 Research Article
Research Article
Atrial Fibrillation in Geriatric Patient at Cardiology Department of General Referral Hospital to Niamey (Niger)
Andia A1*, Riana S2, Saïdou L2, Sorry O2, Daou3 and E adehossi1
1Department of Internal Medicine and Geriatric, General Reference Hospital, Niger
2Department of Cardiology, General Reference Hospital of Niamey, Niger
3Department of Internal Medicine, Hospital of Niamey, Niger
Andia Abdoul Kader, Department of Internal Medicine and Geriatric, General Reference Hospital, Niger.
Received Date:January 27, 2023; Published Date:March 13, 2023
Abstract
Background. Atrial fibrillation (AF) is irregular and very rapid electrical activity in the heart atrium who is the most common arrhythmia in people aged 65 and over. The objective was to determine the clinical, paraclinical and etiological sociodemographic aspects of AF in patients aged 65 and over in the cardiology department of the HGR at Niamey. Methodology. It is a prospective cross-sectional study in the cardiology department of the general referral hospital at Niamey for 3 months, involving all adult patients aged 65 and over. Results a total of 98 patients admitted, 21 were aged 65 and over and 12 patients had AF with a median age of 70 years [65-89 years], a men predominance in 7/12 cases, retired in 7 /12 cases and married in 7/12 cases. The risk factors were physical inactivity (10/12) and hypertension (8/12) while pneumopathy (45%) and treatment discontinuation (45%) were the comorbidities found. the frequent mode of admission was dyspnea at NYHA stage III and lower limb edema in 5/12 cases, dyspnea stage III in 3/12 cases and chest pain in 2/12 cases. The median CHAD2 VASC 2 and HAS BLED scores were 3[2-5] and 2[1-4], respectively
Cardiomyopathy were dilated in 42% frequently ischemic, non-dilated in the same proportion or associated causes and valvulopathy (aortic, mitral and tricuspid) in 16% of cases. Ultrasound showed two (2) cases of pericardial effusion, one (1) frequent intracavitary thrombus. The main complications were stroke and heart failure. Conclusion. AF is the main arrhythmia in geriatrics revealed by comorbidities likes pneumonia and in context of cardiovascular risk factors on the ground of underlying heart disease with a high embolic risk requiring early diagnosis and multidisciplinary management.
Keywords:FA; Geriatrics; Risk factors; Complications; Niamey.
Introduction
Atrial fibrillation (AF) is an irregular and very rapid electrical activity of the atria constituting the most common arrhythmia in elderly aged 65 and over representing 15 to 20% [1]. This age group is characterized by the presence of increasing comorbidities with age, sometimes responsible for an atypical clinical sign [2]. AF is associated with an increased risk of morbidity and mortality such as stroke, heart failure [3-4]. These cardiovascular and metabolic conditions are born of the epidemiological transition on the one hand associated with the persistence of bacterial infections linked to beta hemolytic streptococci responsible for rheumatic valvulopathy on the other hand are the causes of the development of AF compared to the occurrence with the age in sub-Saharan Africa [3-6]. The objective was to determine the clinical, paraclinical and etiological sociodemographic aspects of AF in elderly aged 65 and over in the cardiology department of HGR in Niamey.
Methodology
Elderly people are defined as those who have 65 years old and more; they used to suffer from chronic diseases due limited regenerative abilities and are more susceptible to disease, syndromes, injuries and sickness compared with younger adults. The structural, functional, and molecular levels of their physiology are changes; in fact, in elderly people, most of the major organ system experiences physiological changes. The changes to the nervous system result mostly in cognitive impairments; the cardiovascular system develops higher blood pressures with lower cardiac output; the respiratory system undergoes a reduction of arterial oxyhemoglobin levels the gastrointestinal system experiences delayed gastric emptying and reduction of hepatic metabolism; and the renal system experiences a diminished glomerular filtration rate [3].
Heart failure with preserved ejection fraction (HFPEF) was defined by the presence of symptoms and/or signs of heart failure (HF), elevation of NT proBNP, demonstration of ventricular ejection fraction left atrial (LVEF) > 50%, left atrial dilation assessed (4 chambers or 2 chambers) when left atrial volume is >32 ml/m2, left ventricular hypertrophy (LVH) assessed by mass index left ventricular (LVMI) and the relative parietal thickness (RPT) of the left ventricle, values systematically given by the ultrasound, threshold values 110 g/m2 in men and 95 g/m2 in women. Diastolic dysfunction was assessed by the ratio of the mitral flow pulsed Doppler E wave (synchronous with left ventricular protodiastolic filling) to the tissue Doppler E’ wave recording the spectral pulsed Doppler signal in the myocardium: (E/E’ > 13). Heart failure with impaired ejection fraction was defined by the presence of symptoms and/or signs of HF and LVEF < 40%. We had the authorization of the management of the General Reference Hospital (HGR) of Niamey to conduct this study taking into account the respect of ethics and deontology.
Results
Aspects sociodémographiques des patients ages avec FA Table [1].
Table 1:Sociodemographic aspects of elderly patients with FA.
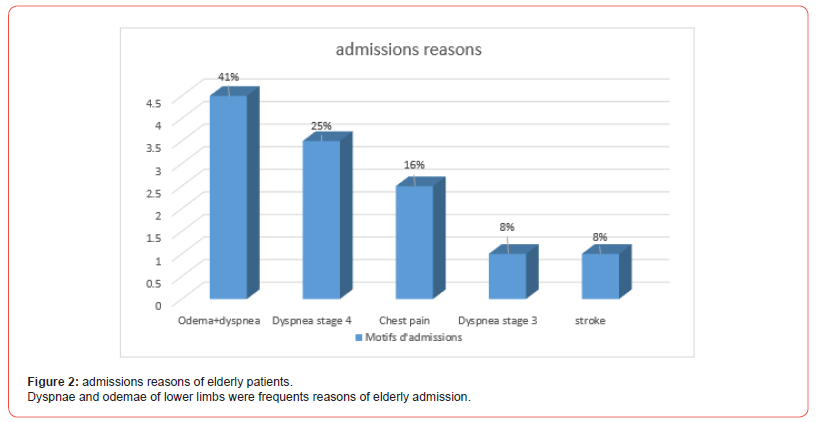
The middle age was 70 years with a major case of married retire 2.2 Associated risk factors.
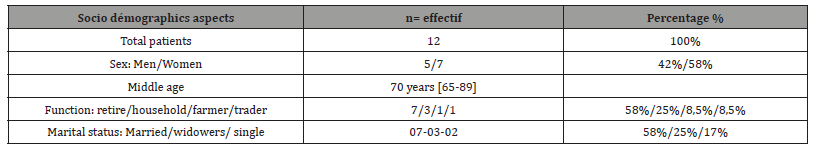
Associated risk factors Figure [1]. Comorbidity
The comorbidity factor associated of FA were: pneumonia (45%), stop treatment (45%) and anemia (10%).
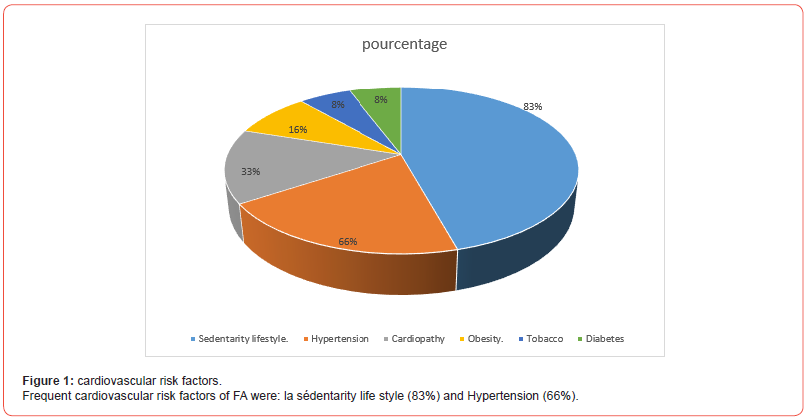
Admission complaints Figure [2]. Biologics aspects. hemorrhagic and embolic risk
The median CHAD2 VASC 2 embolic risk score was 3[2-5] while that of the HAS BLED hemorrhagic risk was 2[1-4].
Socio-demographics, clinics and imagery aspects of elderly FA patient by etiology.
The etiologies frequently found on echocardiography are dilated cardiomyopathies in 5/12 cases including (2 ischemic, 2 mixed and 1 unknown) more common in the 65-70 age group. Nondilated cardiomyopathies were also found in 5/12 cases including (2 ischemic, 2 hypertensive and 1 mixed) frequent in the 65-70 age group.
The valvulopathies found were aortic insufficiency (1 case) and mitral insufficiency more tricuspid (1 case) without predominance without preponderance of sex and age. The ventricular ejection fraction was average (40-50%) in 7/12 cases, altered in 5/12 cases and concerns dilated, non-dilated cardiomyopathy and valvulopathy respectively in 5/12 cases, 5/12 and 2/12 cases.
Associated ultrasound Abnormalities
These are the pericardial effusion found in one (1) case of DMC and three (3) thrombi both in DMC and non-dilated and one (1) intraventricular septal aneurysm in aortic insufficiency. Two (2) cases of minimal aortic and tricuspid insufficiency were found in the non-dilated cardiomyopathies.
Embolic and bleeding risk scores
The median CHADS VASC 2 score was 3 [2-5] preponderant in dilated and non-dilated cardiomyopathies with a score of 5 respectively. The median HAS BLED hemorrhagic risk was 2[1-4] and preponderant in dilated cardiomyopathies with at 5 score.
Discussion
The hospital prevalence of patient aged 65 and over in cardiology was 21/98 (21%), that of FA was 12% and the prevalence in geriatrics was (12/21 = 57%). The average age of our study patient was 70 years [60-89 years]. In the general population over the age of 70 in Tanzania, FA was 0.7% and the hospital prevalence in the cardiology department was 7.8% with an average age of 68 years characterized by women preponderance and a trend increasing with age [7-8]. In the United Kingdom, Majjed et al found in the age group 70-74 years a prevalence of FA was 4.6% in men and 3.3% in women and could reach more than 10% in women and men over 85 years old [9]. In Europe the prevalence is higher and varied from 6.9 %, 5.4% and 10% beyond 85 years respectively for the age group of 70-74 years, in men and women and both sexes over 85 years [10].
In African American subjects in the USA, Go As and coll found the same proportions as Majeed and coll but much less in the age group of 70-79 years and over 80 years in black Americans [11]. The women prevalence of FA and the increase with age was reported in sub-Saharan Africa by some authors without generalizing the fact because of the limited number of studies [12-14]. The size of the different samples, the different means of diagnosis, in particular ischemia, could be the cause of this disparity.
Frequent risk factors in our study were hypertension (66%), obesity (16%) and diabetes (8%). In the study of Dewhurst MJ and coll in Tanzania, hypertension defined by a value of 140/90 mm Hg was found in 70% of cases [7] and corroborates the review of the Sub-Saharan literature which reports a prevalence of 10 to 70% in the general population [15-16]. Diabetes was found in 8% of cases in our study, while its prevalence varies from 2.9 to 33% respectively in the study of Diallo in Mali [16] and Shavadia in Kenya [17]. The prevalence of obesity with a body mass index over or equal to 25 ranged from 5.5 to 48.1% in sub-Saharan Africa [3]. In our study, a sedentary lifestyle (83%) and smoking (8%) had been reported and could lead to an increased risk of developing FA.
The etiological factors in our study were heart disease (33%) reported at the interview, cardiomyopathy (83%) frequently ischemic and valvulopathy (16%). Underlying cardiomyopathies were reported in 20% and valvular heart disease reported in 12 to 44.4% in the general population of Sub-Saharan Africa [3,18]. Myocardial ischemia is the mechanism frequently reported in the literature and ranged from 2.7 to 22.9% in Sub Saharan general [19,20]. The complications of FA in our study were, heart failure (41.6%), stroke (8%) and three (3) cases of intracavitary thrombus while in sub-Saharan Africa heart failure was reported in 60%, in old and recent stroke (2.4 to 33.8%) and intracavitary thrombus in 15 to 30% of cases [3].
Conclusion
FA in the elderly patient is associated with comorbidities such as pneumonia on the grounds of hypertension, diabetes or underlying heart disease which may be complicated by ischemic visceral attack or heart failure.
Acknowledgement
None.
Conflict of Interest
None.
References
- A Da Costa, C Roméyer-Bouchard, L Bisch, L Khris, K Isaaz, et al. (2009) La fibrillation auriculaire : Enjeux épidémiologiques, définition, nosologie, médico-é Ann Cardiol Angeiol 58(1): S3-S5.
- Cynthia Barbraud (2016) Prise en charge des arythmies chez les patients âgé Louvain med 135(10): 709-712.
- Noubiap JJ, Nyaga UF (2019) A review of the epidemiology of atrial fibrillation in sub‐Saharan Africa. J Cardiovasc Electrophysiol 30(12): 3006-3016.
- SS Chugh, R Havmoeller, K Narayanan, D Singh, M Rienstra, et al. (2014) Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129(8): 837‐847.
- GA Roth, MH Forouzanfar, AE Moran, R Barber, G Nguyen, et al. (2015) Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med 372(14): 1333‐1341.
- Mendis S, Puska P, Norrving B (2011) Global Atlas on Cardiovascular Disease Prevention and Control. Geneva, Switzerland: World Health Organi- zation: 155 p.
- MJ Dewhurst, PC Adams, WK Gray, F Dewhurst, GP Orega, et al. (2012) Strikingly low prevalence of atrial fibrillation in elderly Tanzanians. J Am Geriatr Soc 60(6): 1135‐1140.
- IO Oyediran, S Prattipati, FM Sakita, GL Kweka, TG Tarimo, et al. (2021) The prevalence, management, and thirty-day outcomes of symptomatic atrial fibrillation in a Tanzanian emergency department. Afr J Emerg Med 11(4): 404-409.
- M Connor, P Rheeder, A Bryer, M Meredith, M Beukes, et al. (2005) The South African Stroke Risk in General Practice Study. S Afr Med J 95(5): 334-339.
- J Heeringa, DAM van der Kuip, A Hofman, JA Kors, G van Herpen, et al. (2006) Prevalence, incidence and lifetime risk of atrial fibrillation: The Rotterdam Study. Eur Heart J 27(8):949-953.
- AS Go, EM Hylek, KA Phillips, Y Chang, LE Henault, et al. (2001) Prevalence of diagnosed atrial fibrilla- tion in adults: National implications for rhythm management and stroke prevention: The Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 285(18): 2370-2375.
- Majeed A, Moser K, Carroll K (2001) Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994–1998: Analysis of data from the general practice research database. Heart 86(3): 284-288.
- M Ntep-Gweth, M Zimmermann, A Meiltz, S Kingue, P Ndobo, et al. (2010) Atrial fibrillation in Africa: Clinical characteristics, prognosis, and adherence to guidelines in Cameroon. Europace 12(4): 482-487.
- K Sliwa, MJ Carrington, E Klug, L Opie, G Lee, et al. (2010) Predisposing factors and incidence of newly diagnosed atrial fibrillation in an urban African community: Insights from the Heart of Soweto Study. Heart 96(23): 1878-82.
- Goma FM, Kalinchenko S (2015) Atrial fibrillation in Lusaka–Pathoaetiology, pathophysiology and clinical management challenges in primary care settings. Med J Zambia 42(1): 31-41.
- Diallo K 2015 Aspects cliniques et évolutifs de la fibrillation atriale non valvulaire dans le service de cardiologie du CHU Point‐G. Thesis.
- J Shavadia, G Yonga, S Mwanzi, A Jinah, A Moriasi, et al. (2013) Clinical characteristics and outcomes of atrial fibrillation and flutter at the Aga Khan University Hospital, Nairobi. Cardiovasc J Afr 24(2): 6-9.
- MU Sani, BA Davison, G Cotter, BM Mayosi, C Edwards, et al. (2018) Prevalence, clinical characteristics and outcomes of valvular atrial fibrillation in a cohort of African patients with acute heart failure: insights from the THESUS‐HF registry. Cardiovasc J Afr 29(3): 139-145.
- A Mbaye, S Pessinaba, M Bodian, BN Mouhamadou, F Mbaye, et al. (2010) Atrial fibrillation, frequency, etiologic factors, evolution and treatment in a cardiology depart- ment in Dakar, Senegal. Pan Afr Med J 6 : 16.
- Sacca-Vehounkpe J, Tchabi Y, Hounton N, Hounkponou M, Assani S, et al. (2016) Facteurs de risque de la fibrillation atriale en cardiologie au CNHU de Cotonou (2010‐2014). Journal de la Société de Biologie Clinique du Bénin 24: 52-55.
-
Andia A*, Riana S, Saïdou L, Sorry O, Daou and E adehossi. Atrial Fibrillation in Geriatric Patient at Cardiology Department of General Referral Hospital to Niamey (Niger). Glob J Aging Geriatr Res. 2(2): 2023. GJAGR.MS.ID.000534.
-
Heart atrium, Methodology, Hypertension, Cardiomyopathy, Atypical clinical sign, Beta hemolytic streptococci
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






