 Research Article
Research Article
Association Between Albuminuria and Left Ventricular Structural Changes in Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study from a Tertiary Hospital in Malaysia
Nor Izzati Saedon1, Firdaus Hadi2, Imran Zainal Abidin2 and Nur Izyan Diyana Bt Md Nasir1,2
1Geriatric Unit, Department of Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
2Cardiology Unit, Department of Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
Nor Izzati Saedon, Geriatric Unit, Department of Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
Received Date:June 18, 2025; Published Date:July 17, 2025
Abstract
Background: Albuminuria is increasingly recognized as a predictor of cardiovascular morbidity and mortality in patients with type 2 diabetes
mellitus (T2DM), independent of traditional risk factors. However, the relationship between albuminuria and early echocardiographic markers of
cardiac structural changes, particularly interventricular septal thickness in diastole (IVSd), remains underexplored in Southeast Asian populations.
Objective: To determine the association between urine albumin-creatinine ratio (UACR) and echocardiographic indices of cardiac structure and
function among diabetic patients in a Malaysian tertiary care setting.
Methods: This was a cross-sectional study involving 82 adults with T2DM and preserved renal function (eGFR ≥60 mL/min/1.73m²) who
underwent echocardiography and UACR testing within six months at University Malaya Medical Centre (UMMC). Echocardiographic parameters
included IVSd, left ventricular internal diameter at diastole (LVIDd), left ventricular ejection fraction (LVEF), tricuspid annular plane systolic
excursion (TAPSE), and left ventricular diastolic dysfunction (LVDD) grade. Associations were analyzed using multivariable linear and ordinal
regression.
Results: Patients with higher UACR levels had significantly increased IVSd values (p = 0.014). UACR was an independent predictor of IVSd in
multivariable regression (β = 0.001, p = 0.006). No significant associations were found between UACR and LVIDd, LVEF, TAPSE, or LVDD severity
after adjusting for confounders.
Conclusion: UACR is independently associated with interventricular septal thickening, suggesting early structural cardiac remodelling in T2DM
patients. Routine measurement of UACR may aid in cardiovascular risk stratification, particularly in settings where echocardiography is not readily
available.
Keywords:Albuminuria, Urine Albumin-Creatinine Ratio, Type 2 Diabetes Mellitus, Interventricular Septal Thickness, Echocardiography, Cardiac Remodelling
Introduction
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality among individuals with type 2 diabetes mellitus (T2DM), accounting for over 50% of deaths in this population worldwide [1]. Among the numerous markers of cardiovascular risk in diabetes, albuminuria-defined as the presence of albumin in urine at micro- or macro- levels-has emerged not only as a predictor of progressive diabetic nephropathy but also as an independent risk factor for cardiovascular events and all-cause mortality [2, 3].
The urine albumin-creatinine ratio (UACR) is a validated, practical surrogate for quantifying albuminuria. Beyond its renal implications, UACR reflects systemic endothelial dysfunction, a pathophysiological hallmark of both atherosclerosis and myocardial remodelling [4, 5]. Indeed, studies have consistently shown that microalbuminuria correlates with subclinical cardiac abnormalities such as left ventricular hypertrophy (LVH) and diastolic dysfunction, which often precede overt heart failure [6-8]. Echocardiography remains the cornerstone for evaluating cardiac structure and function, with metrics such as interventricular septal thickness in diastole (IVSd) and left ventricular internal diameter (LVIDd) providing reliable indicators of early remodelling. Among these, IVSd is a sensitive early marker of concentric hypertrophy, especially in diabetic populations where subclinical myocardial changes may remain undetected without imaging [9].
Despite the global recognition of albuminuria as a cardiovascular risk marker, data on its relationship with echocardiographic indices-particularly in Southeast Asian diabetic populations-are limited. Malaysia, where the prevalence of diabetes exceeds 18.3% in adults aged ≥18 years [10], represents a critical setting to evaluate such associations. Understanding whether albuminuria corresponds with early echocardiographic markers of structural heart disease may offer a low-cost, non-invasive strategy to enhance risk stratification and guide timely therapeutic intervention. This study aimed to evaluate the association between UACR and echocardiographic markers of cardiac structure and function-specifically IVSd, LVIDd, and parameters of systolic and diastolic function-among patients with T2DM in a Malaysian tertiary care setting.
Methods
Study Design and Setting
This cross-sectional observational study was conducted at the University Malaya Medical Centre (UMMC), a leading academic tertiary referral hospital in Kuala Lumpur, Malaysia. The study was carried out between January 1, 2020, and December 31, 2021, and adhered to the principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the UMMC Medical Research Ethics Committee (MREC) [Protocol ID: Insert Reference Number].
Study Population and Eligibility Criteria
We screened adult patients aged 18 to 65 years with a confirmed diagnosis of type 2 diabetes mellitus (T2DM) based on HbA1c ≥6.3% or documented use of anti-diabetic therapy. Eligible patients must have undergone a transthoracic echocardiogram (TTE) and a urine albumin-creatinine ratio (UACR) measurement within six months of each other. To ensure assessment of early structural cardiac changes without confounding from advanced renal disease, we included only those with preserved renal function (estimated glomerular filtration rate [eGFR] ≥60 mL/min/1.73m² as calculated by the CKD-EPI equation).
Patients were excluded if they had:
• Acute or chronic urinary tract infections,
• Pregnancy,
• Known history of end-stage renal disease,
• eGFR <60 mL/min/1.73m²,
• Congenital or structural heart disease not related to T2DM.
Many retirees also re-enter the work force for financial reasons. It is possible that they may be moving into new jobs, new industries and also possibly doing so for lower pay and fewer benefits. As such, entrepreneurship, including self-employment and bridge employment, offers an important opportunity for older adults who have left their main work chapter.
Data Sources and Collection Procedure
Data were extracted retrospectively from UMMC’s electronic
medical records and echocardiography databases. Collected variables
included:
• Demographics: Age, sex, ethnicity, weight, height, BMI, smoking
status
• Clinical history: Duration of diabetes, presence of hypertension,
dyslipidemia, coronary artery disease, and heart failure
• Medication use: ACE inhibitors, ARBs, ARN inhibitors, diuretics,
insulin, and oral antidiabetic agents
• Laboratory data: HbA1c, serum creatinine, UACR
UACR values were classified according to KDIGO guidelines:
• Normal to mildly increased: <3 mg/mmol
• Moderately increased: 3-30 mg/mmol
• Severely increased: >30 mg/mmol
Echocardiographic Assessment
All echocardiograms were performed using standardized protocols
by trained echocardiographers using Philips iE33 ultrasound
systems. Interpretations followed the American Society of Echocardiography
(ASE) guidelines. Parameters assessed included:
• Interventricular septal thickness in diastole (IVSd)
• Left ventricular internal diameter in diastole (LVIDd)
• Left ventricular ejection fraction (LVEF), calculated using the
biplane Simpson’s method
• Tricuspid annular plane systolic excursion (TAPSE) as a surrogate
for right ventricular function
• Left ventricular diastolic dysfunction (LVDD) grading, categorized
as normal, grade I, II, or III dysfunction based on E/A ratio,
e’, and left atrial volume index
Measurement reliability was ensured by using a single blinded reviewer to extract echocardiographic data. Inter-observer variability was not applicable due to the use of archived final reports.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, USA). Continuous variables were assessed for normality using the Shapiro-Wilk test. Normally distributed variables were expressed as mean ± standard deviation (SD), while non-normally distributed variables were reported as median with interquartile range (IQR). Between-group comparisons were made using one-way ANOVA or Kruskal-Wallis tests, as appropriate. Categorical variables were summarized as frequencies and percentages, and differences across groups were assessed using the chi-square or Fisher’s exact test.
Multivariable linear regression models were constructed to assess the independent association between UACR and echocardiographic parameters (IVSd, LVIDd, LVEF, TAPSE). For ordinal outcomes such as LVDD grade, multivariable ordinal logistic regression was used. All models were adjusted for potential confounders, including age, sex, BMI, hypertension, diabetes duration, and medi cation use. Multicollinearity was assessed using variance inflation factors (VIF), and model fitness was verified with residual plots and adjusted R². A two-tailed p-value of <0.05 was considered statistically significant.
Results
Participant Characteristics
A total of 82 patients with type 2 diabetes mellitus (T2DM) and
preserved renal function (eGFR ≥60 mL/min/1.73 m²) were included
in the analysis. Participants were stratified into three groups
based on their urine albumin-creatinine ratio (UACR):
• Normal to mildly increased (<3 mg/mmol, n = 28)
• Moderately increased (3-30 mg/mmol, n = 35)
• Severely increased (>30 mg/mmol, n = 19)
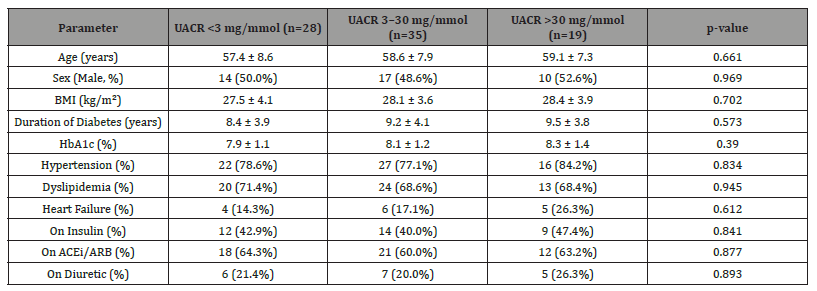
Baseline demographic and clinical characteristics were comparable across UACR groups (Table 1). The mean age ranged from 57.4 to 59.1 years across groups, with balanced gender distribution. There were no significant differences in BMI, duration of diabetes, glycemic control (HbA1c), or comorbidity burden, including hypertension, dyslipidemia, or heart failure. Likewise, medication use including insulin, ACEi/ARB, and diuretics was similar across the groups (all p > 0.05). Insert Table 1 here
Table 1:Echocardiographic Characteristics by UACR Group.
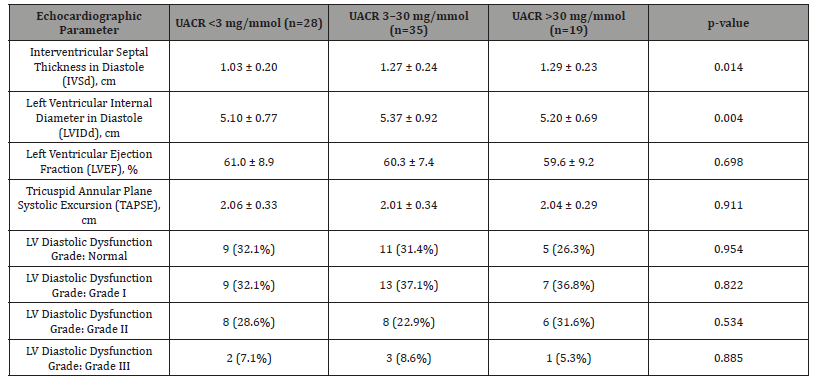
Echocardiographic Differences Across UACR Groups
Table 2 summarizes key echocardiographic findings stratified
by UACR category. A significant trend was observed for interventricular
septal thickness in diastole (IVSd), which progressively increased
across UACR groups:
• 1.03 ± 0.20 cm in the <3 mg/mmol group
• 1.27 ± 0.24 cm in the 3-30 mg/mmol group
• 1.29 ± 0.23 cm in the >30 mg/mmol group (p = 0.014)
Insert Table 2 here
Table 2:Association Between UACR and Echocardiographic Parameters.
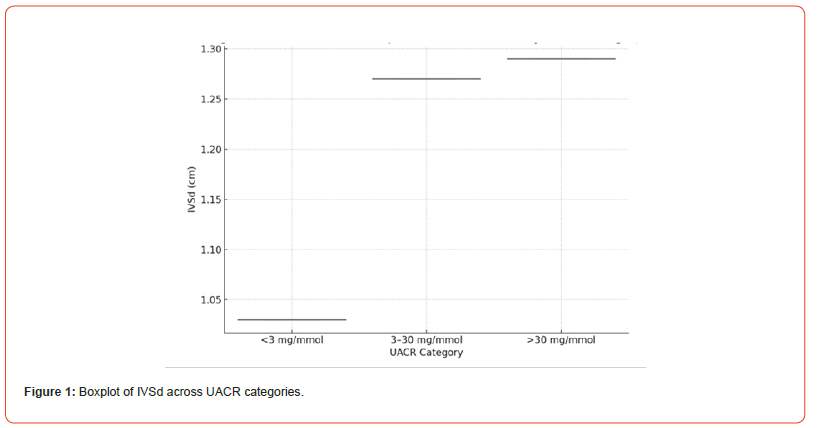
This trend is further illustrated in Figure 1, where a boxplot demonstrates clear septal hypertrophy with increasing levels of albuminuria. Left ventricular internal diameter in diastole (LVIDd) showed a significant difference among groups (p = 0.004), with the highest mean observed in the moderately increased UACR group. However, the pattern was not linear. No significant differences were noted in left ventricular ejection fraction (LVEF) or tricuspid annular plane systolic excursion (TAPSE), suggesting preserved systolic function across all strata. There was also no significant variation in the distribution of left ventricular diastolic dysfunction (LVDD) grades across the UACR groups (all p > 0.05), with Grade I dysfunction being the most common across all categories. Insert Figure 1 Here
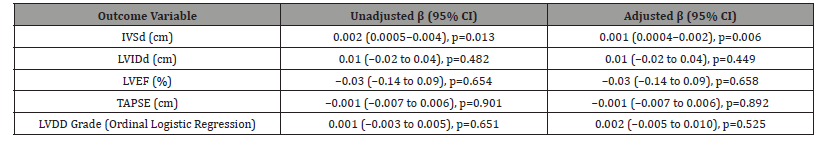
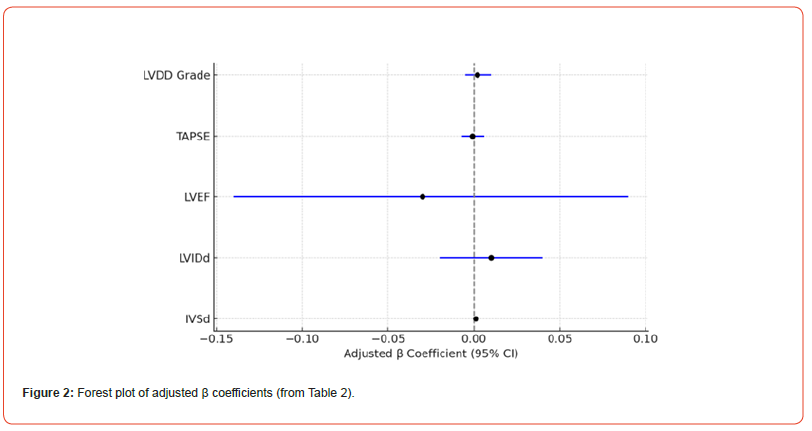
Multivariable Analysis of UACR and Echocardiographic Outcomes
Table 3 presents result from the multivariable linear and ordinal logistic regression analyses examining associations between UACR and echocardiographic parameters. In both unadjusted and adjusted models, UACR was significantly associated with increased IVSd. In the adjusted model (accounting for sex, weight, and diuretic use), the β coefficient for IVSd was 0.001 (95% CI: 0.0004-0.002; p = 0.006), confirming UACR as an independent predictor of myocardial septal thickening. There were no statistically significant associations between UACR and LVIDd, LVEF, or TAPSE in adjusted models. Similarly, UACR was not associated with LVDD grade (adjusted β = 0.002, 95% CI: -0.005 to 0.010; p = 0.525). These results are visually summarized in Figure 2, a forest plot depicting the adjusted β coefficients and 95% confidence intervals across all echocardiographic parameters studied. Insert Table 3 and figure 2 here
Table 3:Baseline Clinical and Demographic Characteristics by UACR Group
Discussion
This cross-sectional study evaluated the relationship between urine albumin-creatinine ratio (UACR) and echocardiographic parameters of cardiac structure and function among patients with type 2 diabetes mellitus (T2DM) and preserved renal function. The primary finding is the robust, independent association between UACR and interventricular septal thickness in diastole (IVSd), even after adjusting for relevant clinical confounders. No significant associations were identified between UACR and systolic function indices (LVEF, TAPSE) or left ventricular diastolic dysfunction (LVDD) grade.
Our findings support the hypothesis that albuminuria reflects not only microvascular damage at the renal level but also early myocardial remodelling. Previous studies have linked albuminuria to left ventricular hypertrophy (LVH), particularly in the context of diabetes and hypertension [1, 2]. The observed increase in IVSd in our cohort aligns with these reports and may indicate subclinical myocardial hypertrophy, even in the absence of overt heart failure or reduced ejection fraction. Interestingly, while LVIDd differed among groups, the lack of a consistent trend and no significance in multivariate models suggest this may be a transient structural variation rather than a consistent pathological response to increasing albuminuria. Likewise, LVEF and TAPSE were not significantly different across albuminuria strata, reinforcing the notion that systolic function remains preserved in the early remodelling phase.
The absence of a clear relationship between UACR and LVDD grade in our study may be explained by several factors. Diastolic dysfunction is multifactorial and often influenced by aging, glycemic variability, blood pressure, and myocardial fibrosis, factors that may not be fully captured in our regression models. Additionally, echocardiographic grading of diastolic dysfunction is subject to inter-operator variability and may lack sensitivity to detect subtle changes across albuminuria levels. This study adds to the growing body of evidence suggesting albuminuria is an accessible, inexpensive biomarker that could aid in cardiovascular risk stratification in diabetic patients-even in resource-limited settings. The independent association with IVSd highlights the potential of UACR to serve as an early marker of myocardial involvement, prompting further cardiac evaluation or more aggressive risk modification.
Strengths and Limitations
Strengths of this study include the use of quantitative UACR measurement, standardized echocardiographic evaluation, and adjustment for important confounders. However, certain limitations must be acknowledged. First, the cross-sectional nature of the study precludes inference of causality. Second, the modest sample size and single-center setting may limit generalizability. Third, the absence of advanced echocardiographic techniques (e.g., speckle tracking or myocardial strain) restricts our ability to detect subtle systolic or diastolic changes. Future studies should explore longitudinal relationships between albuminuria progression and echocardiographic remodelling, and whether interventions targeting albuminuria (e.g., SGLT2 inhibitors) yield parallel cardiac structural benefits.
Conclusion
In this cohort of T2DM patients with preserved renal function, UACR was independently associated with increased interventricular septal thickness, suggesting early subclinical myocardial remodelling. No associations were observed with global systolic function or diastolic dysfunction severity. Routine measurement of UACR may serve as a practical tool for identifying diabetic patients at risk of early cardiac structural changes, particularly in primary care or low-resource setting.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Low Wang CC, Hess CN, Hiatt WR, Goldfine AB (2016) Clinical update: Cardiovascular disease in diabetes mellitus. Circulation 133(24): 2459-2502.
- H C Gerstein, J F Mann, Q Yi, B Zinman, S F Dinneen, et al. (2001) Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286(4): 421-426.
- Caroline S Fox, Kunihiro Matsushita, Mark Woodward, Henk J G Bilo, John Chalmers, et al. (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: A meta-analysis. Lancet 380(9854): 1662-1673.
- Deckert T, Feldt-Rasmussen B, Borch-Johnsen K, Jensen T, Kofoed-Enevoldsen A (1989) Albuminuria reflects widespread vascular damage. Diabetologia 32(4): 219-226.
- Stehouwer CD, Smulders YM (2006) Microalbuminuria and risk for cardiovascular disease: Analysis of potential mechanisms. J Am Soc Nephrol 17(8): 2106-2111.
- Jennifer E Liu, David C Robbins, Vittorio Palmieri, Jonathan N Bella, Mary J Roman, et al. (2003) Association of albuminuria with systolic and diastolic left ventricular dysfunction in type 2 diabetes. J Am Coll Cardiol 41(11): 2022-2028.
- Parsaee H, Nabati M, Azizi S, Yazdani J (2021) Correlation between albuminuria and left ventricular myocardial performance in type 2 diabetes. J Clin Ultrasound 49(5): 472-478.
- Mehta J, Godbole VY, Mehta KG, Lalithambigai A (2021) Association of microalbuminuria with left ventricular dysfunction in type 2 diabetes. Egypt J Intern Med 33: 1-6.
- Muhammad Hamza, Mishal Fatima, Muhammad Masood, Hafiz Umar Masood, Ghazal Tasleem, et al. (2020) Relationship of left ventricular and atrial dimensions with moderate to severe LV diastolic dysfunction. Afr Health Sci 20(4): 1749-1753.
- Institute for Public Health, National Institutes of Health, Ministry of Health Malaysia. National Health and Morbidity Survey (NHMS) 2019: Non-communicable diseases, healthcare demand and health literacy.






