthy diet were identified more often as being protective against dementia [9,10]. The modified Lifestyle for Brain Health scale was developed by our group to quantify general public literacy of Brain Health [11]. Brain health was recently proposed as an overarching concept to describe measures to maintain a healthy brain, and this was further supplemented by the U.S. National Institute on Aging by stating that “brain health is all about making the most of your brain and helping reduce some risks to it as you age” [12].
Globally, reported rates of malnutrition in older adults are concerning [13]. In a New Zealand study, focusing on the prevalence of malnutrition risk in older people demonstrated that 1 in 5 older adults were malnourished. In the present study, we report on a survey aimed at gaining a comprehensive understanding of the views concerning effects of nutrition on brain health based on a representative New Zealand (NZ) sample of older adults.
Methods
This survey of public opinion on “Brain Health” presented participants with open-ended questions as to dementia risk and protective factors. This strategy embraced the AICR Cancer Risk Awareness Survey aimed at gauging awareness of lifestyle-related cancer risk factors [14]. We adapted a similar way of asking questions about the risk of dementia. Detailed description of our methodology is published in our survey in NZ [15,16].
Procedures
The National Research Bureau (www.nrb.co.nz) was employed to carry out a telephone survey. The National Research Bureau is an independent NZ research company. It has been contracted in the past by the NZ Ministry of Health to conduct nationwide health surveys [17,18]. The National Research Bureau Ltd is a member of ESOMAR; an international organization that advances ethics and effectiveness in gathering research, including social research.
Data were collected via telephone-administered interviews, conducted by trained interviewers. Each household was called up to four times, that is, an initial call, followed by three callbacks if unreachable, before replacing that household with another household. Callbacks were made on different days, and at different times of the day, to maximize the chance of contacting the eligible respondent. Response rate was 77%. All survey methods were performed in accordance with the university of Otago guidelines and regulations.
Sample
Our sampling frame was adults aged 50 to 74 years old. One thousand and three hundred households selected from the electoral role were contacted and asked to take part. The response rate was 68%, yielding a sample of 1,005 participants. The response rate is in line with using telephone interviews to reduce nonresponse bias [19]. The interviewing period was from November to December 2018. The sample size herein provides + 3.1% for estimated proportions. This sample was selected using the random digit telephone dialing, public directories, and sample quotas; population proportional ‘interview’ quotas set to reflect the sex, education, ethnicity and rural or urban residence of the general population within this age group [20].
Participants
Participants were consenting older adults aged 50 to 74 years and then the eligible respondent in the household was the person in that age group with the last birthday. Participants gave verbal consent when contacted by the survey team.
Analyses
Respondent characteristics are described using summary statistics and the percentages affirming each belief are presented. For categorical demographic variables, Chi-squared (without continuity correction) or Fisher’s Exact Tests as appropriate (the latter used instead of the former when more than 20% of cells had expected counts below 5). Missing data was minimal and no formal treatment of this was applied. Analyses were conducted using Stata 15.1 (Stata Corp, 2017). Statistical significance was determined by (two-sided when appropriate) p<0.05.
Data Availability
The data analyzed in this study is freely available by request to the corresponding author. Data will be provided as a pdf or word document.
Results
There were 1,005 respondents included in our present analysis. Respondents were slightly more women (n=518, 51.5%), mostly European (n=921, 91.6%) and well educated (n=100, 46%, with a tertiary qualification, including n=17, 8%, with a post-graduate qualification). A little over half of the sample were from a large urban center (n=540, 53.7%) and the rest were from rural communities.
The majority (n=921, 91.6%) were European with 35 identifying as Māori, (the indigenous people of New Zealand, 3.5%), 42 identifying as “another ethnic group”, 4 identifying as Chinese, 1 as Indian and 2 refusing ethnicity disclosure. It is of note that the sample herein analyzed has fewer Māori and Asian NZers than expected based on census data from the NZ Health Survey.
Education levels were high with 553 having high school education (secondary school, 54.9%), 247 had post-secondary qualifications (BA, BSc or tertiary learning, 24.4%), 103 had postgraduate qualifications (MA, MSc or PhD 10.1%), 88 had a diploma (trade, technical or professional qualifications, 8.6%) and only 14 participants had primary or intermediate schooling.
Nutrition Associated Risk and Protective factors
Open Ended Questions
As shown in (Table 1), in response to the question about risk factors: ‘What do you believe are the 3 factors that will increase the chances of a person experiencing memory problems in older age?’, replies featuring nutritional associated variables focused on “Alcohol Abuse” and “Poor Diet.” Other factors mentioned – Obesity, Diabetes, High Serum Cholesterol and Dehydration were all endorsed by less than 1% of respondents. In response to the protective factors question: ‘What do you believe are the 3 factors that will reduce the chances of a person experiencing memory problems in older age?’ “Healthy Nutrition” was the major focus with 39.6% mentioning this and avoiding alcohol mentioned by 11.1% of respondents while hydration and use of “fish-oil” supplements were mentioned by less than 1% of respondents.
Misconceptions
There are two types of misconceptions that were captured in the present survey. First, participants who underestimated risk factors. The second type of misconceptions are reflection of assigning protective properties to factors that have no scientific evidence supporting this effect. Both types of misconceptions were captured, however, underestimation of established risk factors was more pronounced. The major risks underestimated were less than 1% of participants recognized the risk associated with diabetes, obesity or high serum cholesterol. Poverty, stress and depression were also underestimated but were mentioned by 3.0% to 9.0% of participants. Misconceptions about protective factors may be a reflection of media coverage and advertisements. Regular medical health assessments were mentioned by 1.8% of participants, omega-3 supplements (“fish-oil”) by 1.2% and hydration by 1.0%.
Table 1:Overview of Nutrition Associated Responses (N= 1,005).
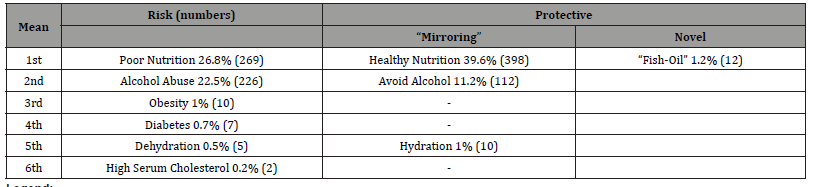
Legend:
Mean: percentage of those providing that response.
Mirroring: response that is the “negative” of a risk response.
Discussion
The present survey demonstrates that general awareness of nutritional factors related to brain health is evident only in a significant minority of older adults in New Zealand. Particular knowledge is patchy and misconceptions about nutrition and brain health are plain. The American Institute of Medicine noted that there are 90 million adults in the United States with limited health literacy [21]. Following this report, health literacy has become an animated area of research. Investigators have expounded on the prevalence of limited health literacy and the relationship of limited health literacy with patients’ knowledge, health behaviors, health outcomes, and medical costs [22]. Health literacy is a set of individual capacities that allow the person to acquire and use new information. These capacities may improve with educational programs or decline with aging [23].
Our findings need to be discussed in light of three recent surveys, from Holland, Germany and from the UK, that are informative and relevant for comparison [24-26]. As part of “What Keeps You Sharp?” - a UK survey completed by adults aged 40–98 years - participants completed an open-ended question about “keeping sharp” in later life. Answers from over 3,000 individuals were analyzed. Keeping fit and healthy in mind, body and spirit was one theme, however only 8.7% of participants specifically mentioned “a healthy diet” or ‘watching one’s alcohol intake” [27]. Analysis of data from the German “Socio-Economic Panel” sample showed that over 80% of individuals 50 years or older perceived dementia to be preventable, however, no strategies related to nutrition were endorsed or rejected [26]. Finally, an online survey undertaken in Holland demonstrated that the majority of participants were unaware of the relationship between lifestyle and dementia risk [24]. There are limitations to our findings: generalization of findings is restricted by the narrow ethnic focus, cognitive ability and mood have not been evaluated due to the study’s design and the bias inherent in a telephone survey. However, this survey has strengths that are a large representative sample, the use of open-ended rather than prompted questions and a high response rate.
In the present study, several findings are of interest. The participants demonstrated what we consider an inadequate level of brain health literacy. Obesity, diabetes, hypercholesterolemia, and alcohol abuse were not adequately recognized as associated with brain health. Although a “Good Nutrition” was endorsed by a significant minority not a single participant detailed either the MIND diet, the Mediterranean diet, or any specific dietary component in their responses. This may reflect a general but vague awareness that nutrition influences brain health. One of the drawbacks to generalization of our findings is the narrow ethnic and cultural focus. There are also marked ethnic inequalities in care seeking and uptake of treatments and lifestyle changes for dementia. Nevertheless, ethnic differences in dementia care are under-explored. Evidence to date suggests there are ethnic differences in risk of dementia. Better understanding of the drivers of these differences may inform efforts to prevent dementia especially as researchers and clinicians prioritize genetic over social explanations when encountering disproportionately high disease rates in ethnic minorities thus distracting from modifiable determinants of health [28,29].
The current generation of ageing adults in the UK anticipates ageing well and maintaining their general well-being. Indeed, most people aged 50 and more rate themselves as ageing well, or successfully, and few rate as high their risk of losing their memory [30]. These positive perspectives reflect a shift away from a predominantly ageist perspective of later life, which exaggerated the extent to which chronic ill health could be attributed to ageing, and which largely, ignored the heterogeneity of the older population. A more positive view of old age is common nowadays [31]. The growing attention to cognitive health promotion among older adults emphasizes the importance of inspecting public understanding of risk and protective factors for dementia. Health beliefs have long been recognized as an important factor in risk self-management and recent studies demonstrate that is true when “dementia worry” is examined [32,33]. The perceived peril of disease - personal vulnerability – is associated with willingness to seek out preventive options whereas beliefs about causes influence self-management [34].
Conclusions
Given our results and the likely overestimation of knowledge in our educated sample compared the findings of the present survey emphasize lacunas in knowledge that may be in need of addressing in order to advance these messages. As our research was undertaken with a representative sample of the population the need for more specific information on nutrition and brain health is emphasized. The dissemination of knowledge about “Brainfood” [35] and elements brain-healthy dietary intervention [36] should become part of public campaigns aiming to help reduce dementia risk.
Ethics Approval and Consent to Participate
Ethical approval for the proposed survey was obtained from the University of Otago Ethics Committee and the Department of Psychological Medicine Ethics Committee, approval # D17/231. Participants gave verbal informed consent when contacted by survey team. All survey methods were performed in accordance with the university of Otago guidelines and regulations.
Consent for Publication
Not Applicable.
Availability of Data
The data analyzed in this study is freely available by request to the corresponding author. Data will be provided as a pdf or word document.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
Funding
None.
Authors’ Contributions
Y Barak designed the study, supervised the data collection and wrote the main manuscript text. AR Atti and MHA Damanhuri assisted with data analysis, prepared the table and wrote the main text.
References
- Liesi E Hebert, Jennifer W, Paul AS, Denis AE (2013) Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology 80(19): 1778-1783.
- Michael DH, Paco M, Kenneth ML (2013) Monetary costs of dementia in the United States. N Engl J Med 369(5): 489-490.
- G Livingston, J Huntley, A Sommerlad, D Ames, C Ballard, et al. (2020) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396(10248): 413-446.
- Cahill S (2021) Personhood, dementia literacy, and the causes and consequences of Alzheimer's disease fear. Int Psychogeriatr 33(10): 997-999.
- Sun F, X Gao, DW Coon (2015) Perceived threat of Alzheimer's disease among Chinese American older adults: the role of Alzheimer's disease literacy. J Gerontol B Psychol Sci Soc Sci 70(2): 247-257.
- Gibney S, G Doyle (2017) Self-rated health literacy is associated with exercise frequency among adults aged 50+ in Ireland. Eur J Public Health 27(4): 755-761.
- Kristine S, Jürgen MP, Florian R, Kristin G, Zofia S, et al. (2015) Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 25(6): 1053-1058.
- (2014) Association., A. s. Brain Health [Internet].
- I Heger, S Köhler, M van Boxtel, M de Vugt, K Hajema, et al. (2020) Raising awareness for dementia risk reduction through a public health campaign: a pre-post study. BMJ Open 10(11): e041211.
- Joyce S, Laura D, Kay D, Sebastian K, Christopher JA, et al. (2023) Cross-sectional survey of attitudes and beliefs towards dementia risk reduction among Australian older adults. BMC Public Health 23(1): 1021.
- Yoram B, Andrew RG, Charlene R, Kate S (2019) The Dunedin dementia risk awareness project: pilot study in older adults. Int Psychogeriatr 32(2): 1-14.
- IB Ljøsne, BB Friedman, S Suri, CS Padullés, S Düzel, et al. (2020) The Global Brain Health Survey: Development of a Multi-Language Survey of Public Views on Brain Health. Front Public Health 8: 387.
- Rui Xu, Qiufang Li, Feifei Guo, Maoni Zhao, Luyao Zhang, et al. (2021) Prevalence and risk factors of frailty among people in rural areas: a systematic review and meta-analysis. BMJ Open 11(4): e043494.
- (2017) AICR/WCRF. Food, Nutrition, physical Activity, and Prevention of Cancer: A Global Perspective. Continuous Update Project (CUP) reports.
- Yoram Barak, Andrew R Gray, Charlene Rapsey, Kate Scott (2020) The Dunedin dementia risk awareness project: pilot study in older adults. Int Psychogeriatr 32(2): 241-254.
- Barak Y, C Rapsey, KM Scott (2022) Clusters of Dementia Literacy: Implications from a Survey of Older Adults. J Prev Alzheimers Dis 9(1): 172-177.
- Winsome P, Noela W, Donnell A, Mark W, Micalla W, et al. (2008) Exploring the relationship between sugars and obesity. Public Health Nutr 11(8): 860-866.
- Pledger M, G Martin, J Cumming (2016) New Zealand Health Survey 2012/13: characteristics of medicinal cannabis users. N Z Med J 129(1433): 25-36.
- FJ Fowler Jr, PM Gallagher, VL Stringfellow, AM Zaslavsky, JW Thompson, et al. (2002) Using telephone interviews to reduce nonresponse bias to mail surveys of health plan members. Med Care 40(3): 190-200.
- (2012) Health., M.o., The Health of New Zealand Adults 2011/12: Key Findings of the New Zealand Health Survey., MOH., Editor Government of New Zealand: Wellington.
- Lynn Nielsen-Bohlman, Allison M Panzer, David A Kindig (2004) Health literacy: A prescription to end confusion. I.o. Medicine, Editor the National Academies Press.: Washington, DC.
- Baker DW (2006) The meaning and the measure of health literacy. J Gen Intern Med 21(8): 878-883.
- DW Baker, JA Gazmararian, J Sudano, M Patterson (2000) The association between age and health literacy among elderly persons. J Gerontol B Psychol Sci Soc Sci 55(6): S368-374.
- I Heger, K Deckers, M van Boxtel, M de Vugt, K Hajema, et al. (2019) Dementia awareness and risk perception in middle-aged and older individuals: baseline results of the MijnBreincoach survey on the association between lifestyle and brain health. BMC Public Health 19(1):
- Niechcial M, R Vaportzis, A Gow (2019) What keeps you sharp? People's views about preserving thinking skills in old age. Age and Ageing 48: 32-35.
- Hajek A, HH König (2020) Determinants of Perceived Own Risk for Developing Dementia and the Perception That Memory Deterioration Is Preventable. Findings From the General Adult Population in Germany. Front Med (Lausanne) 7: 203.
- Niechcial MA, E Vaportzis, AJ Gow (2019) People’s views on preserving thinking skills in old age. Educational Gerontology 45(5): 341-352.
- JD Walker, G Spiro, K Loewen, K Jacklin (2020) Alzheimer's Disease and Related Dementia in Indigenous Populations: A Systematic Review of Risk Factors. J Alzheimers Dis 78(4): 1439-1451.
- SI Shiekh, SL Cadogan, L Yu Lin, R Mathur, L Smeeth, et al. (2021) Ethnic Differences in Dementia Risk: A Systematic Review and Meta-Analysis. J Alzheimers Dis 80(1): 337-355.
- Bowling A, P Dieppe (2005) What is successful ageing and who should define it? Bmj 331(7531): 1548-1551.
- Bowling A, S Iliffe (2011) Psychological approach to successful ageing predicts future quality of life in older adults. Health Qual Life Outcomes 9: 13.
- Bowen CE, EM Kessler, J Segler (2019) Dementia worry in middle-aged and older adults in Germany: sociodemographic, health-related and psychological correlates. Eur J Ageing 16(1): 39-52.
- Sayegh P, BG Knight (2013) Cross-cultural differences in dementia: the Sociocultural Health Belief Model. Int Psychogeriatr 25(4): 517-530.
- Janz NK, MH Becker (1984) The Health Belief Model: a decade later. Health Educ Q 11(1): 1-47.
- Hügel HM (2015) Brain Food for Alzheimer-Free Ageing: Focus on Herbal Medicines. Adv Exp Med Biol 863: 95-116.
- AR Shaw, MN Key, S Fikru, S Lofton, DK Sullivan, et al. (2023) Development of a Culturally Adapted Dietary Intervention to Reduce Alzheimer's Disease Risk among Older Black Adults. Int J Environ Res Public Health 20(17): 6705.
-
Yoram Barak*, Hanafi Ahmad Damanhuri and Anna Rita Atti. Public Views About Nutrition and Brain Health: A Survey of Older Adults in New Zealand. Glob J Aging Geriatr Res. 2(5): 2024. GJAGR.MS.ID.000548.
-
Nutrition, Brain Health, Older Adults, Dementia, Malnutrition, Health Survey, Alcohol, Literacy
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






