 Review Article
Review Article
Assessment of Knowledge of Brazilian Health Professionals About Advance Directives: A Systematic Review
Vanessa Cristina Carvalho Castro¹; Juliana Reis Moura Lippo Acioli¹ and Isaura Romero Peixoto²*
1Student of the Medicine Course at Tiradentes, University in Jaboatão dos Guararapes, Brazil
2Post-Graduate Program in Tropical Medicine, Federal University of Pernambuco, Recife, Brazil
Isaura Romero Peixoto, Post-Graduate Program in Tropical Medicine, Federal University of Pernambuco, Brazil.
Received Date:May 31, 2023; Published Date:June 05, 2023
Abstract
Objective: To assess the level of knowledge of Brazilian health professionals about Advance Directives.
Methods: This is a systematic review, carried out in accordance with the Protocol for Systematic Reviews and Meta-Analyses, following the
PICOS strategy. The search for articles was realized in March 2023 in the databases: Scientific Electronic Library Online, Virtual Health Library
and PubMed. For the search, the Health Sciences Descriptors were used: “Advance Directives”, “Living Wills”, “Health Professionals”, “Knowledge”
combined with the AND and OR operators. 1119 records were identified, and 1077 articles were evaluated, of which 5 were included in this review.
Results: Most studies identified gaps in the knowledge of health professionals about Advance Directives, implying less safety in their use.
Conclusion: More research on the subject is needed beyond the medical public in the South and Southeast regions, in addition to publicizing the
Advance Directives, including its legal aspects, in order to provide greater knowledge and, consequently, more security for professionals of health in
implementation of the instrument.
Keywords:Advance directives; Living wills; Health professionals; Knowledge.
Introduction
The Advance Directives (AD) are a set of wishes expressed by the patient in lucid conditions, about the treatments to which he wants or not to be submitted in a moment of advanced and irreversible disease, in which he is not able to express his will. These directives were standardized by Resolution No. 1,995/2012 of the Brazilian Federal Council of Medicine (BFCM) a little over a decade ago and regulating that they are in line with the respect for the dignity of the person, provided for in the Brazilian Federal Constitution of 1988. It provides for the ethically appropriate way to guide patients to participate actively, even if anticipated in the event of their disability, in the decision-making process [1-9]. This document is relevant for preserving the autonomy and dignity of the patient, related to orthothanasia, that is, when death occurs properly, avoiding the use of extraordinary therapeutic measures in order to prolong life without taking into account the quality of life. In addition, the literature addresses that health professionals who have training in end-of-life issues are more confident in care practice and have less moral anguish in the face of many issues that involve this stage [10-15].
Despite this relevance, the insufficient dissemination of this tool in clinical environments is notorious. As an example of this, Guirro et al [15] (2022) identified that only 25% of the health professionals approached in their study were aware of the directives. This lack of adherence can be attributed to the absence of specific brazilian legislation on such a document (although this does not make it invalid), as well as the lack of knowledge about this instrument. Thus, the present study aims to evaluate the knowledge of Brazilian physicians and nurses about AD [3,6,8,16].
Methodology
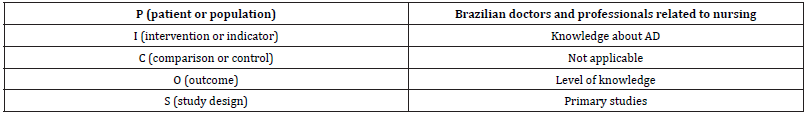
This is a systematic literature review carried out in March 2023 in order to answer the guiding question: “What is the level of knowledge of Brazilian doctors and professionals related to nursing about advance directives?”. To prepare this question, as described in [Table 1], the “PICOS” strategy was used, an acronym whose “P” indicates patient or population; “I”, intervention or indicator; “C”, comparison or control; “O”, outcome; “result”; “S”, study design. The survey was carried out on the platforms: Scientific Electronic Library Online (SciELO), Virtual Health Library (VHL) and PubMed. For the search, the following Medical Subject Headings (MESH) were used: “Advance Directives”, “Living Wills”, “Health Professionals”, “ ”, combined by the Boolean logical operators AND and OR.
Table 1:Application of the PICOS strategy in the present study.
As inclusion criteria, primary studies indexed in the last five years were established, with full text available, in Portuguese, English or Spanish and that answered the guiding question. As exclusion criteria: duplicate studies; surveys that did not address the cited population; articles whose outcome is unrelated to the research question.
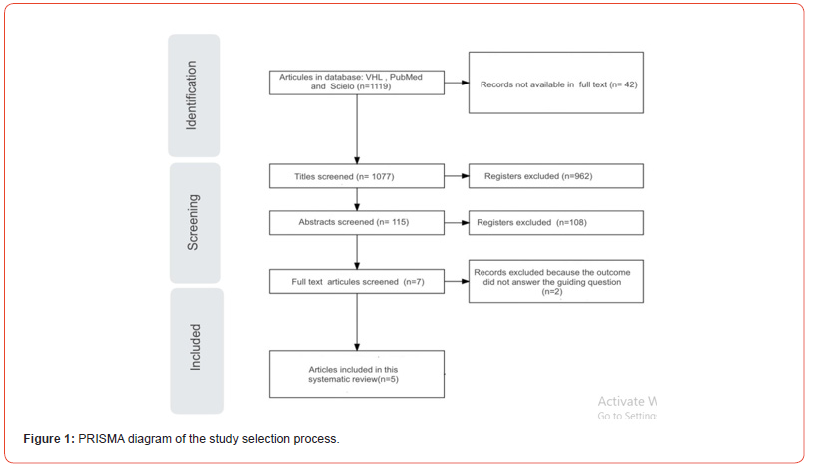
As a result of the search, 1119 studies were obtained, of which 42 were excluded due to the unavailability of full text. From this, the titles of 1077 records were observed, defining, among them, 115 that had their abstracts read. Studies were excluded according to the criteria mentioned above, leaving 7 for full reading. Of these, 5 articles were selected for review, being submitted to data extraction and narrative synthesis for later publication. The process described is illustrated in [Figure 1], which follows the guidelines of the PRISMA 2020 guideline. Furthermore, it is worth noting that the stages of this study were carried out independently by two researchers with the help of a third reviewer to resolve possible disagreements. Finally, this systematic review was submitted on the PROSPERO platform, under ID CRD42023427848. This international Review Article 3 platform is a permanent and prospective record of systematic reviews that have relevant health information as an outcome.
Results
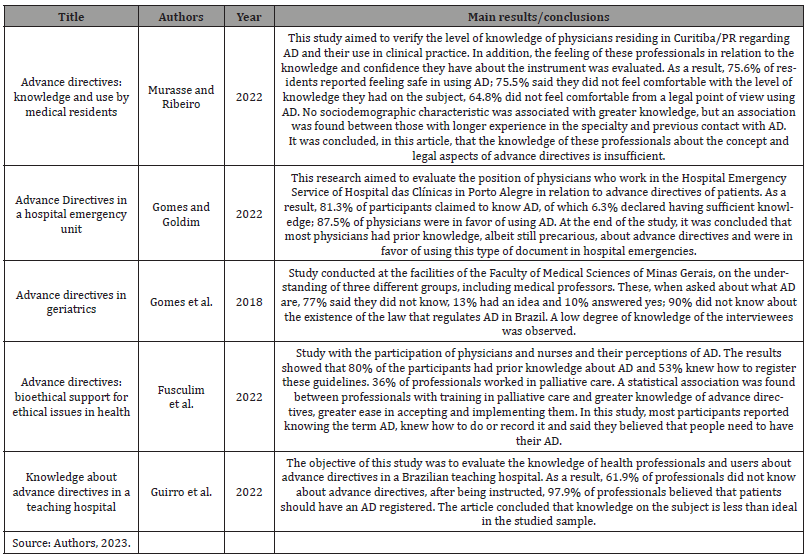
Five studies were found according to the evaluation of the titles, abstracts and keywords previously elucidated, all of which were exploratory and cross-sectional, with a quantitative approach and with a significance level of 5% (p<0.05). About the regions of Brazil, the South region concentrated the largest volume of production, considering that only one article used digital platforms in order to obtain a greater number of participants from different regions, enabling the analysis of different social and cultural realities. and educational. The studies applied in person were carried out both in teaching clinics and in hospital services, with the participation of health professionals, mostly physicians (n=287), but also with the contribution of nurses (n=58) and nursing technicians (n=30). Finally, considering the year of publication of the studies, four were produced in 2022, and one in 2018. All studies found were published in a bioethics journal. The characterization of the articles that made up the body of the research, as well as the main results and conclusions found are presented in [Table 2].
Table 2:Description of selected articles.
Discussion
Knowledge of health professionals about AD and associated factors.
After analyzing the included articles, different levels of knowledge of professionals about Advance Directives were observed. In the studies by Guirro et al (2022) [15] and by Gomes et al [19] (2018), the participants’ lack of knowledge about the topic was observed, since respectively 61.9% and 77.7% of respondents did not know what it was about. On the other hand, two of the reviewed articles described the professionals’ knowledge as “insufficient”, since, despite the majority being aware of the term AD, a large part also did not feel “comfortable” or “secure” regarding their degree of understanding [18,19].
Only one of the studies found knowledge about AD as a reality for most participants. This outcome was associated by the authors with the characteristic of the sample, since the applied form was disclosed on digital platforms, which probably attracted individuals with greater interest and knowledge in the subject [20]. Thus, from the five articles evaluated, it appears, in response to the guiding question of this study, that the knowledge of Brazilian health professionals about AD is mostly low or insufficient. It is reiterated that the lack of a broad understanding about AD can contribute to therapeutic obstinacy in the medical environment, causing the implementation of treatments that will prolong the patient’s life, but without equivalent gain in quality of life. These actions are contrary to respect for the patient’s autonomy and removing it from it place in the care center [15-20].
This evidenced panorama may be a consequence of different causes, such as the lack of approach to these themes in undergraduate courses. This hypothesis can be supported by the finding by Fusculim et al [20] (2022) that most health professionals only had contact with knowledge of palliation and end-of-life care after graduation. This corroborates the need for greater attention from higher education institutions on the subject. This also points to the need for greater regulation of the practice through specific protocols and more publicized by the Federal Council of Nursing and the Federal Council of Medicine [19,20]. Furthermore, two of the surveys performed a statistical analysis of responses in search of possible factors that favored satisfactory levels of knowledge about AD. Both pointed out that a greater understanding of palliative care would be one of these factors. This relationship cof explained by the hypothesis that, by acting in situations in which finitude and terminality of life are much discussed, it is possible that professionals with greater experience in palliative care have more contact with complex end-of-life situations and, therefore, have greater affinity with AD [18,20].
However, although this relationship is understandable, it denounces a simplistic view of application of AD. Because, by favoring communication and stimulating autonomy and dignity of the patient, these directives should also be used in other specialties and regardless of the stage of the disease in which the patient is, not restricted to the scope of palliation [18,20]. Furthermore, in three of the included studies, the majority (60 to 83%) of health professionals interviewees never had clinical contact with the living will and also had knowledge insufficient about AD. This observation reinforces the finding of the study conducted by Fusculim et al [20] (2022), who highlighted that one of the factors associated with greater knowledge about AD would be prior contact with some advance directive in clinical practice.
The widely observed lack of previous contact may be related to the fact that the AD have not yet managed to be effectively integrated into the Brazilian reality, still suffering barriers to its use, whether they are the population’s lack of knowledge, cultural issues and also the legal ones. This data also allows the assumption that one of the strategies to be used in the teaching of AD may be the simulation of clinical situations. This simulated scenario would help to promote the knowledge and application skills of AD, supplying, momentarily, the absence of practical experience. Despite the fact that knowledge is still insufficient, it is notable that some studies suggest the possibility of change in this scenario by pointing out that, after being instructed to, the majority (ranging from 87.5 to 98%) of the participants demonstrated to find the directives relevant advances of will to patients. So, a relevant portion of respondents (43% to 73.2%) expressed interest in creating their own directives [15,17,19,20]. This evidence weakens the possibility that lack of knowledge about AD is linked to the professional’s lack of interest or the belief in their irrelevance by these professionals. For the contrary, since the exposure to initial concepts about the directives raised the recognition of its relevance. Added to this, the fact that the studies observed receptivity and interest from the majority (88 to 98%) of participants to learn more about the topic, thus reinforcing the need for institutional programs that efficiently address the issue [18,20].
Knowledge about the legal aspects of AD and security for its application
From the legal point of view of AD, in addition to being provided for in Resolution BFCM nº 1.995/2012, their use is supported by the Federal Constitution, in its article 5, which establishes autonomy as a fundamental right, and in the Civil Code, in its article 15, which guarantees patient participation and the possibility of consenting or not to medical treatments. Furthermore, it is important to point out that the Brazilian Statute of the Elderly, Law 10.741/2003, guarantees the participation of people over 60 years of age in situations of medical care [21-23]. It is also essential to remember that the BFCM can establish routines and procedures that allow the proper practice of medicine, since it has the legal attribution to provide for the ethical performance of medicine in accordance with Law 3.268/1957. This can be seen, as an example, through Resolution BFCM 2168/2017, in the area of assisted reproduction, and through Resolution BFCM 2173/2017, regarding the criteria for the diagnosis of brain death [24,25].
Of the five articles selected, four of them questioned the knowledge of health professionals about the existence of the resolution and, in two of them, most claimed to know. According to the study by Fusculim, et al [20] (2022), about 58% of the participants, composed of doctors and nurses, knew the resolution; Murasse, and Ribeiro [18] (2022) demonstrated that 57.8% of participating physicians knew. However, it is worth noting that a significant number of professionals were not aware of it and, as it is a standard applicable to health professionals, it is imperative that it be generally known.
Contrary to the cited studies, Gomes, et al [17] (2018) demonstrated that only 10% of physicians had prior knowledge about AD and understood that there is no legislation regarding the entire Brazilian population so far. In agreement with this result, Guirro, et al [15] (2022) reported that 38.1% of health professionals knew some document related to the manifestation of the patients’ will, and only 19.6% knew the BFCM Resolution 1995/2012. The lack of further clarification on the legal aspects of AD, which should be explored since college, can generate insecurity or a feeling of discomfort in the care team, from a moral point of view, affecting adherence to the instrument, even though they continue to respect the patient’s autonomy. As proof of this, Gomes and Goldim [19] (2022) demonstrated that 78.1% of doctors who work in a hospital emergency in Curitiba/PR believe that legal aspects influence the use of AD, second only to ethical aspects (93.8%), moral (87.5%) and technical (81.2%).
Furthermore, an important data presented by Murasse and Ribeiro [18] (2022), was that although most of the participants claimed to know the CFM Resolution 1995/2012, 64.5% expressed that they did not feel legally comfortable to use the instrument in the decision-making process. of decision. Although the professional team is legally covered, as previously mentioned, Gomes and Goldim [19] (2022) found in a survey that 84.4% of doctors think it is necessary to create a specific law for situations of AD, so that 87.5 % of physicians stated that they would comply with AD if there were specific legislation and the remaining 12.5% responded that they might consider them in their decisions.
Regarding the use of AD by health professionals, among the five selected articles, Gomes and Goldim [19] (2022); Murasse and Ribeiro [18] (2022) and Fusculim, et al [20] (2022) demonstrated that most participants used the tool. The other two articles demonstrated that a minority would use AD. Gomes and Goldim [19] (2022) addressed the justifications presented by physicians for the use of AD, encompassing both the perspectives of patients and professionals themselves. From the patient’s point of view, they highlighted the need to be properly informed and respected for their autonomy. From the physician’s perspective, directives facilitate decision-making since they emphasize the desires and expectations of the patient and also support the non-use of therapeutic measures characterized as futile, that is, that do not benefit the patient.
Still on the implementation of AD in the practice of health professionals, three articles explained elements that cause hesitation in the use of directives. According to Fusculim, et al [20] (2022), the fear of doctors and nurses in implementing the tool would be negatively associated with some factors, that is: the greater the fear, the lower the incidence of other variables. The conditions related in this way were: knowledge in palliative care, beginning of contact with palliative care at home, main activity in palliative care/intensive care and knowledge of BFCM Resolution 1995/2012. As previously mentioned, Gomes and Goldim [19] (2022) address eleven different aspects that may influence the use of AD in the hospital emergency environment, with five of them cited by most participants ethical aspects (93.8%), moral (87.5%), technical (81.2%), legal (78.1%) and religious (56.2%). Gomes, et al [18] (2018) reports that 88% of the physicians interviewed believed that religion can interfere with the use of directives. It is important to emphasize that in the studies that presented positive results for the use of the instrument, they identified a higher percentage in the question of clarification of professionals on the subject. Therefore, it is possible to perceive an intimate relationship between the level of knowledge about AD among health professionals and the feeling of security in using it for registering patients or preparing their own AD.
According to Gomes and Goldim [19] (2022), 81.3% of physicians claimed to know about AD and 87.5% were in favor of its use. The two doctors who answered that the patient could only influence, but not define, the decision to be taken had little and medium knowledge about the directives. The only physician who replied that he would not take into account the patient’s anticipated wishes in his decision-making process was unaware of AD. Following the same line of reasoning, Murasse and Ribeiro [18] (2022) reported that physicians who correctly answered the questionnaires about their perceptions in relation to AD, had less discomfort in their application for decision-making in cases of patients with incurable disease in an advanced state. In addition, in the study by Fusculim, et al [20] (2022), whose result of doctors and nurses who knew AD was 82% and about 74.4% had knowledge about palliative care, demonstrated that on average 94% of participants stated that they believe that people need to have their AD and about 64% would be interested in writing their own AD.
However, in the study proposed by Gomes, et al [17] (2018), in which 90% of physicians did not know what AD was and did not know a standard that regulated AD, even after being introduced to the official concept of Resolution BFCM 1995 /2012 and presented with the current situation and importance of the topic in Brazil, only 43% of physicians were willing to use the instrument. This result goes against the research carried out by Guirro, et al [15] (2022), which identified that 60% of the health professionals who worked in a teaching hospital located in the city of Curitiba/PR did not know the AD, however, after explanation on the subject, 71% of the participants perceived the AD as an important document, believing that people should express their desire about end-of-life treatments and responding that they would think about preparing their own AD.
It is also worth mentioning that although AD is a topic that is still not very acceptable to the medical profession, the two articles that portray who should be given the responsibility of initiating a conversation about the instrument believe that it should be the doctor. This data reinforces the risk of lack of knowledge about the subject, because if the professional does not know, it will probably not be discussed in the reality of care. Nevertheless, it is valid that the responsibility must be divided between doctors and nurses, since these professionals have a closer relationship with the patient because they work on the front line of care and are in constant contact with patients. It is also clear to highlight the existence of a study limitation, as only one study cited the nurse’s option to initiate conversation [15-20].
Finally, it is worth noting the concentration of the five studies conducted in the South region, with one article, and the Southeast region of Brazil, with the remaining four. The study conducted by Fusculim et al. [20] (2022), using social networks, made it possible to reach a larger number of participants throughout the country. In the same study, it was observed that professionals from the Southeast region have a positive relationship with knowledge about AD and its process of development and documentation; knowledge of other people who have the tool; and knowledge of CFM Resolution 1995/2012. Additionally, professionals from the Southeast were the ones who attributed the responsibility of initiating the conversation about ACP to the doctor, while in the South region, this responsibility was attributed to family members/ caregivers.
Furthermore, according to the author [20], the Southeast region encompasses the largest number of postgraduate courses in palliative care, extending to the multidisciplinary team, which suggests that these professionals have more knowledge about palliative care and AD, as well as better conditions to discuss AD with patients. However, it should be emphasized that the study proposed by Fusculim et al (2022) [20], when comparing regions of the country, has a limited analysis, as professionals from the South and Southeast regions accounted for 84.4% of the research participants, leaving the remaining 15.6% for the Midwest (7.1%), Northeast (7.8%), and North (0.1%).
Conclusion
With the data obtained in this research, it can be concluded that knowledge about AD and its ethical and legal bases is still precarious among health professionals, reflecting the lack of instrumentation of patients. This is because the greater the knowledge and experience in the practice of health and palliative care, the greater the safety in the applicability of the instrument. This makes clear the need for teaching about AD and their bioethical aspects throughout graduation, since, as noted, professionals are interested in learning these directives. In addition, it is the responsibility of the councils referring to the professions of medicine and nursing to increase the dissemination of the document and greater guarantee of safety for health professionals in its use. However, it must be considered that there are still a scarce number of studies on the subject, with a predominance of the medical public and the South and Southeast regions of Brazil, making it evident the need for further investigation in the nursing public and nursing technicians, as well as approaching other regions of the country.
Acknowledgment
None.
Conflict of interest
None.
References
- Arruda LM de, Abreu KPB, Santana LBC, Sales MV de C (2019). Variables that influence the medical decision regarding Advance Directives and their impact on end-of-life care. einstein [Internet] 18: eRW4852.
- Chang HY, Takemura N, Chau PH, Lin CC (2022). Prevalence and predictors of advance directive among terminally ill patients in Taiwan before enactment of Patient Right to Autonomy Act: a nationwide population-based study. BMC Palliat Care 21(1): 178.
- Cogo SB, Lunardi VL, Quintana AM, Girardon-Perlini NMO, Silveira RS, et al. (2016) Challenges to implementation of advance directives of will in hospital practice. Rev Bras Enferm [Internet] 69(6): 1031-1038.
- Cogo SB, Lunardi VL, Quintana AM, Girardon-Perlini NMO, Silveira RS da, et al. (2017) Assistência ao doente terminal: vantagens na aplicabilidade das diretivas antecipadas de vontade no contexto hospitalar. Rev Gaúcha Enferm [Internet] 38(4):
- Dadalto L, Tupinambás U, Greco DB (2013) Diretivas antecipadas de vontade: um modelo brasileiro. Revista Bioética 21(3): 463-476.
- Santana SCG, Câmara D de B (2022) Percepção e Expectativas de Pacientes com Câncer acerca das Diretivas Antecipadas de Vontade. Rev. Bras. Cancerol. [Internet]. [citado 29º de maio de 2023] 68(1): e-181625.
- Alves TAB (2017) Limitação do esforço terapêutico no doente internado: definição do processo de decisão e sua oportunidade Investigação casuística do problema. [master’s thesis]. Covilhã: Faculdade de Ciências da Saúde, Universidade da Beira Interior p: 20.
- Mendes MVG, Silva JC de O, Ericeira MAL, Pinheiro AN (2019) Testamento Vital: Conhecimentos e Atitudes de Alunos Internos de um Curso de Medicina. Rev bras educ med [Internet] 43(2): 25-31.
- (2012) Conselho Federal de Medicina. Resolução no 1.995, de 9 de agosto de 2012. Dispõe sobre as diretivas antecipadas de vontade dos pacientes. Diário Oficial da União [Internet]. Brasília, nº 170: 269-270.
- Nogario ACD, Barlem ELD, Tomaschewski-Barlem JG, Silveira RS da, Cogo SB, et al. (2020) Advance directives of patients: process of implementation by palliative care teams. Rev Bras Enferm [Internet] 73(suppl 6): e20190567.
- Silveira MJ (2022) Advance care platina and advance directives.
- Pittelli SD, Oliveira RA, Nazareth JC (2020) Diretivas antecipadas de vontade: proposta de instrumento único. bioét 28(4): 604-609.
- Nunes MI, Anjos MF dos (2014) Diretivas antecipadas de vontade: benefícios, obstáculos e limites. Rev Bioét [Internet] 22(2): 241-251.
- Hassegawa LCU, Rubira MC, Vieira SM, Rubira APA, Katsuragawa TH, et. al. (2019) Approaches and reflexions on advance healthcare directives in Brazil. Rev Bras Enferm [Internet] 72(1): 256-264.
- Guirro ÚB do P, Ferreira F de S, Vinne L van der, Miranda GF de F (2022) Conhecimento sobre diretivas antecipadas de vontade em hospital-escola. Rev Bioét [Internet] 30(1): 116-125.
- Simões NG, Flávia Augusta, Jurema Telles, Mirella Rebello, Ana Karla Almeida, et al. (2019) Conhecimentos e práticas de médicos do IMIP sobre Diretivas Antecipadas de Vontade: “corte transversal”. Atena Editora: 138-147.
- Gomes BMM, Salomão LA, Simões AC, Rebouças BO, Dadalto L, et al. (2018) Diretivas antecipadas de vontade em geriatria. Rev Bioét [Internet] 26(3): 429-439.
- Murasse LS, Ribeiro URVCO (2022) Diretivas antecipadas de vontade: conhecimento e utilização por médicos residentes. bioét 30(3): 598-609.
- Gomes PA, Goldim JR (2022) Diretivas antecipadas de vontade em unidade de emergência hospitalar. Rev Bioét [Internet] 30(1): 106-115.
- Fusculim ARB, Guirro ÚB do P, Souza W, Corradi-Perini C (2022) Diretivas antecipadas de vontade: amparo bioético às questões éticas em saúde. Rev Bioét [Internet] 30(3): 589-597.
- (2016) Brasil. [Constituição (1988)]. Constituição da República Federativa do Brasil [Internet]. Brasília, DF: Senado Federal; [cited 2023 Mar 19] p: 496.
- (2002) Lei nº 10.406, de 10 de janeiro de 2002. Institui o Código Civil. Diário Oficial da União [Internet]. Jan 11.
- (2003) Brasil. Lei nº 10.741, de 1º de outubro de 2003. Dispõe sobre o Estatuto do Idoso e dá outras providências. Diário Oficial da União [Internet].
- (2017) Conselho Federal de Medicina. Resolução CFM no 2.168, de 21 de setembro de 2017. Adota as normas éticas para a utilização das técnicas de reprodução assistida – sempre em defesa do aperfeiçoamento das práticas e da observância aos princípios éticos e bioéticos que ajudam a trazer maior segurança e eficácia a tratamentos e procedimentos médicos –, tornando-se o dispositivo deontológico a ser seguido pelos médicos brasileiros e revogando a Resolução CFM no 2.121. Diário Oficial da União [Internet]. Brasília.
- (2017) Conselho Federal de Medicina. Resolução CFM no 2.173, de 23 de novembro de 2017. Define os critérios do diagnóstico de morte encefálica. Diário Oficial da União [Internet]. Brasília.
-
Vanessa Cristina Carvalho Castro, Juliana Reis Moura Lippo Acioli and Isaura Romero Peixoto*. Assessment of Knowledge of Brazilian Health Professionals About Advance Directives: A Systematic Review. Glob J Aging Geriatr Res. 2(4): 2023. GJAGR.MS.ID.000541.
-
Advance Directives, Living Wills, Health Professionals, Knowledge, Comfortable
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






