 Research Article
Research Article
Prevalence of Comorbidity Among Elderly
Salem Alsuwaidan1*, Abrar Algharbi2, Shrooq Alyami2, Norah Almukhlifi2 and Sundus Alsalamah2
1Research and Innovation Center, King Saud Medical City, Ministry of Health, KSA
2King Saud Medical City Academy for Postgraduate Studies in Family Medicine, Ministry of Health, KSA
Salem Alsuwaidan, Research and Innovation Center, King Saud Medical City, Ministry of Health, KSA.
Received Date:July 28, 2021; Published Date:August 24, 2021
Abstract
Comorbidity is the association of one or more diseases co-exiting with the primary chronic condition in the same individual. It is sometimes considered to be a secondary diagnosis, having been recognized during or after treatment for the principal diagnosis. While the elderly people are defined as those who have 65 years old and more; also have more experiences with chronic conditions due limited regenerative abilities and are more susceptible to disease, syndromes, injuries, and sickness compared with younger adults. There is no specific prevalence study in Saudi Arabia related to the prevalence of comorbidities in elderly patients.
The objectives of the present study were:
• To identify the most common chronic comorbidities among the elderly.
• To explore the association between age and the number of comorbidities.
Aiming to evaluate prevalence of comorbidities in elderly patients.
This study will analyze the comorbidities among elderly patients, which is a factor to help the future prospective on how to make a better control on health and disease conditions in elderly subjects. The average concurrent chronic diseases were 2.01 for the elderly patients with average of their age of about 75 years. About 60% (3482) elderly patients were having two diseases or more and up to six concurrent chronic diseases. There was no specific nationality having specific chronic disease in elderly patients. The most frequent disease was hypertension with 58.1%, then diabetes mellitus with 48.6%. The average number of the concurrent diseases have no correlation with the progress of age, either decreasing or increasing the age (in year). Cases represented in percentage in each particular disease showing variation over age progress.
Keywords:Comorbidity; Elderly; Prevalence.
Introduction
Comorbidity is the association of one or more diseases coexiting with the primary chronic condition in the same individual. It is often called multiple morbidities or multi-morbidities, and most frequently called as “comorbidity”. There is no standard method on how to assess comorbidity, but it is one of the basics to assess comorbidity in order to avoid any risk or future complication [1]. Comorbidity is associated with worse health outcomes, more complex clinical management, and increased health care costs. There is no specific mechanism that may underlie the coexistence of two or more diseases in a patient (direct causation, associated risk factors, heterogeneity, independence) are examined, and the implications for clinical care considered [2].
Elderly people are defined as those who have 65 years old and more; they used to suffer from chronic diseases due limited regenerative abilities and are more susceptible to disease, syndromes, injuries and sickness compared with younger adults. The structural, functional, and molecular levels of their physiology are changes; in fact, in elderly people, most of the major organ system experiences physiological changes. The changes to the nervous system result mostly in cognitive impairments; the cardiovascular system develops higher blood pressures with lower cardiac output; the respiratory system undergoes a reduction of arterial oxyhemoglobin levels the gastrointestinal system experiences delayed gastric emptying and reduction of hepatic metabolism; and the renal system experiences a diminished glomerular filtration rate [3].
Comorbidity diseases for elderly patients aged 65 years and older had been reported by Alsuwaidan et al., that Saudi Arabia has a great percentage of geriatric patients associated with multiple chronic diseases that require close attention and monitoring for their medications. In Saudi Arabia, hypertension was the most common comorbidity disease with more than 47% followed diabetes mellitus with 37.3%, which almost with same percent as hyperlipidemia with about 36% [4].
There is no specific prevalence study in Saudi Arabia related to the comorbidities in elderly patients, however, in southern Saudi Arabia, 11% of elderly had one morbidity and 89% had two comorbidity or more [5]. The prevalence of physical comorbidity in elderly with depression was 78.7% that have at least one comorbidity [6] and about 44% have multimorbidity in china [7] and around 80% of elderly in Australia having three or more illnesses [8]. Patients with multiple chronic conditions have on average a higher level of morbidity, poorer physical functioning and quality of life, a greater likelihood of persistent depression, and lower levels of social wellbeing [9]. Elderly patients often develop complicated and multi-factorial health states that require extensive pharmacotherapy, leaving this population at risk for exposure to drug-drug interactions and other adverse events [10].
The progress and development increase the level of quality of life where, elderly or age progressing have no influence on quality of life [11-20] on the other hand, comorbidity should have a negative influence on quality of life. Therefore, studying the combination of comorbidity and elderly patients is very important to identify and assess a degree of comorbidity to avoid risk and complication in elderly subjects. This requires primary and secondary prevention of ill health through synergies such as low carbon transport systems that promote physical activity, improve physical fitness and reduce avoidable morbidity and mortality, promote health and wellbeing through community-based approaches and by promoting protective factors, reduce risk of common risk factors (e.g., smoking, obesity, alcohol, poor diet, physical inactivity).
Aim and objectives
Promoting physical activities should improve healthcare and physical fitness in order to avoid comorbidities. Moreover, understanding, planning, managing risks and complications for elderly subjects should help for appropriate strategies.
The objectives of the present study were:
1. To identify the most common chronic comorbidities
among the elderly.
2. To explore the association between age and the number of
comorbidities.
Aiming to evaluate prevalence of comorbidities in elderly patients at the King Saud Medical City.
Methodology
Study Setting: The study will take place at King Saud Medical City in Riyadh during the period from Jan 2017- Dec 2019; this is to exclude any effect of the COVID-19 pandemic and targeting most of elderly patient’s records.
Study Design: This study is a retrospective cross-sectional study of the database linked with patient information available from the medical files of all patients aged 65 years and older with two or more chronic medical illnesses to be included in this study. The data will be collected retrospectively, including socio-demographic features as well as comorbidities.
Study Population: The geriatric patients admitted to different departments of King Saud Medical City. This study will consider geriatrics as subjects aged 65 years and older have one or more chronic medical conditions. The medical files of all the elderly patients admitted to King Saud Medical City during the period from Jan 2017- Dec 2019 (3 years) and to avoid any effect of the COVID-19 so that will be reviewed in this study to determine the prevalence of comorbidities.
Sample Size: This study was conducted on 5874 elderly patients whom have one or more than one particular diseases.
Inclusion criteria:Those patients should meet the inclusion criteria and therefore will be included in this study. Male or female subjects aged 65 years or older with two or more medical conditions.
Exclusion criteria:Subjects will be excluded if they are less than 65 years. Any elderly subject has no medical profile in the King Saud Medical City.
Database Collection: Data collection sheet template structured using Excel included the age, gender, and the categories of the comorbidities. Only qualified and professional candidates will be chosen for data entry and data verification to present the quality and accuracy of data.
Comorbidities Categories:This study divided comorbidities into major categories; should include Hypertension, Diabetes mellitus, Asthma, Dyslipidemia, Cardiac diseases, Lung diseases, Renal diseases, Rheumatic diseases, Cancer, Neurological diseases, Psychiatric (mental) diseases and others (including gastric diseases).
Statistical Considerations
The primary hypothesis of this study is to identify the most common chronic comorbidities among the elderly and to explore the association between age and the number of comorbidities aiming to evaluate prevalence of comorbidities in elderly patients [21-27]. The primary analysis will use descriptive analysis for demographic and exposure characteristics of the participants.
Results
This is a cross sectional observational study conducting on 5874 elderly patients who have one or more than one particular diseases. The average of their age was 75 years (± 8 SD), 2401 (40.9%) were female and 3473 (59.1%) were males. Almost 40% (2393 patients) out of the total number 5874 elderly were having only one chronic disease. The average concurrent chronic diseases for these particular subjects were 2.01 (± 1.01 SD). They were collectively from 38 nationalities were classified according to their income and environment to “Saudis and Gulf Corporation Countries”, “Arabian Middle East”, “Asian and Far East”, “Americans, Europeans, and Australians” and “African countries” as shown in Figure 1. Frequency and percentage of elderly patients according to nationality was shown in Table 1. There was no difference in total number of diseases in terms of nationality in individuals with over 65 years old whom getting full treatment at the KSMC.
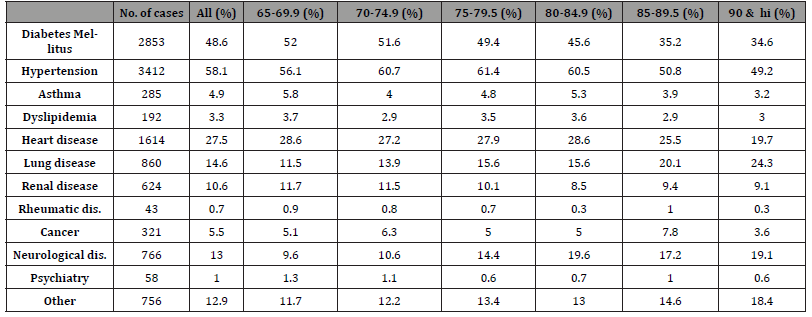
Most of the valid cases for elderly patients were hypertension with 3412 (58.1%), diabetes mellitus 2853 (48.6%), Asthma 285 (4.9%), dyslipidemia 192 (3.3%), Cardiac diseases 1614 (27.5%), lung diseases 860 (14.6%), renal 624 (10.6%), rheumatic diseases 43 (0.7%), cancer 321 (5.5%), neurological diseases 766 (13%), psychiatric 58 (1%) and others (including gastric diseases) 756 (12.9%).Table 2 showed more descriptive for the number of cases and percentage of the diseases as age categories in elderly patients over age progressing.

Table 1:Frequency and percentage of elderly patients showing their chronic disease according to nationality including the frequency number of diseases and percentages.
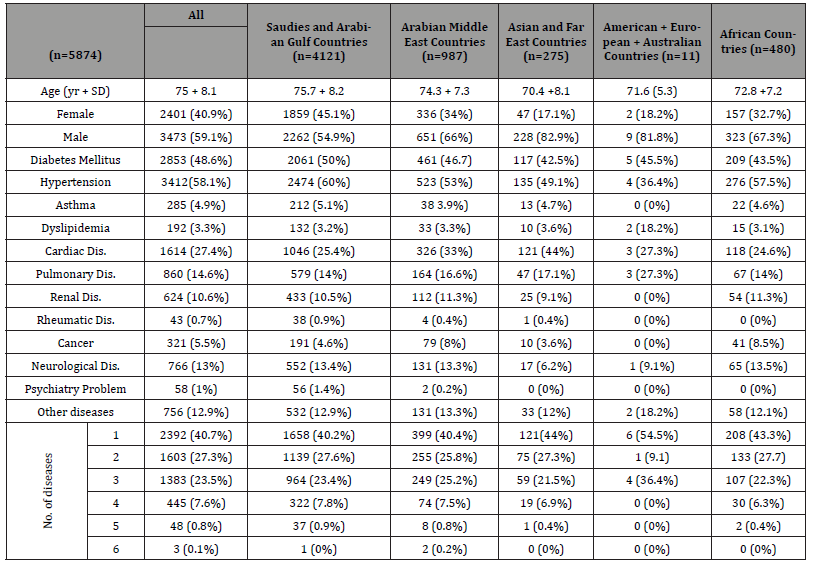
Table 2:Number of cases and percentage of the most frequent diseases in elderly patients over age progressing.
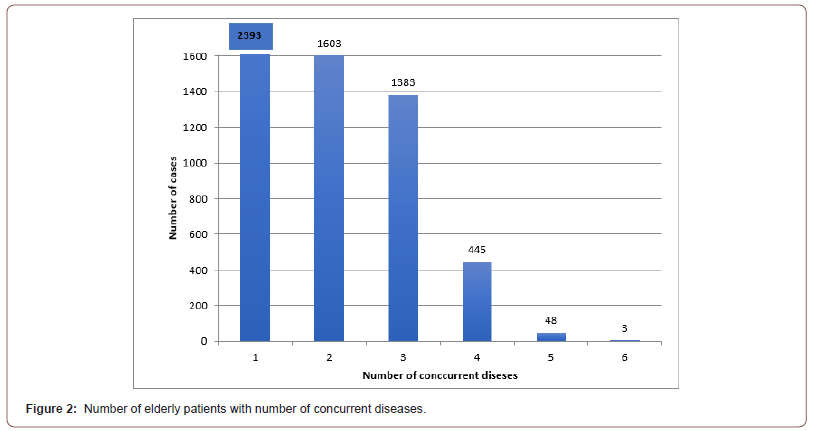
Comorbidity diseases in elderly patients were defined as an elderly patient (> 65 years) having more than one concurrent chronic disease. Results showed that elderly patient with only one disease were 2394 (40.7%) out of 5874, whereas 3482 elderly patients were having two diseases or more and up to six concurrent chronic diseases as showing Figure 2. The main focus will be on the 3482 patients (59.3% of the total population) and their comorbidity characteristics.
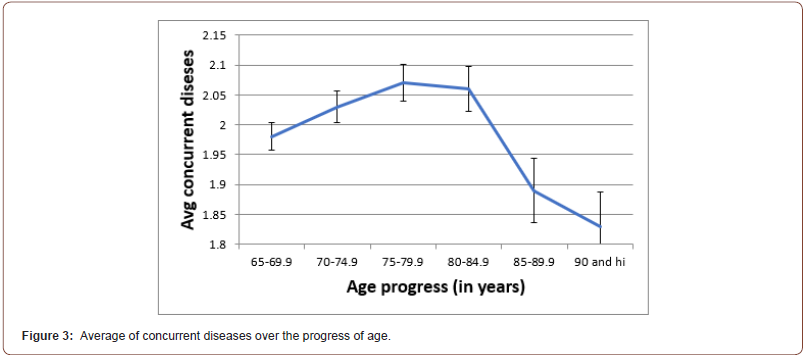
Age has no influence on the concurrent diseases, so that the average of the concurrent diseases did not affect by decreasing or increasing the age if it is within the elderly patients. Results of this study showed that the average number of concurrent diseases were with minor variation over age progressing. The linear graph of average number of diseases was with mild increment in average number of diseases during the age of 80s years, then it went declining with less average number of concurrent diseases than it started on 65 years as shown in Figure 3.
Number of cases in each particular disease represented in percentages has no specific correlation over age progressing. In diabetes mellitus, the number of cases showing declining over age progressing, while in hypertension showing variation by declining over age progressing after mild increment in number of cases during the age of 75-85 years as shown in Table 1 a similar profile had been shown in most of other disease.
Discussion
This study was conducting on 5874 elderly patients, their age was 75 years (± 8 SD), 2401 (40.9%) were female and 3473 (59.1%) were males. Almost 40% out of the total number 5874 elderly were having only one chronic disease. The average concurrent chronic diseases for these particular subjects were 2.01 (± 1.01 SD). They were collectively from 38 nationalities where were classified according to their income and environment; the results showed that there is no specific nationality for the elderly disease. Full descriptive statistics including frequency and percentage of elderly patients showing their chronic disease according to nationality including the frequency number of diseases and percentages, shown in Table 1. There was no difference in total number of diseases in terms of nationality in individuals with over 65 years old whom getting full treatment at the KSMC. There was no specific nationality having specific chronic disease in elderly patients.
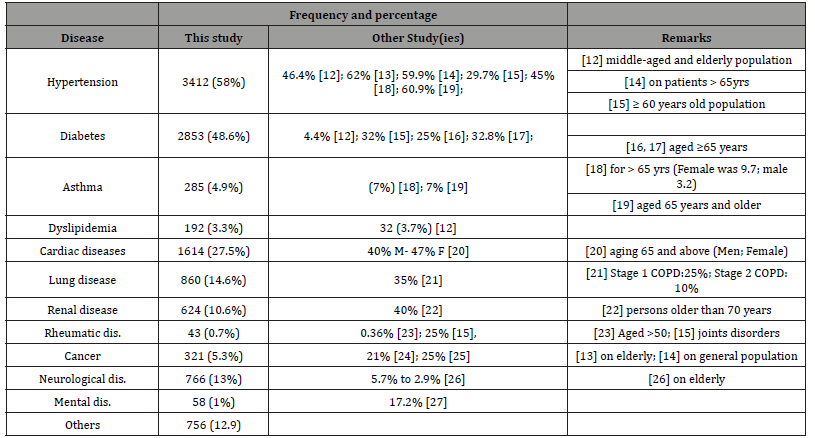
Out of 5874, the most frequent three diseases in this study were hypertension with (3412), diabetes (2853) and cardiac diseases (1614) with a prevalence of 58.1%, 48.6% and 27.3% respectively. In a comparison with other studies, it showed that hypertension ranged from almost 30% to 60.9%, then diabetes mellitus ranged 4.4% to 32.8% and cardiac diseases, which are vary between male and female however it is with ranged about 40s%. Other comorbidities including frequency and percentages were illustrated in the below Table 3.
Table 3:A table showing the percentages of the most frequently diseases in elderly patients compared with other studies.
Comorbidity diseases in elderly patients were defined earlier as older than 65 years and having more than one concurrent chronic disease. Results showed that elderly patient with only one disease were 2394 (40.7%) out of 5874. This study will focus on these 3482 patients (59.3% of the total population) and their comorbidity characteristics. Although age difference in particular population for elderly aged 77-100 having 55% with comorbidity (more than one disease) [28], compared with 36% of the asthmatic patients experienced more comorbidity simultaneously [29].
Progress in aging has no influence on number of the concurrent diseases. The average number of the concurrent diseases did not affect by decreasing or increasing the age (in year). Results of this study showed declining average number of diseases over age progressing after mild increment in average number of diseases during the age of 80s years as shown in Figure 3. Number of cases in particular disease also shown declining over age progressing during age categories with also mild increment in number of disease during the age of 75-85 years as shown in Table 2.
Number of cases in each particular disease showing variation over age progress, this was represented in percentage as in Table 2. Most of the diseases showing increasing in number of cases (and also percentage wise) during the period of age at 75-85 years then declining; this is either by improving their situation or passing away. A similar profile had been shown in previous study (Alsuwaidan R). However, elderly patients with diabetes mellitus showing reducing in number of cases and percentage over age progressing. There is no specific correlation to explanation this variation of disease over age progressing.
Conclusion
The average concurrent chronic diseases were 2.01 for the elderly patients with average of their age of about 75 years. About 60% (3482) elderly patients were having two diseases or more and up to six concurrent chronic diseases. There was no specific nationality having specific chronic disease in elderly patients. The most frequent disease was hypertension with 58.1%, then diabetes mellitus with 48.6%. The average number of the concurrent diseases have no correlation with the progress of age, either decreasing or increasing the age (in year). Cases represented in percentage in each particular disease showing variation over age progress.
Ethical consideration
Investigators granted Institutional Review Board (IRB) approval “H1RI-02-Jul20-02” after clear assurance for the IRB committee that all the processes of this study will be in accordance of the Good Clinical Practice standards and regulations, and inconsistence with the declaration of Helsinki. Investigators also assure the IRB committee that confidentiality of patients’ names, medical record numbers, identity, and identification numbers will be the most important consideration.
Acknowledgments
Authors acknowledge, commitment, and sacrifice of the staff at data warehouse and statistics administration at the King Saud Medical City for their dedication [30]. All authors substantially contributed to the conception, design, analysis, and interpretation of data and checking and approving the final version of the manuscript, and we agree to be accountable for its contents.
Conflict of interests
The authors declare that there are no existing commercial or financial relationships that could, in any way, lead to a potential conflict of interest.
Sponsorship
None.
References
- Breccia M, Latagliata R, Stagno F, Luciano L, Gozzini A, et al. (2011) Charlson comorbidity index and adult comorbidity evaluation-27 scores might predict treatment compliance and development of pleural effusions in elderly patients with chronic myeloid leukemia treated with second line dasatinib. Haematologica 96(10): 1457-1461.
- Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M (2009) Defining comorbidity: implications for understanding health and health services. The Annals of Family Medicine 7(4): 357-363.
- Alvis BD and Hughes CG (2015) Physiology considerations in geriatric patients. Anesthesiology clinics 33(3): 447-456.
- Alsuwaidan A, Almedlej N, Alsabti S, Daftardar O, Al Deaji, F, et al. (2019) A comprehensive overview of polypharmacy in elderly patients in Saudi Arabia. Geriatrics 4(2): 36.
- Al Modeer MA, Hassanien NS and Jabloun CM (2013) Profile of morbidity among elderly at home health care service in Southern Saudi Arabia. Journal of family & community medicine 20(1): 53-7.
- Grover S, Avasthi A, Sahoo S, Lakdawala B, Dan A, et al. (2018) Prevalence of physical comorbidity and prescription patterns in elderly patients with depression: A multicentric study under the aegis of IAGMH. Journal of Geriatric Mental Health 5(2): 107-114.
- Zhang R, Lu Y, Shi L, Zhang S, Chang F (2019) Prevalence and patterns of multimorbidity among the elderly in China: a cross-sectional study using national survey data. BMJ open 9(8): e024268.
- Australian Institute of Health (2012) Australia's health 2012: the thirteenth biennial health report of the Australian Institute of Health and Welfare. AIHW.
- Davis JW, Chung R and Juarez DT (2011) Prevalence of comorbid conditions with aging among patients with diabetes and cardiovascular disease. Hawaii medical journal 70(10): 209-213.
- Bjerrum L, Søgaard J, Hallas, J, Kragstrup J (1998) Polypharmacy: correlations with sex, age and drug regimen A prescription database study. European journal of clinical pharmacology 54(3): 197-202.
- Nóbrega TCMD, Jaluul O, Machado AN, Paschoal SM, Jacob Filho W (2009) Quality of life and multimorbidity of elderly outpatients. Clinics 64(1): 45-50.
- Ejim EC, Okafor CI, Emehel A, Mbah AU, Onyia U, et al. (2011) Prevalence of cardiovascular risk factors in the middle-aged and elderly population of a Nigerian rural community. Journal of tropical medicine.
- Brindel P, Hanon O, Dartigues JF, Ritchie K, Lacombe JM, et al. (2006) Prevalence, awareness, treatment, and control of hypertension in the elderly: the Three City study. Journal of hypertension, 24(1): 51-58.
- Yang ZQ, Zhao Q, Jiang P, Zheng SB, Xu B (2017) Prevalence and control of hypertension among a Community of Elderly Population in Changning District of shanghai: a cross-sectional study. BMC geriatrics 17(1): 1-9.
- Khoja AT, Aljawadi MH, Al Shammari SA, Mohamed AG, Al Manaa HA, et al. (2018) The health of Saudi older adults; results from the Saudi National Survey for Elderly Health (SNSEH) 2006–2015. Saudi Pharmaceutical Journal 26(2): 292-300.
- Lange S, Diehm C, Darius H, Haberl R, Allenberg JR, et al. (2004) High prevalence of peripheral arterial disease and low treatment rates in elderly primary care patients with diabetes. Experimental and clinical endocrinology & diabetes 112(10): 566-573.
- Dybicz SB, Thompson S, Molotsky S, Stuart B (2011) Prevalence of diabetes and the burden of comorbid conditions among elderly nursing home residents. The American journal of geriatric pharmacotherapy 9(4): 212-223.
- Park SY, Kim JH, Kim HJ, Seo B, Kwon OY, et al. (2018) High prevalence of asthma in elderly women: findings from a Korean national health database and adult asthma cohort. Allergy, asthma & immunology research 10(4): 387-396.
- Oraka E, Kim HJE, King ME, Callahan DB (2012) Asthma prevalence among US elderly by age groups: age still matters. Journal of asthma 49(6): 593-599.
- Dewhurst G, Wood DA, Walker F, Lampe FC, Jeffreys M, et al. (1991) A population survey of cardiovascular disease in elderly people: design, methods and prevalence results. Age and ageing 20(5): 353-360.
- Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, et al. (2002) Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. European Respiratory Journal 20(5): 1117-1122.
- Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, et al. (2007) Prevalence of chronic kidney disease in the United States. Jama, 298(17): 2038-2047.
- Peschken CA and Hitchon CA (2012) Rising prevalence of systemic autoimmune rheumatic disease: increased awareness, increased disease or increased survival. In Arthritis Research & Therapy Bio Med Central 14(3): 1-28.
- Berthier F, Grosclaude P, Bocquet H, Faliu B, Cayla F, et al. (1997) Prevalence of cancer in the elderly: discrepancies between self-reported and registry data. British journal of cancer 75(3): 445-447.
- Schrijvers CT, Stronks K, van de Mheen DH, Coebergh JWW, Mackenbach JP (1994) alidation of cancer prevalence data from a postal survey by comparison with cancer registry records. American Journal of Epidemiology 139(4): 408-414.
- Manton KG, Gu XL, Ukraintseva SV (2005) Declining prevalence of dementia in the US elderly population. Успехи геронтол (16) : 30-37.
- Palay J, Taillieu TL, Afifi TO, Turner S, Bolton JM, et al. (2019) Prevalence of mental disorders and suicidality in Canadian provinces. The Canadian Journal of Psychiatry 64(11): 761-769.
- Yáñez A, Soria M, De Barayazarra S, Recuero N, et al. (2018) Clinical characteristics and comorbidities of elderly asthmatics who attend allergy clinics. Asthma research and practice 4(1): 1-7.
- Marengoni A, Winblad B, Karp A, Fratiglioni L (2008) Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. American journal of public health 98(7): 1198-1200.
- Ninios I, Pliakos C, Ninios V, Karvounis H, Louridas G (2007) Prevalence of interatrial block in a general population of elderly people. Annals of Noninvasive Electrocardiology 12(4): 298-300.
-
Salem Alsuwaidan, Abrar Algharbi, Shrooq Alyami, Norah Almukhlifi. Prevalence of Comorbidity Among Elderly. Glob J Aging Geriatr Res. 1(4): 2021. GJAGR.MS.ID.000518.
-
Comorbidity; Elderly; Prevalence.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






