 Research Article
Research Article
A Community-Based Participatory Approach for Needs Assessment and Intervention: A Mixed Methods Study Program of Older University Employees During COVID-19
Zhao Chen1*, Yunjia Yang2, Kendra Jason3, Mark Wager1, Kathleen C Insel4, Hamza Butt1a, Dagoberto Robles1, Amanda Sokan5, Heather Kenning1, Marc Verhougstraete6, Lisa O’Neill7, Mindy Fain7, Linda Philips7, Kiranmayee Muralidhar8 and Nicole Yuan9
1Department of Epidemiology and Biostatistics, Mel and Enid Zuckerman College of Public Health, the University of Arizona, 1295 N Martin Ave, Tucson, AZ 85724, USA
2Public Health Administration, Mel and Enid Zuckerman College of Public Health, the University of Arizona, USA
3Department of Sociology, UNC Charlotte, USA
4Nursing and Health Sciences Division, University of Arizona, USA
5Department of Public Health Practice & Translational Research, Mel and Enid Zuckerman College of Public Health -Phoenix Campus, University of Arizona, USA
6Department of Community, Environment, and Policy, Mel and Enid Zuckerman College of Public Health, the University of Arizona, USA
7Center on Aging, University of Arizona, USA
8Public Health Research Institute of India, India
9Department of Health Promotion Sciences, Mel and Enid Zuckerman College of Public Health, the University of Arizona, 1295 N Martin Ave, Box 245209, Tucson,AZ 85724, USA
aHamza Butt passed away
Zhao Chen, Department of Epidemiology and Biostatistics, Associate Dean for Research Mel and Enid Zuckerman College of Public Health, University of Arizona, USA
Received Date:December 16, 2024; Published Date: February 04, 2025
Abstract
Background: The COVID-19 pandemic has negatively impacted the work and life of older adults. Studies on university campus have been
primarily focusing on students, but rarely on older employees who are a significant part of the campus community. This study program was designed
to survey older university employees’ concerns and needs during the pandemic and to develop strategies to mitigate the adverse health impacts of
COVID-19 in a pressing timeframe.
Methods: Mixed methods and community-based participatory approach were used in this three-phase study program. Older employees (age
≥50) from the University of Arizona were recruited. Focus groups and online campuswide survey were done in the fall of 2020 followed by three pilot
online interventions for health promotion. Descriptive data analysis was done by gender of the survey participants in this paper.
Results: There were 1030 individuals from different classified jobs, genders, and racial/ethnic groups who participated in the online survey.
The group’s diversity was high, but men and racial or ethnic minority groups were still underrepresented. The overall health was good for the
majority of the participants, but a small percent had not only poor overall health but also specific disease conditions which may increase their risk
for poor outcomes with COVID-19. Participants expressed concerns about work safety related to their caregiving responsibilities. We observed high
interest in participating in online health promotion interventions during the pandemic.
Conclusion: COVID-19 adversely affected older university employees existed in many domains. The methodological considerations in the three
phases of the study activities on campus for health promotion and disease prevention among older employees may inform future research and health
promotion programs.
Keywords:Older Employees; University; COVID-19; Health
CBPA: Community-Based Participatory Approach; SAGUARO: A SAFER and STRONGER UA FOR OLDER EMPLOYEES; CAB: Community Advisory Board; FFMQ: Five Facet Mindfulness Questionnaire; PSQI: Pittsburg Sleep Quality Index; AI/AN: American Indian/Alaska Native
Introduction
A community-based participatory approach (CBPA) to health research is a valuable and underutilized methodology that requires academic and community partners to collaborate in research design and intervention conceptualization to address health disparities [1]. It is very effective in developing interest and participation of underrepresented populations in health research such as African American [2] hearing-impaired [3] and Latino communities [4]. CBPA is used to center cultural relevance, promote engagement and acceptability in health research, and increase awareness of health issues embedded in communities [5]. CBPA is often carried out using qualitative methods such as participatory methods, interviews, evaluation research, and case studies [6]. By necessity, the approach is based on relationships and networks with community stakeholders [7].
In this article, we systematically examine our research design and fieldwork experiences to bring forth deeper knowledge and understanding of the benefits of a community participatory approach and a mixed methods design with another underrepresented community in health research: older workers in higher education. Here we focus on methodological issues and present findings only as they are relevant to the research practice [8] and inform future data collection and increase scientific stature. We also seek to bring more attention to older workers as high-risk adults navigating COVID-19 and, in the future, other health-related exposures. in a context-specific workplace: the university.
The examination of our study begins with contextualizing our research within the broader literature on older adults, COVID-19, and health disparities. We then detail our communitybased participatory approach which includes virtual community engagement, a community advisory board, focus groups, online surveys, and three separate interventions: 1) a virtual Tai Chi/ Qigong program, 2) a step-up (walking) program, and 3) a daily meditation program. We detail the analytic process used to determine the CBPA and connect each approach to key study features. Finally, we discuss the challenges and advantages of our approach through our lessons learned which are designed to inform future research.
Research Context Older University Workers
Institutions of higher learning have higher numbers of older employees who represent a valuable and more experienced part of the workforce [9, 10] with diverse job responsibilities, racial and ethnic backgrounds, and socioeconomic status. A recent report by the College and University Professional Association for Human Resources identified that while the median age of the U.S. workforce is 42 years, universities and colleges present a median faculty employee age of 45 years [11]. Around 23% percent of workers in the U.S. fall into an age category of 55 years or more, and although colleges and universities do show similar proportions of employees in this age range, those classified specifically as faculty aged 55 or older make up 37% of older workers [11, 12].
Understanding the risk perceptions and concerns of the older university employees with university reopening during the pandemic is important as many of the older faculty and staff need to interact closely with a large number of students. However, burgeoning research on the effects of COVID-19 and university experiences in the U.S. tend to focus on the transmission of SARS- CoV-2, the virus that causes COVID-19, or student-related consequences of COVID-19 such as clusters [13], mental health [14], and sleep [15], but none to our knowledge on the effects on university workers, especially those that go beyond the consideration of faculty. This research will provide information for us to better prepare for future outbreaks or pandemics.
COVID-19 Impacts on Older Workers
Middle age and older adults are at increased risk for severe illness with COVID-19 due to age-related weakening immune function and the increased presence of comorbidities such as hypertension, cardiovascular disease, diabetes, chronic respiratory disease, and chronic kidney disease [16,17]. Previous studies highlight the challenges facing older adults during the outbreak of the COVID-19 pandemic. One of these challenges is continued workforce engagement during the pandemic. According to the U.S. Bureau of Labor Statistics [12], approximately one in five adults aged 65 or older participated in the labor force prior to the pandemic, with nearly 75% of these individuals working at jobs where teleworking was not an option [18]. Older workers have been hit harder by the effects of COVID-19 than any other demographic [18], and the effects of coronavirus have disproportionately affected Black and Hispanic workers, women caregivers, and lowwage workers [19,20].
Previous research has linked health, work environments, and workforce engagement, but none to our knowledge has addressed these relationships within the context of the COVID-19 pandemic. Research has demonstrated that more vulnerable populations experience increased health risks and financial risks such as older workers engaged in low-wage work are substantially higher than for high-wage workers [21]. Less is known about how the vulnerability of older workers is influenced by the type of job worked. In this study, we examine the work experiences of older adults at a large land-grant university in the southwestern region of the United States to explore how the effects of COVID-19 shaped their workforce engagement and their perceptions of how the university responded to their unique needs.
University of Arizona: The SAGUARO Study
Arizona had the country’s leading incidence of cases of COVID-19 and death rate in June 2020 and January 2021 [22,23]. The University of Arizona (UA) provided a unique opportunity to study the concerns and needs for interventions to promote the health and well-being of older employees during a pandemic. In the “A SAFER and STRONGER UA FOR OLDER EMPLOYEES” (SAGUARO) study program, we examined the work experiences of older adults (≥50) at the University of Arizona, a large state university consisting of 64,274 faculty, students, and staff [24]. The study objectives were 1) to understand the needs and concerns about re-opening campus during the pandemic; 2) to use the findings to inform the development of mitigation strategies that promote health and wellbeing; 3) to implement and evaluate mitigation strategies for this older population. The study aimed to recruit employees with diverse employment categories (e.g., staff, student workers, graduate assistants, continuing professionals, and faculty) to better capture the experiences based on occupation status, as well as factors such as age, race, gender, and household composition. In this paper, we presented the study design, procedures, and methodological considerations of the SAGUARO study program and results from the first online campus-wide survey to demonstrate the concerns and needs of older employees at the University.
Key Study Features
The Saguaro study program was designed to capture a historical public health event: the worldwide spread of a new disease’s impact on a local university community and it included three phases. The COVID-19 pandemic presented a unique opportunity to capture genesis data on individual lives and community ties at the University of Arizona. Our study was designed to maximize data collection through unique methodological approaches to address the ever-evolving challenges and changes associated with the pandemic in a work setting under pressing time and with limited resources. This manuscript focuses on the overview of the study design, recruitment process, data collection methods, analytic approach, and results of the characteristics of the participants in phase I, and the impact of COVID-19 on the entire research process. The findings and potential values of this research as well as lessons learned from this research undertaken can be used to inform future studies and health promotion programs.
Methods
Overall Study Design:
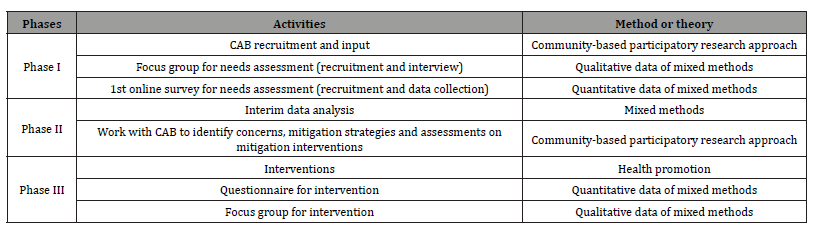
The Saguaro study program started in July 2020 with funding support from the university and included three phases. We applied community-based participatory research principles, with an emphasis on the engagement of key stakeholders at the university in the design and conduct of the study, to ensure that the investigation was not only relevant but also beneficial to the targeted age group. Mixed methods research designs were used to achieve a greater depth of understanding of the needs of older employees and the impacts of health promotion interventions. The study protocol was approved by the Institutional Review Board. The study design and activities for each phase of the study are summarized in Table 1 and described below.
Table 1: Study Overview.
Phase 1- A sequential exploratory mixed methods study design was used in the first phase of the study. The purpose of Phase 1 was to engage UA leaders, stakeholders, and older employees in a needs assessment during the early stages of the COVID-19 pandemic and the closing of the university campus. A community advisory board (CAB) was formed to partner with the research team throughout this study. The needs assessment was first conducted using focus group interviews. The interview results were then used to inform the design of an online survey with older employees. The online survey aimed to further assess the specific needs and concerns of older employees that were brought up from the focus group interviews regarding the creation of a healthier, safer, and supportive workplace during and post COVID-19.
Phase 2 - Development of mitigation strategies/interventions and identification of indicators for the effectiveness of the mitigation strategies. Phase 2 involved developing health promotion strategies tailored for UA employees ≥50 based on known risks from COVID-19 research and perceived risks and needs identified in Phase 1. This phase involved a review of the focus group interview transcripts and responses to the survey items about interest in intervention strategies in the survey. In addition, the study team consulted with the CAB and sought their input on specific intervention strategies, including peer support groups, meditation, Tai Chi practice and other forms of stress reduction, and mental health promotion and resilience-building programs for older populations.
Phase 3 - Implementation of mitigation strategies and preliminary evaluation. Phase 3 involved implementing the interventions that were considered feasible based on the short study timeframe of 3 months and limited budget and resources. Three separate interventions were developed: 1) a virtual Tai Chi/ Qigong program, 2) a step-up (walking) program, and 3) a daily meditation program. Mixed methods were used to increase the understanding of the intervention impacts.
Recruitment and Participants
Phase 1- Community Advisory Board (CAB): One of the most critical first steps of the study consisted of establishing a CAB with older employees. The purpose of the CAB was to provide input on all three phases of the study. This included a review of study protocols and documents, assistance with participant recruitment, feedback on the interventions, interpretation of findings, and contributions to dissemination activities. CAB members were recruited by sending email invitations to administrators, key operation units, and employee organizations and councils and requesting either their participation in the CAB or to provide recommendations for alternative employee representatives.
The CAB was managed by the principal investigator and two coinvestigators with expertise in community engagement including one who co-authored guidelines for increasing the effectiveness of CABs in health research [25]. A total of 12 older employees (50 and older) agreed to serve on the board. CAB members attended an introduction session where the investigative team presented the aims of the study, CAB responsibilities, hours required, and the anticipated project timeline. After the initial meeting, CAB members signed a commitment letter indicating they were willing to serve the study for 4 months. The CAB met every two weeks during the first three months of the study and then monthly for two months. During the meetings and email exchanges, CAB members provided continuous input to all three phases of the study.
Focus groups: Recruitment for focus group interviews with older employees began by asking the CAB members to provide names and contact information for 4-6 people they believed would be comfortable sharing their thoughts and opinions on campus re-opening in a virtual focus group setting. CAB members were provided the option of contacting individuals to pre-confirm interest or sending names of those they had not contacted to the study team. CAB members were also asked for suggestions regarding recruitment flyer advertising. University employees were eligible to participate in the focus group interviews if they were 50 and older. Efforts were made to recruit employees with diverse racial/ethnic backgrounds and university job classifications (i.e., faculty, academic professionals, administration, classified staff, service professionals, and post-docs/grad assistants/student workers). The study team also invited university employees they knew of and who met the inclusion criteria and posted the study information to university listservs.
Online Survey: Recruitment for the online survey was conducted primarily via college listservs and UA announcement boards, with links posted on the UA Research, Innovation, and Impact (RII) website. The survey information was sent to each College Dean with a request that they forward the survey to the faculty and staff in his/her respective colleges. In addition, CAB members sent the survey to people within the University Facilities Management and other appointed personnel throughout the University. To reach employees who do not routinely utilize computers for their work, flyers were posted in the student union and distributed elsewhere via Facilities Management. All respondents were given a unique ID number and any personal information collected from the consent form or gift card raffle drawing (as an incentive) was completely separated from survey responses. Each participant who was interested in the raffle drawing was randomly assigned a number. CAB members and research team members, who were blinded by participants’ names, did the drawings using random numbers.
Phase 2 - There was no new recruitment in Phase 2 as this phase was used to analyze data collected from Phase 1 and develop interventions for Phase 3.
Phase 3 - Participants in this phase were also older UArizona employees (≥50). Those who completed the online survey were invited to join one of the interventions (Tai Chi/Qigong, Step-Up, and Meditation). Emails were also sent to college deans and staff organizations to expand the recruitment. Participants of each intervention were sent email invitations to participate in separate focus group interviews for the Tai Chi/Qigong, Step-Up, and Meditation interventions after they completed the intervention. Raffle drawings for gift cards were offered to individuals who participated in the intervention programs and focus group interviews.
Data Collection
Phase 1 - The focus group interviews took between 1 - 1.5 hours. The focus group facilitator asked questions about concerns and perceived risks related to the university community returning to campus, individual strategies, and barriers to reducing risks, and university interventions and policies to promote the safety and health of older employees. The focus group interviews were transcribed using a Zoom function. The Zoom transcriptions were compared to the video recordings by a member of the study team and were corrected to achieve maximum accuracy. A preliminary review of the transcripts was used to highlight some key areas for consideration for the online campus survey for older employees.
The online survey assessed the specific needs and concerns of older employees regarding the creation of a healthier, safer, and supportive workplace during and post COVID-19. The survey was developed by the study team using adapted questions from NIH resources and published studies and questions developed specifically for this study.
The survey had seven sections: 1) demographic and characteristics; 2) employment and work experience; 3) work environment; 4) risks, perceptions, and exposure with COVID-19; 5) psychological health in relation to COVID-19; 6) life change as a result of the COVID-19 pandemic; and 7) perception of the UArizona leadership in relation to response and management of risks of COVID-19. A list of potential interventions was presented at the end of the survey to determine respondents’ interest in participating in them. The survey was administrated using REDCap and took about 20 minutes to complete. Formal consenting was done within REDCap for electronic signatures from the participants.
Phase 2 - There was no new data collection in Phase 2.
Phase 3 - Questionnaires and focus group interviews were used to collect data on the impact and outcomes of the three separate interventions 1) a virtual Tai Chi/Qigong intervention, 2) a step-up (walking) intervention, and 3) a daily meditation intervention.
The questionnaires included a basic demographics questionnaire, the Five Facet Mindfulness Questionnaire (FFMQ) [26], Pittsburg Sleep Quality Index (PSQI) [27], and a series of questions on psychological health to measure outcomes of interest (psychological health, sleep quality, mindfulness). In addition, the follow-up questionnaire included satisfaction questions about the intervention and a question asking individuals whether they would be interested in participating in a focus group interview about their experiences with the intervention.
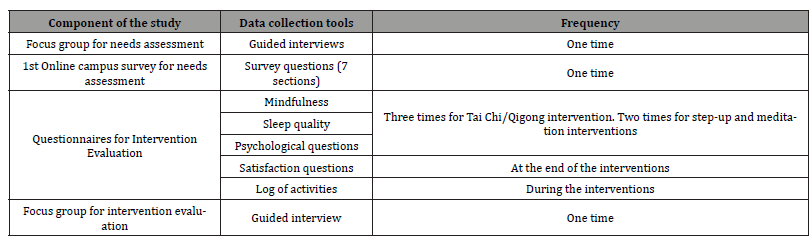
The focus group interview questions assessed the impacts of the intervention, participants’ satisfaction, and suggestions for improvements. The focus group interviews took between 1 - 1.5 hours. The focus group interviews were transcribed using a Zoom function. The Zoom transcriptions were compared to the video recordings by a member of the study team and were corrected to achieve maximum accuracy. Data collection was completed in May 2021. Table 2 presents the data collection details.
Table 2: Data Collection.
Data Analysis
This manuscript intends to highlight methodological considerations and a protocol summary. A descriptive analysis was conducted on quantitative data from the online survey in Phase 1 to help show the characteristics of the study population and facilitate the discussion on the strengths and limitations of this study program.
Results
Phase 1 - Thirty-three individuals agreed to participate in the Phase 1 focus group interview. Individuals completed an online consent form and a short demographic survey before the focus group interview. Out of the 33 potential participants, 24 individuals participated in one of the six focus group interviews that were conducted virtually using Zoom video conferencing in August 2020. The other nine participants had time conflicts with the focus group meeting times. The focus group participants were largely female (70%, n=17) and from different job classifications, including faculty (8%, n=2), academic professional (17%, n=4), administration (13%, n=3), and staff (63%, n=15). A total of 1030 employees completed the online survey. The demographic and caregiver characteristics of the participants are presented in Table 3.
Table 3: Demographic and caregiver characteristics (overall and stratified by gender).
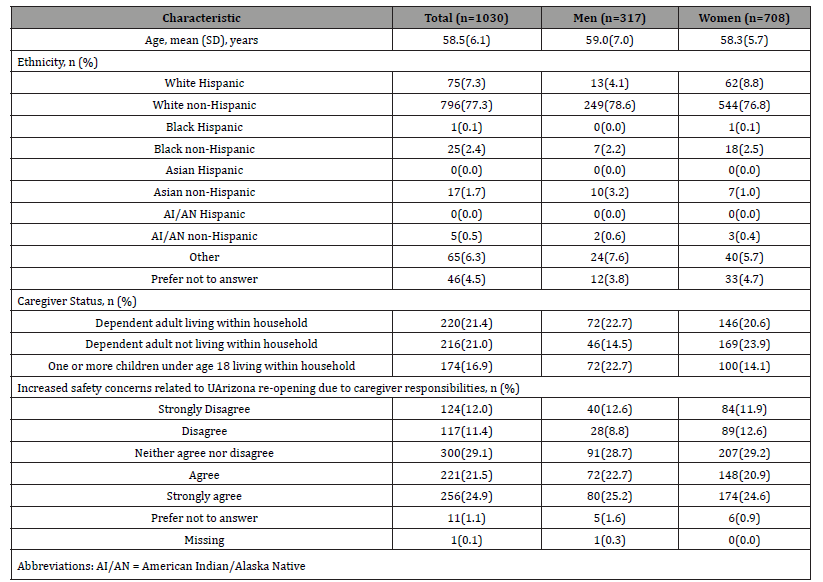
a. The gender group ‘other’ contained 5 observations and is included in the totals but not as a separate category.
The majority of the participants were women. The average age of the survey participants was 58.5 (SD = 6.1), with men slightly older than women. Overall, 796 (77.3%) of the participants were White non-Hispanics. There were 75 White Hispanics, 1 Black Hispanic, 25 Black non-Hispanics, 17 Asian non-Hispanics, 5 AI/ AN non-Hispanics, 65 who chose “others”, and 46 who preferred not to answer. For caregiver status, 21.4%, 21.0%, and 16.9% of participants reported having dependent adults living within the household, dependent adults not living within the household, or one or more children under age 18 living within the household correspondingly. There were 21.5% of them agreed and 24.9% of them strongly agreed that they had increased safety concerns related to UA reopening due to caregiver responsibilities, however, there were 11.4% of them disagreed and 12.0% of them strongly disagreed with this statement.
Table 4 presents the employment and workplace characteristics of the online survey participants. The majority (62.5%) of the participants were staff members of the university, 21.6% were faculty, 3.5% were continuing academic professionals and 10.2% were administrative personnel. The majority (88.6%) of the participants were from the Tucson Campus where the research team is based. Despite the university closing (between March - August of 2020), 37.7% of the participants still worked on campus, with about 22 hours per week to support the basic functions of the university. At the survey time (August 2020), over 62% of the participants expected to work primarily at home in the fall semester.
Table 4:Employment and workplace characteristics (overall and stratified by gender).
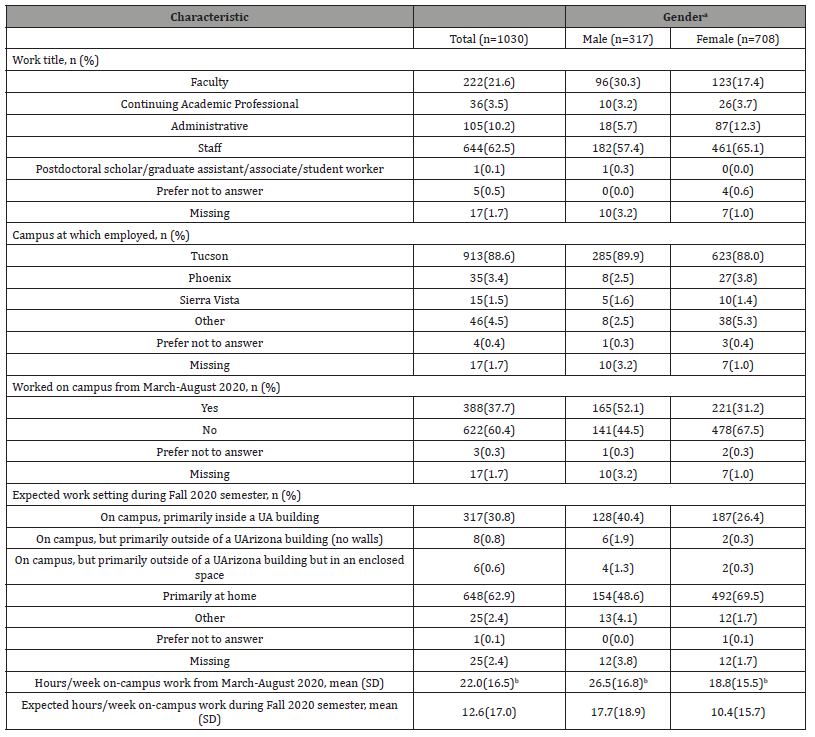
a. The gender group ‘other’ contained 5 observations and is included in the totals but not as a separate category.
b. Refers only to respondents who reported working ‘on-campus’ from March-August 2020
Table 5 provides insights into individuals’ health and psychological well-being, with a focus on gender-based differences. Most participants reported no comorbid conditions (50.2% overall). Distribution by gender was similar, with men at 48.9% and women at 50.7% reporting no conditions. The majority rated their health as “very good” (39.7% overall), followed by “good” (33.2%). Men slightly outnumbered women in the “excellent” and “very good” categories. About 41.4% reported having 2-3 individuals to talk to about important matters since the pandemic started.
Table 5:Health status and psychological impact of COVID-19 pandemic (overall and stratified by gender).
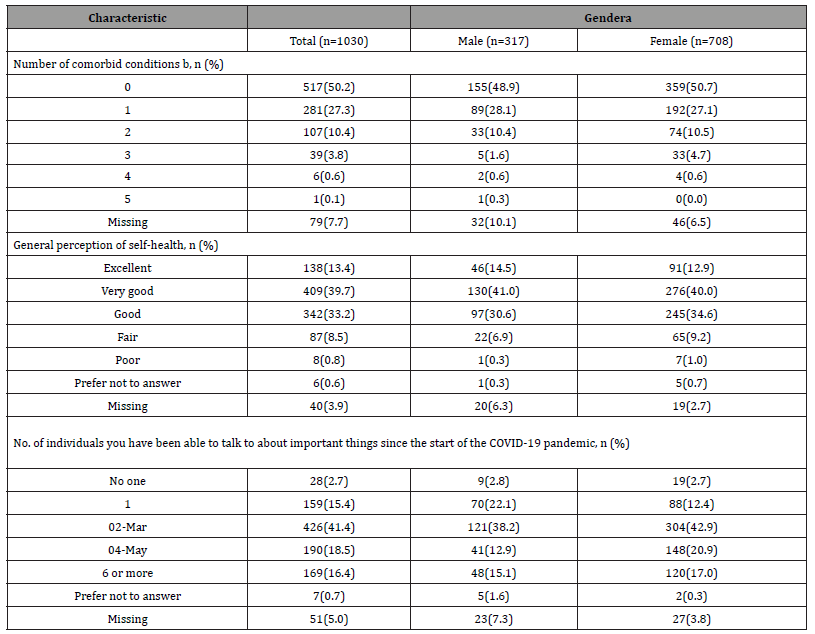
a. The gender group ‘other’ contained 5 observations and is included in the totals but not as a separate category.
b. Comorbid conditions included: Chronic Kidney Disease (CKD), Chronic Obstructive Pulmonary Disease (COPD), Obesity (BMI of 30 or higher),
Immunocompromised State from Solid Organ Transplant, Serious heart conditions (such as heart failure, coronary artery disease, cardiomyopathies),
Type 2 Diabetes.
Phase 2 - The mixed methods analysis results on needs assignment and intervention program development in Phase 2 will be reported in a later paper.
Phase 3 - a). Online Tai Chi/Qigong intervention: We recruited 102 participants who were UA employees aged ≥50 years for the Tai Chi and Qigong intervention program. Participants were randomly assigned to one of two groups. The first group immediately began the 6-week Tai Chi and Qigong intervention. The second group served as waitlist controls. The groups were then switched at the end of week 6, making the intervention period a total of 12 weeks in length. Demographic information was collected at baseline while other questionnaires were administered at three time points: baseline, six weeks, and twelve weeks for all participants. Information regarding the participant’s satisfaction with the intervention was also collected at the end of intervention. Tai Chi and Qigong classes were taught live three times a week for a total of six weeks using Zoom video conferencing. The sessions consisted of warm-up with meditation, Qigong (Ba Duan Jin), Tai Chi (Bafa Wubu), and cool down, which totaled 50 minutes. Participants were asked to complete and submit weekly logs online that described the frequency and length of their practice. All sessions were recorded, and recordings were available to participants. Individuals were given the option to participate in the heart rate variability portion of this study using a wearable sensor Polar® H9 [28] at different time points of a week and submit the data weekly. The mixed methods result of the intervention will be reported later.
b). Step-up intervention: One-hundred and thirty-two participants were recruited into a 4-week walking intervention to increase physical activity. During a 1-hour online introductory session via Zoom, the research team introduced the intervention and purpose of the study, provided the informed consent form, discussed the benefits of walking and physical exercise specific to older adults, and answered any questions or concerns. Resources provided to participants included instructions on how to obtain a step count via smartphone or pedometer (provided by the research team if the participant did not have access to a step counting device), population/usage density maps of the UA campus, and an average number of steps to expect per distance walked. The introductory session was recorded to be viewed by participants later if needed. Participants were asked to complete questionnaires via REDCap before and after the intervention. Participants were also asked to record their daily step amounts and submit a weekly report online using RedCap. Researchers emailed participants weekly reminders to submit this weekly report and provided motivation and encouragement to engage in regular and consistent exercise. The mixed methods analysis of the intervention will be reported later.
c). Daily meditation intervention: Fifty-four participants enrolled in a 4-week meditation intervention study. The same set of questionnaires was used to assess outcomes with both preintervention and post-intervention assessments. A 1-hour Mindful Workshop was held via Zoom to introduce the participants to the principles of meditation by a UA Campus Health Counseling and Psych Services Therapist. Participants practiced with the instructor and were provided tools for daily meditation practice (e.g. phone apps and YouTube videos). Participants were asked to meditate at least 10 minutes per day, record the amount of time spent meditating, and submit a weekly report via REDCap. Researchers sent weekly reminders to submit the report, and to provide motivation and encouragement to participants about their meditation practice. The mixed methods analysis of the daily meditation intervention will be reported in a later paper.
Discussion
Older workers have been hit harder by the effects of COVID-19 than any other demographic [18], and the effects of coronavirus have disproportionately affected Black and Hispanic workers, female caregivers, and low-wage workers [19, 20]. Previous research linked work experiences and health, but to our knowledge none has addressed these relationships within the context of older workers during the COVID-19 pandemic. While much attention has been given to university remote learning, closures, and guidelines for preparedness of COVID-19, much less is known about the needs, concerns, and coping strategies of the very employees who create and maintain the learning and research environment for students. Our study filled in the gap of knowledge during the critical time of an unprecedented pandemic and showed great interest of participating in studies by older university employers. The strong needs for health promotion were reflected by their active participation in the interventions, and their appreciation for having these health promotion opportunities during the discussions of the focus group interview.
Universities employ a higher percentage of older adults [29] with diverse job responsibilities and socioeconomic status. Similar to the nationwide percentage of older employees in universities, the University of Arizona had 23.8% (or 5768) of employees aged 50 and over in 2020. Approximately 52.8% of the ≥50 employees are women (n = 3045) vs. 47.2% (n = 2723) men. In our 1030 online survey participants (17.9% of the 5768 older employees) 67.8% (n = 708) of them were women vs. 32.3% (n = 317) men, reflecting the general phenomena of low response rate from men observed in most studies [30]. The race/ethnicity breakdown at the UA for this age group was: 65.0%, 20.4%, 4.2%, 1.9%, and 0.9% for non- Hispanic white, Hispanic white, Asian, Black or African American, and American Indian or Native American, respectively. The race/ ethnicity distribution in the online survey participants was 77.3%, 7.3%, 1.7%, 2.5%, and 0.5% for non-Hispanic white, Hispanic white, Asian, Black, or African American, and American Indian or Nativ American, respectively, showing the needs to increase minority participation in studies like this [31].
The distribution for job classification in this age group was 6.9%, 4.6%, 28.0%, 40.4%, and 1.1% for Academic Professionals, administrative, faculty, staff, and post-doc/students at the University of Arizona in 2020. In our online survey, respondents were 3.5%, 10.2%, 21.6%, 62.5%, and 0.1% for Academic Professionals, administrative, faculty, staff, and postdoc/students (graduate student assistants or student workers), showing Academic Professionals’ and staff’s participations were higher than other groups while post-doc and student workers were lower in this survey sample. The major strengths of this study include taking the community participatory approach, using mixed methods, building our intervention based on needs assessment, and implementing online intervention which is critical during the pandemic. Using a community-based participatory research approach was extremely important to allow us to quickly engage the targeted community and accomplish our research objectives to address the concerns and needs of the participants. The community advisory board with representatives from diverse units of the campus contributed to the three phases of the study and was critical in helping with recruitment, needs assessments, and interpreting the study findings. For example, to capture people’s concerns with the campus reopening before the beginning of the fall semester, we had less than 2 months to complete Phase 1 of the study which included recruiting CAB members, conducting focus group interviews, completing primary data analysis on the interview, constructing a survey questionnaire and collecting online survey data from over 1000 participants. The CAB members provided strong support for our recruitment by suggesting recruitment strategies and directly helping recruit participants. CAB members were instrumental in helping form focus group interview questions and developing the online survey questionnaire in phase 1 of the study. CAB members worked with the team extensively during phase 2 of the study to identify the most desirable and feasible interventions addressing the needs of the community in a short preparation time. The intervention of phase 3 started by the end of October which gave us 6 weeks for the intervention and additional time for the focus group after the intervention before the holiday break.
In the first phase of this study the mixed methods research approaches were fundamental for us to first identify the dominants for the survey and then construct and implement the survey. In the third phase of this study, we gained appreciative information from both the qualitative and quantitative data on intervention effects and areas for improvements in future interventions. The use of mixed methods throughout the needs assessment and intervention phases of the project allows us to combine the power of words and the power of numbers to best capture participants’ concerns and their evaluation and feedback on the interventions [32]. With both quantitative and qualitative data, this study has the potential to enrich our understanding of the concerns and needs of older employees in higher education. The multiple stages of the project guided focused effort with clear goals to build and to execute the project in an extremely short period of time. As indicated above, this study is limited in the diversity of participants, and also inperson measures were not possible in the midst of the pandemic.
Conclusion
In conclusion, the Saguaro Study program was designed to survey and conduct interventions among UA older employees during the COVID-19 pandemic, but the results can be used to inform future study and policy in higher education. Using mixed methods, a community participatory approach, and multiple research components, the Saguaro Study program presents great opportunities for us to understand concerns and needs of older employees in higher education. The findings from pilot interventions will contribute to developing age-appropriate health promotion programs for older employees at universities.
Ethics Approval
University of Arizona IRB Approved
Consent
Formal consenting was done within REDCap with an electronic signature from the participants.
Data, Material and/or Code availability
The data that support the findings of this study are available from the corresponding author upon request.
Authors’ Contribution Statement
Zhao Chen: Obtaining funding, study design, supervision of research team, data analysis, manuscript writing and review; Mark Wager: Participant recruitment, consenting, data collection, interpretation of results, manuscript review; Kathie Insel: Participant recruitment, study design, interpretation of results, manuscript review; Hamza Butt: Data analysis and presentation; Yunjia Yang: Intervention, data collection, data management, manuscript writing and review; Dagoberto Robles: Intervention, manuscript review; Kendra Jason: Manuscript writing and review; Amanda Sokan: Qualitative data collection, community advisory board, manuscript writing and review; Heather Kenning: Intervention, data collection, manuscript writing and review; Marc Verhougstraete: Study design, intervention, data collection, manuscript review; Lisa O’Neill: Study design, manuscript review; Mindy Fain: Study design, manuscript review; Linda Philips: Study design, data collection, manuscript review ; Kiranmayee Muralidhar: Manuscript writing and review; Nicole Yuan: Study design, qualitative data collection and analysis, community advisory board, interpretation of findings, manuscript writing.
Acknowledgement
This study was funded by the University of Arizona.
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
References
- Israel BA, Eng E, Schulz AJ, Parker EA (2005) Introduction to methods in community-based participatory research for health. Methods in Community-Based Participatory Research for Health 3: 26.
- Rollins L, Carey T, Proeller A, Anne Adams M, Hooker M, et al. (2021) Community-based participatory approach to increase African Americans’ access to healthy foods in Atlanta, GA. Journal of Community Health 46(1): 41-50.
- Graybill P, Aggas J, Dean RK, Demers S, Finigan EG, et al. (2010) A community-participatory approach to adapting survey items for deaf individuals and American Sign Language. Field Methods 22(4): 429-448.
- Kim S, Koniak-Griffin D, Flaskerud JH, Guarnero PA (2004) The impact of lay health advisors on cardiovascular health promotion: using a community-based participatory approach. Journal of Cardiovascular Nursing 19(3): 192-199.
- Brewer LC, Hayes SN, Caron AR, Derby DA, Breutzman NS, et al. (2019) Promoting cardiovascular health and wellness among African-Americans: community participatory approach to design an innovative mobile-health intervention. PloS One 14(8): e0218724.
- Vaughn LM, Jacquez F (2020) Participatory research methods--choice points in the research process. Journal of Participatory Research Methods: 1(1).
- Collins SE, Clifasefi SL, Stanton J, Straits KJE, Gil-Kashiwabara E, et al. (2018) Community-based participatory research (CBPR): Towards equitable involvement of community in psychology research. American Psychologist 73(7): 884-898.
- Kemp CL, Ball MM, Morgan JC, Doyle PJ, Burgess EO, et al. (2017) Exposing the backstage: Critical reflections on a longitudinal qualitative study of residents’ care networks in assisted living. Qualitative Health Research 27(8): 1190-1202.
- Reade N (2013) The Surprising Truth About Older Workers Here’s one: Their strengths can make them the most valuable people in the office. AARP The Magazine.
- Van Droogenbroeck F, Spruyt B (2016) I ain’t gonna make it. Comparing Job Demands-Resources and attrition intention between senior teachers and senior employees of six other occupational categories in Flanders. International Journal of Aging and Human Development 83(2): 128-155.
- Pritchard A, Li J, McChesney J, Bichsel J (2019) The Challenges of an Aging Higher Ed Workforce. College and University Professional Association for Human Resources.
- S. Bureau of Labor Statistics (2020) Labor Force Statistics from the Current Population Survey.
- Wilson E, Donovan CV, Campbell M, Chai T, Pittman K, et al. (2020) Multiple COVID-19 Clusters on a University Campus — North Carolina, August 2020. MMWR. Morbidity and Mortality Weekly Report: 69(39): 1416-1418.
- Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, et al. (2020) Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addictive Behaviors 110: 106527.
- Marelli S, Castelnuovo A, Somma A, Castronovo V, Mombelli S, et al. (2021) Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology: 268(1): 8-15.
- Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, et al. (2020) COVID-19 and Older Adults: What We Know. In Journal of the American Geriatrics Society 68(5): 926-929.
- Mayo Clinic Staff (2024) COVID-19: Who’s at higher risk of serious symptoms? Mayo Clinic.
- Gould E (2020) Older workers can’t work from home and are at a higher risk for COVID-19. Economic Policy Institute.
- Andrasfay T, Goldman N (2021) Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proceedings of the National Academy of Sciences of the United States of America: 118(5): e2014746118.
- Jason K, Wilson M, Catoe J, Brown C, Gonzalez M (2024) The impact of the COVID-19 pandemic on Black and Hispanic Americans’ works outcomes: A scoping review. Journal of Racial and Ethnic Health Disparities 11(3): 1157-1172.
- Gallagher S, Roy A, Domeracki SJ, Mohrmann T, Missar V, et al. (2021) The low-wage essential worker: Occupational concerns and needs in the COVID-19 pandemic-A round table. Workplace Health \& Safety 69(4): 154-160.
- Arizona Public Health Association (2021) AzPHA Total Mortality Report Finds 36,000 Excess Deaths Occurred in AZ During the Pandemic - The Largest Percent Increase in Excess Deaths of Any State. Arizona Public Health Association.
- Watts A, Au NH, Thomas-Bachli A, Forsyth J, Mayah O, et al. (2020) Potential for inter-state spread of Covid-19 from Arizona, USA: analysis of mobile device location and commercial flight data. Journal of Travel Medicine 27(8): taaa136.
- (n.d.). DATAUSA: UNIVERSITY OF ARIZONA. DATAUSA.
- Yuan NP, Mayer BM, Joshweseoma L, Clichee D, Teufel-Shone NI (2020) Development of guidelines to improve the effectiveness of community advisory boards in health research. Progress in Community Health Partnerships: Research, Education, and Action: 14(2): 259-269.
- Baer R, Gu J, Strauss C (2022) Five facet mindfulness questionnaires (FFMQ) In Handbook of Assessment in Mindfulness Research. Cham: Springer International Publishing.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research 28(2): 193-213.
- Polar, Polar H9 Heart Rate Sensor.
- Stein D, Rocco TS, Goldenetz KA (2000) Age and the university workplace: A case study of remaining, retiring, or returning older workers. Human Resource Development Quarterly 11(1): 61-80.
- Ding EL, Powe NR, Manson JE, Sherber NS, Braunstein JB (2007) Sex differences in perceived risks, distrust, and willingness to participate in clinical trials: a randomized study of cardiovascular prevention trials. Archives of Internal Medicine 167(9): 905-912.
- De Las Nueces D, Hacker K, DiGirolamo A, Hicks LS (2012) A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Services Research 47(3pt2): 1363-1386.
- Pluye P, Hong QN (2014) Combining the power of stories and the power of numbers: Mixed methods research and mixed studies reviews. Annual Review of Public Health 35: 29-45.
-
Zhao Chen*, Yunjia Yang, Kendra Jason, Mark Wager, Kathleen C Insel.et,all. A Community-Based Participatory Approach for Needs Assessment and Intervention: A Mixed Methods Study Program of Older University Employees During COVID-19. Glob J Aging Geriatr Res. 3(4): 2025. GJAGR. MS.ID.000568.
-
COVID-19, Older Employees, Health Research, Pandemics, Women Caregivers
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






