 Short Communication
Short Communication
Effects Of 1-Year Of Health Coaching and Health Education Interventions on Physical Function of Middle Aged and Older Adults
Megan D Jones1*, Anthony Campitelli1, Joshua L Gills2, Ray Urbina1, Charlie Rodgers1, Jenova A Kempkes1,Sally Paulson3, Jordan M Glenn4, Kelsey Bryk4, Jennifer Myers4, Erica N Madero4 and Michelle Gray1
1University of Arkansas, Department of Health, Human Performance and Recreation, Fayetteville, AR, USA
2Rutgers University, Center for Molecular and Behavioral Neuroscience, School of Arts and Sciences-Newark, Newark, NJ, USA
3St. Elizabeth Healthcare, Edgewood, KY, USA
4Neurotrack Technologies, Inc., Redwood City, CA, USA
Megan D Jones, University of Arkansas, Department of Health, Human Performance and Recreation, Fayetteville, AR, USA
Received Date:February 27, 2024; Published Date:March 06, 2024
Abstract
Physical function is an accepted predictor of health outcomes in the adult population. Remaining physically active throughout the lifespan may aid in preserving physical function. Commonly reported causes of decreased physical activity include lack of motivation, support, and knowledge. Studies have shown health coaching is an effective tool for improving physical activity and health outcomes in older adults and those with chronic diseases. Research is lacking on the effectiveness of health coaching in younger, healthy populations.
Purpose: To evaluate the impact of health coaching or health education on physical function among adults.
Methods: Adults 45-75 were randomly sorted to a health coaching (HC) (N:112; age:62.4±7.7) or a health education (HE) (N:104; age:61.5±8.8)
intervention for 12 months. Participants completed physical function assessments including standing balance, handgrip, chair stands, habitual walk,
and 6-minute walk along with body composition testing at baseline and 12 months. 2x2 factorial ANOVAs were used to determine if there was a
group by time interaction effect for any dependent variable after 12-months of intervention.
Results: There were no group by time interaction effects revealed for physical function or body composition variables after 12 months of
intervention. Main effects for time were shown for lean mass, handgrip, chair stands, and 6-minute walk with those in HC expressing greater
improvements when compared to HE.
Conclusion: Although results indicate both HC and HE are effective means of improving physical function in adults, HC revealed improvements
to a greater extent than HE.
Keywords:Aging; Health Behavior; Physical Activity; Intervention Study
Introduction
The population over the age of 60, commonly known as older adults, is rapidly growing worldwide [1,2]. Concurrently, there are also increases in the number of individuals with chronic diseases and disabilities [2]. Although causes for chronic diseases and disabilities are multifactorial, it is widely accepted that physical function, or the ability to perform basic and instrumental activities of daily living throughout the lifespan, is a predictor of health outcomes in the adult population [2-7]. Preserving physical activity later in life may aid in maintaining physical function, slowing agerelated declines in physical abilities, and in preventing chronic disease and disabilities [3,5,8-10]. Although some age-related declines are expected (sarcopenia, bone mineral density loss, gait changes), it is possible to prevent or slow the progression, while preventing the onset of chronic diseases [2,5,8,11-14].
Age is positively associated with low levels of physical activity, with individuals in the older adult population reporting the lowest level of physical activity when compared to young and middle-aged adults [2,15]. It is estimated that 23% of adults do not meet the World Health Organization recommendations for physical activity, even though the benefits of physical activity are well established [2,16]. Commonly reported reasons for sedentary behavior include lack of motivation, support, resources, and knowledge [15]. Instituting physically active lifestyles and implementing regular exercise starting at younger ages could prevent chronic disease and help maintain physical function late in life [4,10,16,17]. With healthcare costs on the rise, it is essential that inexpensive, scalable, effective interventions are available to individuals of all ages to help decrease sedentary activity and maintain physical function later in life [8,15,16].
Health coaching is gaining attention as a cost-effective means of modifying lifestyle behaviors [10,18-21]. As opposed to a “one size fits all” program for health-related changes, health coaching uses motivational interviewing techniques allowing individuals to set solution-based goals in order to achieve healthy lifestyle modifications [10,20,22,23]. Health coaching introduces health education with the aid of a qualified professional who discusses current health status, provides recommendations for lifestyle modifications, assists with individualized goal setting, identifies challenges, and provides guidance, motivation, and encouragement throughout the program [10,19,22-27]. The goal of a health coach is to enhance the well-being of individuals by meeting them where they are in the behavior change process [10,26,27]. Throughout the health coaching program, the health coach will revisit each lifestyle domain, offer new recommendations for lifestyle modifications, and allow the individual to move forward at their own pace. This allows individuals to develop accountability for their health behaviors through self-discovery of strengths and weaknesses [9,13-16,18- 20].
To date, several studies have investigated the potential health benefits of lifestyle modifications with the aid of health coaching among individuals with chronic disease and among older adults. Health coaching interventions are effective for improving body weight, blood pressure, HDL levels, and physical activity among these populations [10,20,23-28]. As previously stated, sedentary behavior is an issue throughout adulthood yet, few studies have investigated the benefits of health coaching in populations outside of older adults [29]. The purpose of the current investigation was to evaluate the impact of health coaching on physical function among adults aged 45-75.
Methods
Study Design and Participants
This was a randomized controlled trial (RCT) consisting of male and female participants 45-75 years. Prior to study enrollment, participant ID numbers were randomized as being health coaching (HC) or health education (HE). As participants were enrolled, they were randomly assigned to a participant ID number which assigned them to HC or HE. Participants were recruited from Northwest Arkansas and surrounding areas (Arkansas, Oklahoma, Texas, Missouri) via advertisements broadcast on local radio stations, including National Public Radio (NPR), social media advertisements, and word-of-mouth. Participants reported at two time points (Time 1 = baseline and Time 2 = 12 months after Time 1). At each time point, biometric data, including height, weight, and body composition, were collected. Participants also completed a series of physical function assessments including standing balance, repeated chair stands, handgrip, 4-meter (4m) habitual walking trials, and a 6-minute walking assessment. This study was nonblinded as researchers were required to educate participants on the requirements of their randomly assigned groups and how to access the health coach (HC participants) after their Time 1 visit along with following up on HC compliance at Time 2.
Inclusion Criteria
The data collected and analyzed for this study were collected as part of the larger DC MARVel study [21]. Participants of this study were required to be between the ages of 45-75 years at Time 1 and be able to participate in light to moderate physical activity. Participants of the study were enrolled because they were considered at risk for Alzheimer’s Disease (AD) and were required to have at least 2 positive risk factors for AD including a BMI between 18.5-39.3 kg/m2, a history of diabetes, hypertension, or high cholesterol. Furthermore, participants were required to have no more than 1 protective factor for AD, which included high level of physical activity, high fish consumption, or a high level of cognitive engagement [21]. Individuals who had a physician diagnosis of a mental health condition, neurologic condition, dementia or mild cognitive impairment, had a recent cardiovascular event, or who were already participating in another lifestyle change program were excluded from the study [21]. Prior to Time 1 testing, participants who met inclusion criteria and completed the informed consent were randomly assigned to HC or HE [21].
Body Composition Assessment
Body weight and height were measured on a Detecto Physician’s Scale (Detecto, Webb City, MO). BMI was calculated as body mass (kg) over height (m2) [30]. Body composition was evaluated using a Prodigy TM Dual-energy x-ray absorptiometry unit (Lunar Corporation, Madison, WI) [21].
Short Physical Performance Battery (SPPB)
Physical function was assessed using the Short Physical Performance Battery (SPPB) protocol [31]. The SPPB protocol is commonly used to measure lower extremity physical performance and is a reliable and valid predictor of physical function, fall risk, and all-cause mortality [6, 32, 33]. Assessments of this protocol are scored individually and complied into one score ranging from 0 (worst) to 12 (best). This protocol examines standing balance by having the participants stand with feet side-by-side, a semitandem position, and then a tandem position. The amount of time the participant holds each stand determines the score (10 second maximum). Lower extremity endurance was assessed using repeated chair stands. Using a stable, straight-back chair with a seat height of 0.43m, participants were instructed to sit in the chair with feet firmly on the floor with arms and hands crossed over the chest and then stand up and sit back down as quickly as possible five times consecutively. The score for the assessment is based on the amount of time (seconds) it takes the participant to complete five full stands. Lastly, walking speed was assessed with a 4-meter habitual walk which took place in a well-lit, flat-surfaced hallway with the start and finished clearly marked with unraised lines in the floor and orange cones. Scoring was determined by how long (seconds) it took to complete 4 meters at a habitual walking pace [31].
Upper Body Strength
Handgrip testing has been used as a reliable and valid assessment of upper body muscular strength and has been shown to be an effective measure of functional fitness in adults [13, 34]. A Takei hand grip dynamometer (Takei Scientific Instruments Co, Ltd), appropriately set to accommodate each participant’s hand size, was used to complete testing. Participants were instructed to maximally squeeze for 3 seconds. The score provided by the unit (kg) was recorded by a researcher, and they were instructed to duplicate the same procedure on the other hand. Testing was completed three times on each hand with a 1-min rest between trials. For analyses, the average score of the three trials was calculated for each hand, and then the average of the two hand scores was used to create one score for handgrip total score [30].
Aerobic Fitness
Cardiovascular endurance was assessed by a 6-minute walking trial, which is a reliable and valid measure of aerobic fitness and can be administered to individuals with a broad range of aerobic capabilities [33, 35]. Two cones were placed 25m apart in a well-lit hallway and participants were instructed to walk laps around the two cones resulting in a 50m lap. Participants were given instructions to complete as many laps as they could, while maintaining a walking form (1 foot on the ground), in 6 minutes. At the conclusion of the 6 minutes, participants were verbally instructed to stop where they were and if they stopped between the two cones, the researcher measured the remaining distance of the lap to precisely record the distance completed [21].
Health Coaching (HC)
Participants assigned to HC had access to a personal health coach. Health coaching sessions were scheduled every 6-8 weeks with each session lasting 30-45 minutes, via videoconferencing. The focus of health coaching was to improve lifestyle domains including physical activity, nutrition, sleep, stress, social engagement, and cognition. The health coach educated participants on each of these domains and provided lifestyle recommendations which could benefit them individually. Each participant was allowed to select one or more lifestyle domains they wanted to work on, allowing them to determine where they felt most ready to make lifestyle changes. The health coach guided each participant through the goal setting process, addressed barriers to change, and provided encouragement throughout the study. As goals were achieved, participants were encouraged to set new goals and to explore lifestyle changes in alternate domains. Along with scheduled meetings, participants received asynchronous chat messages from the health coach and educational articles on lifestyle modifications. HC participants were informed that they could reach out to the health coach with questions via chat messages any time throughout the study [21].
Health Education (HE)
Participants assigned to HE received email communications every 2 weeks including information on the same health-related lifestyle domains as HC along with benefits and strategies of lifestyle changes [21].
Statistical Analysis
All data analyses were performed using SPSS 28 (IBM Corp, Armonk, NY). Means, standard deviations, and confidence intervals (95%) were calculated for baseline demographics, anthropometric variables, and dependent variables. An independent samples t-test was used to determine if there were differences in baseline variables between HC and HE groups. A 2x2 mixed factorial ANOVA (intervention x time) was utilized to determine if differences in physical function scores collected at Time 1 and Time 2 were dependent on intervention group (HC or HE). Participants with missing data points in a dependent variable were excluded from data analysis of that variable. An alpha level of .05 was used for all analyses.
Relevant assumptions were checked prior to inferential statistical analyses. Normality was assessed using Shapiro-Wilks tests with the distribution of data in several cells being found to be significantly different from normal distribution (p < .05). However, skewness and kurtosis values were not extreme and the assumption of homogeneity of variance (HOV) was met in all cases. Since normality was violated, HOV was checked for each dependent variable using a Brown-Forsythe test and in all cases, the assumption of HOV was met (p > .05). ANOVA is robust to violations of normality in this context [36].
Results
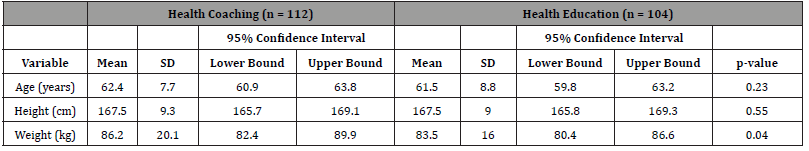
A total of 216 participants completed Time 1 testing for this study (female =157; male=59) with a total of 187 participants completing Time 2 (female = 133; male = 54) for an 87% attrition rate over 12-months. Overall sample demographic statistics are presented in (Table 1). Independent samples t-test revealed there were no Time 1 differences in BMI (t(214)=1.23, p=.22), total body fat percentage (t(214)=0.15, p=.68), hand grip (t(214)=.065, p=.95), chair stands (t(214)=-0.97, p=.33), habitual walk (t(214)=- 1.1, p=.27), 6-minute walk (t(214)=1.5, p=.143), or SPPB scores (t(214)=.35, p=.73) between groups. Independent samples t-test showed that there was a significant difference in Time 1 tandem stands between groups with HC performing significantly better when compared to HE (t (212) =-2.1, p<.05).
Table 1:Baseline Demographic Descriptive Statistics (n = 216).
Mean scores for anthropomorphic statistics for HC and HE from Time 1 to Time 2 are presented in (Table 2). A 2x2 mixed factorial ANOVA showed no statistically significant interaction effect of body weight (F (1,184) =.03, p=.87), BMI (F (1,184) =.10, p=.75), or total body fat percentage (%BF) (F (1,177) =.09, p=.77) between groups. An overall main effect for time was observed for lean body mass (LBM) (F (1,177) =8.0, p<.05, ηp2=.04), with both groups increasing LBM from Time 1 to Time 2.
Table 2:Anthropomorphic Statistics.

Physical function variables with mean scores from Time 1 to Time 2 are presented in (Table 3). All participants who completed assessments were able to complete 10 seconds of a side-by-side stand at Time 1 and Time 2. Among physical function assessments, 2x2 mixed factorial ANOVAs revealed no statistically significant interaction effects of semi-tandem stands (F(1,183)=.97, p=.33), tandem stands (F(1,181)=.29, p=.59), handgrip (F(1,182)=1.1, p=.30), chair stands (F(1,183)=.43, p=.51), 4m habitual walk (F(1,180)=3.20, p=.08), or SPPB scores (F(1,181)=.06, p=.80). A lack of significant interaction in these variables indicates longitudinal changes in the outcomes were not dependent upon group. It is worth noting that although the time*treatment interaction effect was not significant for a 6-minute walk, pairwise comparison revealed that only HC produced a statistically significant increase from Time 1 to Time 2 (p=.03). Similarly, there was not a significant time*treatment interaction found for 4m walk; however, HC was trending towards a significant interaction (p=.07). Results showed HC decreased time to complete 4m while time to complete for HE remained the same.
Table 3:Physical Function Statistics.
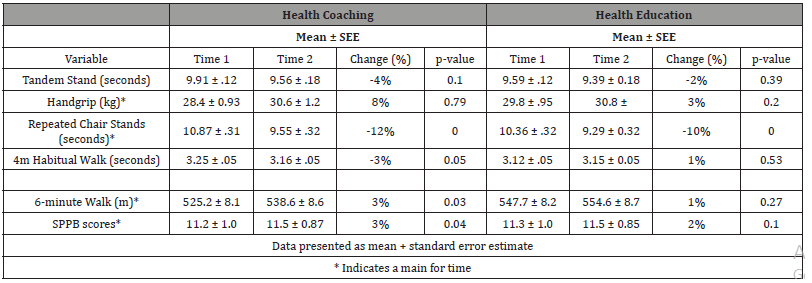
There was an overall main effect for time in total handgrip (F (1,182) =8.49, p<.05, ηp2=.04), chair stands (F (1,183) =39.18, p<.001, ηp2=.18), 6-minute walk (F (1,179) =5.42, p<.05, ηp2=.03), and SPPB (F (1,181) =6.99, p<.05, ηp2=.04). In all variables, both HC and HE significantly improved performance from Time 1 to Time 2.
There were no significant time*treatment interaction or main effects revealed for side-by-side, semi-tandem, or tandem stands.
Discussion
The results of this study suggest that HC and HE interventions have the potential for improving physical function in adults 45- 75 years after 1 year. Previous research suggests an appropriate approach to improve physical function in older adults is to increase physical activity [2-5, 7, 17, 28, 34]. Health coaching is unique in that it allows individuals to set goals based on any health-related lifestyle domains [25, 27]. Previous literature supports the concept that improvement in one or more of these domains may result in improvement in others; however, it is still determined by each individual where their goals are focused [27]. As stated previously, health coaching can improve the health of individuals with chronic diseases and decreasing risk and severity of chronic disease can have a positive impact on physical function [3, 5, 8-10, 24-28].
Although there were no interaction effects found between groups in any dependent variable, it is important to note that in repeated chair stands, 4m habitual walk time, and 6-minute walk distance, HC improved to a greater extent than HE (Table 3). The SPPB is a measure of physical function along with being a tool used to predict fall risk and all-cause mortality in older adults [6,31,32]. Repeated chair stands, a measure of lower extremity power, and 4m habitual walk, a measure of walking speed, are factors in SPPB with the 6-minute walk assessment being a validated predictor of cardiorespiratory fitness [21]. Significant changes in body weight were not observed for HC after 12 months of intervention; however, there was a decrease in %BF accompanied by an increase in LBM among HC participants. Decreasing %BF is another indicator of decreasing risk of chronic disease with increases in LBM suggesting an increase in strength and physical function [13, 37-40]. These findings are further supported by handgrip results. Both HC and HE improved handgrip scores after 12 months, but HC displayed an 8% increase while HE only showed a 3% increase. The improvements observed in repeated chairs stands, 4m habitual walk, 6-minute walk, handgrip, %BF, and LBM could predict improvement in physical function and all-cause mortality risk in HC to a greater extent than HE [6, 31, 32].
While health coaching has been studied more extensively in previous years, few studies have used health education as an intervention for improving health-related outcomes. Health education was provided in the form of periodic email communications including information on how HE participants could improve health-related lifestyle domains. Health education is commonly used in conjunction with health coaching interventions or physical activity interventions, similar to the current investigation [14, 21, 41]. This investigation and others have found similar results in that health education is beneficial in improving health and physical function, albeit with a smaller impact when compared to individuals who had more personalized attention through health coaching [14, 41].
A limitation of the current study is it is part of a larger study investigating the benefits of health coaching in individuals who are at-risk for AD [21]. Risk factors for AD include cognitive and physical health-related risks. This created a population of participants who displayed no physical health-related risk and some who did have physical health-related risks (diabetes, hypertension, hyperlipidemia, or obesity). Another limitation of this study was the broad age range of participants included in analysis. It has been shown that physical function decline occurs every decade after the young adult years making interventions to prevent decline as early as middle-age crucial to maintaining physical function later in life [4, 10, 15-17, 42]. Baseline physical function in middle-aged adults is higher than that of an older adult [2, 43]. Combining these populations in final analyses could explain the lack of significant changes after 12 months of intervention. Lastly, a “standard of care” intervention was utilized for this study. HE participants received educational emails every 2 weeks on improving health-related lifestyle domains. Since the purpose of the larger study (DC MARVel) is to examine the effects of health coaching on AD-risk, the participants of the study were motivated to mitigate AD risk with even those in HE is being motivated to take the education provided and put it into practice. These limitations could have potentially impacted the performance outcomes for the physical function variables. In conclusion, both HC and HE demonstrated improvements in physical function in adults 45-75 after 12 months of intervention. Future studies should examine those free of chronic disease, middle-aged adults or older adults separately, and investigate the benefits of health education without the intervention of a health coach.
Funding
Grant funding for this study was secured from the National Institutes on Aging by Neurotrack Technologies, Inc (grant number R44AG063672). Otherwise, the authors have no conflicts of interest to declare that are relevant to the content of this article.
Acknowledgement
None.
Conflict of Interest
No Conflict of Interest.
References
- Dyussenbayev A (2017) Age Periods of Human Life. Adv Soc Sci Res J 4(6).
- Yorston LC, Kolt GS, Rosenkranz RR (2012) Physical Activity and Physical Function in Older Adults: The 45 and Up Study. J Am Geriatr Soc 60(4): 719-725.
- Buford TW, Anton SD, Clark DJ, Higgins TJ, Cooke MB, et al. (2014) Optimizing the Benefits of Exercise on Physical Function in Older Adults. PM&R 6(6): 528-543.
- Rebecca Seguin, Michael Lamonte, Lesley Tinker, Jingmin Liu, Nancy Woods, et al. (2012) Sedentary Behavior and Physical Function Decline in Older Women: Findings from the Women’s Health Initiative. J Aging Res: e271589.
- Diana A Santos, Analiza M Silva, Fátima Baptista, Rute Santos, Susana Vale, et al. (2012) Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp Gerontol 47(12): 908-912.
- Rita Pavasini, Jack Guralnik, Justin C Brown, Mauro di Bari, Matteo Cesari, et al. (2016) Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med 14(1): 215.
- Manini TM, Pahor M (2008) Physical activity and maintaining physical function in older adults. Br J Sports Med 43(1): 28-31.
- Moreland B, Kakara R, Henry A (2020) Trends in nonfatal falls and fall-related injuries among adults aged≥ 65 years—United States, 2012–2018. Morb Mortal Wkly Rep 69(27): 875-881.
- Adamo DE, Talley SA, Goldberg A (2015) Age and task differences in functional fitness in older women: comparisons with senior fitness test normative and criterion-referenced data. J Aging Phys Act 23(1): 47-54.
- Oliveira JS, Sherrington C, Amorim AB, Dario AB, Tiedemann A, et al. (2017) What is the effect of health coaching on physical activity participation in people aged 60 years and over? A systematic review of randomised controlled trials. Br J Sports Med 51(19): 1425-1432.
- Walston JD (2012) Sarcopenia in older adults. Curr Opin Rheumatol 24(6): 623-627.
- Lotz M, Carames B (2011) Autophagy and Cartilage Homeostasis Mechanisms in Joint Health, Aging and Osteoarthritis. Nat Rev Rheumatol 7(10): 579-587.
- Fulvio Lauretani, Cosimo Roberto Russo, Stefania Bandinelli, Benedetta Bartali, Chiara Cavazzini, et al. (2003) Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol 95(5): 1851-1860.
- Adam J Santanasto, Nancy W Glynn, Laura C Lovato, Steven N Blair, Roger A Fielding, et al. (2017) Effect of physical activity versus health education on physical function, grip strength and mobility. J Am Geriatr Soc 65(7): 1427-1433.
- Martins LCG, Lopes MV de O, Diniz CM, Guedes NG (2021) The factors related to a sedentary lifestyle: A meta-analysis review. J Adv Nurs 77(3): 1188-1205.
- Park JH, Moon JH, Kim HJ, Kong MH, Oh YH, et al. (2020) Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J Fam Med 41(6): 365-373.
- Barajas-Galindo DE, Arnáiz EG, Vicente PF, Ballesteros-Pomar MD (2021) Effects of physical exercise in sarcopenia. A systematic review. Endocrinol Diabetes Nutr Engl Ed 68(3): 159-169.
- Jimison HB, Hagler S, Kurillo G, Bajcsy R, Pavel M, et al. (2015) Remote health coaching for interactive exercise with older adults in a home environment. In: 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). IEEE: 5485-5488.
- Butterworth S, Linden A, McClay W, Leo MC (2006) Effect of motivational interviewing-based health coaching on employees’ physical and mental health status. J Occup Health Psychol 11(4): 358-365.
- Victoria Carmona-Terés, Iris Lumillo-Gutiérrez, Lina Jodar-Fernández, Teresa Rodriguez-Blanco, Joanna Moix-Queraltó, et al. Effectiveness and cost-effectiveness of a health coaching intervention to improve the lifestyle of patients with knee osteoarthritis: cluster randomized clinical trial. BMC Musculoskelet Disord 16(1): 1-12.
- Michelle Gray, Erica N Madero, Joshua L Gills, Sally Paulson, Megan D Jones, et al. (2022) Intervention for a Digital, Cognitive, Multi-Domain Alzheimer Risk Velocity Study: Protocol for a Randomized Controlled Trial. JMIR Res Protoc 11(2): e31841.
- Huffman MH (2009) Health coaching: a fresh, new approach to improve quality outcomes and compliance for patients with chronic conditions. Home Healthc Now 27(8): 490-496.
- Wong-Rieger D, Rieger FP (2013) Health coaching in diabetes: empowering patients to self-manage. Can J Diabetes 37(1): 41-44.
- Wang L, Mårtensson J, Nygårdh A, Zhao Y (2018) A health coaching self-management programme to improve physical activity, lung function and quality of life in patients with Chronic Obstructive Pulmonary Disease: a randomized controlled trial.
- Kivelä K, Elo S, Kyngäs H, Kääriäinen M (2014) The effects of health coaching on adult patients with chronic diseases: a systematic review. Patient Educ Couns 97(2): 147-157.
- Roberto Benzo, Kristin Vickers, Paul J Novotny, Sharon Tucker, Johanna Hoult, et al. (2016) Health coaching and chronic obstructive pulmonary disease rehospitalization. A randomized study. Am J Respir Crit Care Med 194(6): 672-680.
- Jill A Bennett, Nancy A Perrin, Ginger Hanson, Diane Bennett, William Gaynor, et al. (2005) Healthy aging demonstration project: Nurse coaching for behavior change in older adults. Res Nurs Health 28(3): 187-197.
- Julie Williams, Brendon Stubbs, Sol Richardson, Cathy Flower, Lucy Barr-Hamilton, et al. (2019) ‘Walk this way’: results from a pilot randomised controlled trial of a health coaching intervention to reduce sedentary behaviour and increase physical activity in people with serious mental illness. BMC Psychiatry 19(1): 287.
- Park E, Kim H (2015) Experience of Late–Middle-Aged Women who Reside in Small and Medium-Sized Cities in Becoming Psychologically Mature Women. Osong Public Health Res Perspect 6(3): 159-163.
- Gray M, Glenn JM, Binns A (2016) Predicting sarcopenia from functional measures among community-dwelling older adults. Age 38(1): 22.
- JM Guralnik, EM Simonsick, L Ferrucci, RJ Glynn, LF Berkman, et al. (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49(2): M85-M94.
- Fulvio Lauretani, Andrea Ticinesi, Luciano Gionti, Beatrice Prati, Antonio Nouvenne, et al. (2019) Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exp Res 31(10): 1435-1442.
- Rikli RE, Jones CJ (2013) Senior Fitness Test Manual. Human kinetics.
- Glenn JM, Gray M, Binns A (2015) The effects of loaded and unloaded high-velocity resistance training on functional fitness among community-dwelling older adults. Age Ageing 44(6): 926-931.
- Rikli RE, Jones CJ (1999) Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act 7(2): 129-161.
- Schmider E, Ziegler M, Danay E, Beyer L, Bühner M (2010) Is it really robust? Methodology 6(4): 147-151
- Ahmed Elhakeem, Kimberly Hannam, Kevin C Deere, April Hartley, Emma M Clark, et al. (2018) Physical activity producing low, but not medium or higher, vertical impacts is inversely related to BMI in older adults: findings from a multicohort study. J Gerontol Ser A 73(5): 643-651.
- Ferreira RS, da Silva Coqueiro R, Barbosa AR, Pinheiro PA, Fernandes MH, et al. (2013) Relationship between BMI and physical performance among older adults. Geriatr Nur (Lond) 34(6): 465-468.
- Woo J, Leung J, Kwok T (2007) BMI, body composition, and physical functioning in older adults. Obesity 15(7): 1886-1894.
- Lijing L Yan, Martha L Daviglus, Kiang Liu, Amber Pirzada, Daniel B Garside, et al. (2004) BMI and health-related quality of life in adults 65 years and older. Obes Res 12(1): 69-76.
- Seongryu Bae, Sangyoon Lee, Sungchul Lee, Songee Jung, Keitaro Makino, et al. (2019) The effect of a multicomponent intervention to promote community activity on cognitive function in older adults with mild cognitive impairment: a randomized controlled trial. Complement Ther Med 42: 164-169.
- Adamson S, Lorimer R, Cobley JN, Lloyd R, Babraj J, et al. (2014) High Intensity Training Improves Health and Physical Function in Middle Aged Adults. Biology 3(2): 333-344.
- Alden L Gross, Qian-Li Xue, Karen Bandeen-Roche, Linda P Fried, Ravi Varadhan, et al. (2016) Declines and Impairment in Executive Function Predict Onset of Physical Frailty. J Gerontol Ser A 71(12): 1624-1630.
-
Megan D Jones*, Anthony Campitelli, Joshua L Gills, Ray Urbina, Charlie Rodgers, Jenova A Kempkes, Sally Paulson, Jordan M Glenn, Kelsey Bryk, Jennifer Myers, Erica N Madero and Michelle Gray. Effects Of 1-Year Of Health Coaching and Health Education Interventions on Physical Function of Middle Aged and Older Adults. Glob J Aging Geriatr Res. 3(1): 2024. GJAGR.MS.ID.000551.
-
Health Coaching, Health Education, Physical Function, Middle Aged, Older Adults, Aging, Health Behavior, Physical Activity, Intervention Study
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






