Review Article
Review Article
COVID 19 and Diabetes: What have we Learnt
Shambo Samrat Samajdar1*, Jyotirmoy Pal2, Sougata Sarkar3 and Saibal Das4
1Department of Clinical & Experimental Pharmacology, School of Tropical Medicine, Kolkata & Consultant, Diabetes & Allergy-Asthma Therapeutics Specialty Clinic, India
2Department of General Medicine, R G Kar Medical College & Hospital, India
3Department of Clinical & Experimental Pharmacology, School of Tropical Medicine, India
4Department of Health Research, Ministry of Health and Family Welfare, Government of India, India
Shambo Samrat Samajdar, MBBS MD DM (Clinical Pharmacology) PG Dip Endo & Diabetes (RCP) Fellowship in Respiratory & Critical Care (WBUHS); Clinical Pharmacologist, Department of Clinical & Experimental Pharmacology, School of Tropical Medicine, Kolkata & Consultant, Diabetes & Allergy-Asthma Therapeutics Specialty Clinic, Kolkata, India.
Received Date: December 02, 2022; Published Date: December 19, 2022
Introduction
Diabetes is associated with suppressed innate and humoral immune functions. Diabetes and related macrovascular, microvascular complications increase the risk of morbidity and mortality during acute infections. In a study it had been shown that there is 60% increased risk of hospitalization and pneumoniarelated severity during bacterial infection if HbA1c is more than 9% [1]. We had witnessed increased morbidity and mortality during previous viral pandemics. The presence of diabetes was considered to be an independent risk factor for development of complications and mortality during SARS CoV1 epidemic in 2002 -2003 [2]. Diabetics had three times more risk of getting hospitalized and four times higher risk of admission in intensive care unit during Influenza A (H1N1) infection outbreak [3]. In another study done during MERS epidemic, it was found that mortality rate in diabetics was 35% [4].
After more than 1·5 years with pandemic of SARS-CoV-2, it has been seen that diabetes patients are more susceptible to severe COVID-19. They are also having increased risk of postacute sequelae of COVID-19 and vaccine breakthrough. Patient suffering from chronic non communicable diseases like diabetes, hypertension, and cardiovascular disease (CVD), COVID 19 infection is common. After pooled analysis from 10 studies including 2209 COVID-19 patients, conducted in China it was found that prevalence of hypertension, diabetes and CVD in 21%, 11%, and 7% patients, respectively. In a meta-analysis of 8 trials including 46,248 COVID19 patients, prevalence was found to be 17%, 8%, and 5% for hypertension, diabetes and CVD respectively [5]. Prevalence rate differs in studies conducted in Europe and USA. One study conducted in Italy had shown prevalence of diabetes is nearly 36% of 355 admitted COVID-19 patients [6]. Another study from Italy including 481 patients it was seen that 34% of the mortality in COVID 19 patients were suffering from diabetes [7]. Centers for Disease Control and Prevention (CDC), USA had reported from the database of 7162 COVID-19 patients, 11% were diabetics [8]. Different studies were suggesting that diabetic COVID 19 patients had severe or critical disease, prevalence varying from 14% to 32% [9]. In a study including 138 COVID 19 patients ICU admission rate was 72% patients of COVID-19 with comorbidities including diabetes, compared to 37% of patients without comorbidities [10]. Another study including 201 COVID-19 patients it was found that for development of acute respiratory syndrome (ARDS) diabetic patients had a hazard ratio (HR) of 2.34 (95% CI, 1.35 to 4.05; p < 0.002). One meta-analysis including 9 studies from China with a sample size of 1936 had suggested a significant correlation between severity of COVID-19 and diabetes (OR, 2.67, 95% CI; 1.91 to 3.74; p < 0.01) [11]. Various studies had reported the prevalence of nonsurvivors was unfortunately high among diabetics with COVID-19. According to those studies it was varying between 22 to 31% [12]. Diabetes and COVID 19 may act synergistically to produce atrocities which need urgent attention and holistic multidisciplinary care.
“COVID Approach” In Diabetic COVID 19 Patients
While attending our diabetic individuals suffering from COVID 19 infection we need to consider a “COVID approach”.
C – Complications
Diabetes associated macro and micro vascular complications need to be evaluated. In the presence of associated complications, the prognosis worsens. If a patient has microalbuminuria, he may land up with macro-albuminuria and finally could experience end stage kidney disease. As the presence of cardiovascular disease (CVD) independently increases morbidity and mortality in COVID 19 patients, common associated subclinical CVD needs special attention while treating COVID 19 patients.
O – Obesity & Other Comorbidities
Obesity is individually considered as a high-risk factor for COVID 19 patients. Obesity increases COVID 19 related hospitalization risk by 3 times and 1.42 times higher risk when hospitalized, of severe illness (intensive care unit admission, invasive mechanical ventilation, or death). Diabetic COVID 19 patients need evaluation of presence of other comorbidities like hypertension, dyslipidemia etc. As other comorbidities increase mortality, they should be adequately addressed [12].
V – Viscosity
COVID-19 infection is a pro-thrombotic state, with elevated level of fibrin, fibrin degradation products, fibrinogen, and D-dimers [13]. These factors contribute to hyper viscosity in COVID 19. Hyper viscosity is responsible for damaging endothelium leading to thrombosis. Endothelial dysfunction, coagulation system activation and platelet hyper-reactivity make diabetes a prothrombotic state. Thrombosis is one of the major contributing factors behind diabetes mellitus associated morbidity and mortality [14]. This issue should be addressed well, and rational risk benefit analysis should be done with utilization of antiplatelet and or antithrombotic agents in COVID 19 infected diabetics.
I – Insulin
In-hospital hyperglycemia in the presence of COVID-19 is better managed with insulin as it is the safest option. Inertia to insulin should be properly addressed in COVID 19 infected patients to optimize glycemic control. Hypoglycemia education and insulin injection technique require urgent attention especially when patients are being treated from telemedicine platform. Antiinflammatory pleiotropic action could be beneficial for patients but optimizing dose is very important to prevent hypoglycemic atrocities [15].
D – Dysregulated Immunity
Immune system dysregulation is a key pathogenic factor to produce insulin resistance and dysglycemia in COVID 19 infected patients. A few patients experiencing severe COVID 19 have cytokine release syndrome which is associated with elevated level of IL-6. IL-6 increases oxidative stress and damage proteins, lipids and DNA. SARS-CoV-2 infection produces an increase in the level of reactive oxygen species (ROS). Viral activation of the renin– angiotensin–aldosterone system (RAAS) is aggravated by ROS which leads to insulin resistance, hyperglycaemia and vascular endothelial damage. Diabetes and dysregulated immune system is strongly associated and they are linked to accelerated ageing. Obesity phenotype is responsible to produce pro-inflammatory cytokines with T helper type 1 responses and T helper type 17 responses. They are responsible to increase insulin resistance. T helper type 1 and T helper type 17 pathways are predominant in COVID 19 infection. Low NK cell activity in hyperglycemia is well evidenced by different studies. These factors may majorly contribute by placing diabetes as an independent risk factor for COVID 19 related mortality and morbidity. A thorough knowledge on immune system dysregulation occurring during SARS-CoV-2 infection is extremely important to understand the targets and developing therapeutics [16]. Dysregulated immunity should be addressed during management and there should not be any inhibition due to fear of steroid induced hyperglycemia to start corticosteroid therapy like dexamethasone when indicated. Rationalized insulin protocol in respective patients on steroid therapy would prevent harm by steroid which is a double-edged sword.
Pathogenesis
In β cells it had been found that ACE2 and related SARS CoV 2 entry factors (TMPRSS2, NRP1, and TRFC) are expressed. There is selective high expression of neuropilin 1 (NRP1). Pancreatic β cells are infected by SARS-CoV-2 in COVID 19 patients, which lead to attenuation of insulin levels and secretion from pancreas. This is also responsible for β cell apoptosis [17]. In diabetes ACE 2 upregulation occurs in pancreas [18]. Hyperglycemic state aggravates SARS CoV2 induced pancreatic β cell dysregulation and destruction.
Vascular perfusion is compromised in diabetes. In the presence of hyperglycemia glucose is going to deposit on the endothelial surface protein structure and also passes towards basement membrane and produce network of fused glycated protein products by non-enzymatic glycosylation. This is responsible for atherosclerosis. Endothelial dysfunction and narrowing of blood vessels lead to lesser perfusion to tissues. SARS CoV 2 infected persons require good perfusion to tissues like lungs but in presence of compromised vascular perfusion tissue damage would be aggravated. Increased insulin resistance will cause elevated free fatty acid (FFA) levels. There is also abundance of ROS in COVID 19 infection which is also elevated in diabetic subjects. Increased FFA also produces ROS. The combined effects of atherosclerosis, high FFA and elevated ROS are responsible for COVID 19 related increased morbidity and mortality.
Defective carbohydrate metabolism, increased FFA is responsible for acidic environment in diabetics. Relative increase in acidity of environment causes immune cells not reacting properly. The immune system function is disrupted. In obese patients’ hypertrophic adipocytes are infiltrated with pro-inflammatory immune cells producing cytokines, chemokines, and adipokines. Patients may land up into an irreversible inflammatory phenotype by hyper reactive white adipose tissue. In the presence of insulin resistance there would be enhanced infiltration of M1 macrophages into adipose tissue and increased production of proinflammatory cytokines like IL 6, IL -1 beta and TNF alpha. Chronic inflammation and immune dysregulation aggravate COVID-19 symptoms in a synergistic way. Severe form of COVID-19 is mostly caused by metainflammation and a cytokine storm [19].
The interplay between non-communicable disease (diabetes) and communicable disease (COVID 19 infection) is extremely important to be understood. On one hand, diabetes aggravates the risk of developing severe COVID-19 or breakthrough infections following COVID 19 vaccination. On the other hand, SARS CoV2 infection would lead to produce new-onset diabetes or complicating already existing diabetes mellitus.
Essential Steps to be Taken for Diabetics
1. Encourage diabetics to have restricted social contact and practice social distancing to reduce risk of infection.
2. We need to prioritize diabetes patients to give COVID 19 vaccination. It is also essential to educate them regarding chances of breakthrough COVID 19 infections and continue following SMS (social distancing, mask use correctly and sanitization) protocol like before. Scientists need to explore the need and justification of booster. Influenza and pneumonia vaccination need to be properly scheduled in diabetes subjects.
3. Proper counselling and encouragement of diabetes patients are essential to develop a healthy lifestyle during lockdown and quarantine.
4. Individualization of management is required to incorporate a personalized set of self-management goals (measurement of heart rate, weight, waist circumference, capillary blood glucose, steps per day and blood pressure) and adherence to these goals.
5. Digital support is extremely crucial for helping out diabetics to utilize online health education, diet counselling, virtual consultation, and digitalized health records.
6. Behavioral support and psychological counselling to help patients to combat against stress.
7. Intensification of foot care and eye care is required. Digital retinal examination using artificial intelligence could be immensely helpful.
8. Screening for new onset diabetes is needed.
9. Prompt identification and management of cardiac risk factors should be emphasized. Adherence to lipidlowering drugs should be monitored and patients should be educated on their importance. Selection of anti-diabetes agents (empagliflozin, dapagliflozin, liraglutide, dulaglutide, semaglutide etc) having shown to be beneficial in established or high cardiovascular disease risk patients need to be considered.
10. Monitoring of urinary albumin creatinine ratio, serum creatinine, progression of edema in patients with chronic kidney disease need specific attention.
Target Range [20]
For OPD Consultation
a) Plasma glucose concentration: 72–144 mg/dL [Target lower plasma glucose concentrations can be adjusted to 90 mg/ dL in frail patients to prevent hypoglycemia]
b) HbA1c: less than 7% [HbA1c testing is not always possible, but previous reports if available guide prescriber to differentiate between chronic and acute decompensation]
c) CGM/FGM targets: TIR (70-180 mg/dl): more than 70% (in case of frail and elderly patients cut off is changed to >50%) & Hypoglycemia (<56 mg/dl): should be less than 4% (in case of frail and elderly patients cut off is changed to <1%)
For In-patient or Intensive Care Unit
72–180 mg/dL [Target lower plasma glucose concentrations can be adjusted to 90 mg/dL in frail patients to prevent hypoglycemia]
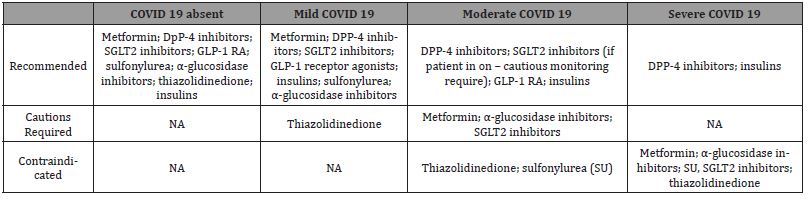
Anti-diabetes Drugs in COVID 19 Diabetics [15]
Metformin
Dehydration status should be evaluated carefully regarding decision making on metformin initiation and continuing as chance of lactic acidosis will be more if patients are dehydrated. Patients should be educated regarding stopping the drug in presence of dehydration. They need to follow sick day rules. Function of kidney should be vigilantly monitored because of underlying probability of chronic kidney disease or chance of developing acute kidney injury.
Pioglitazone
Volume overload is an important consideration of pioglitazone use. It should be better to avoided in COVID 19 patients especially in moderate and severe COVID 19 cases.
Sodium-glucose-co-transporter 2 inhibitors
Drugs like canagliflozin, dapagliflozin, and empagliflozin carry the risk of dehydration and diabetic ketoacidosis if patients are suffering from infection. It is wiser from perspectives of patients to stop taking this group of drugs and follow sick day rules. Patients suffering from acute respiratory illness need to stop this group of drugs. As there is a possibility of acute deterioration of renal function, eGFR should be carefully monitored.
Glucagon-like peptide-1 receptor agonists (GLP1 RA)
Dulaglutide, exenatide, liraglutide, lixisenatide are available in India. New initiation may cause gastrointestinal adverse effects which may aggravate dehydration already present in COVID 19 patients and develop a serious illness. A few animal studies had shown that GLP-1R agonists reduced pulmonary inflammation and decreased production of cytokine. In one mice model study, GLP-1R agonists reduce pulmonary type 2 immune cytokine responses in response to a respiratory syncytial virus isolated from a child with severe lower respiratory tract infection. But we have insufficient experience and clinical data on safety to prescribe GLP-1R agonists in critically ill subjects. We need to conduct randomized controlled trials (RCTs) to justify use of GLP1 RA in the context of coronavirus infection. Adequate fluid intake and regular small and timely meals should be encouraged if patients are on GLP1 RA.
Dipeptidyl peptidase-4 inhibitors (DPP4 I)
Alogliptin, linagliptin, saxagliptin, teneligliptin and sitagliptin are widely used anti-diabetes agents in Indian context. They have the least adverse effects, well tolerated and can be continued. There is least chance of hypoglycemia. There is one concern regarding immune reactions of DPP4 I and their immunogenic effects on COVID-19. Impaired T cell-dependent immune responses with DPP4 inhibitors are not clinically relevant as per different clinical studies. DPP4 I can safely be used in COVID 19 patients.
Insulin
Insulin therapy should be continued in COVID 19 patients. Selfmonitoring of blood-glucose should be regularly advocated as per the type of insulin schedule. Some of them may require continuous glucose monitoring. Adjusting the dose and type of insulin should be done carefully to reach treatment goals depending on age, type of diabetes, comorbidities, duration of diabetes, BMI and life expectancy. Telemedicine and digital health should be utilized optimally for proper management. Virtual health education programs need to be promoted for ensuring adherence of patients to therapy. In the following table 1 we are going to summarize role of different anti-diabetes agents in background of COVID 19 (Table 1) [21].
Table:Use of different anti-diabetes agents in background of COVID 19[21].
Steroid Induced Hyperglycemia
In-hospital management of moderate to severe COVID 19 cases requires corticosteroid therapy as a backbone. In mild symptomatic cases with raised inflammatory markers physicians need to initiate timely corticosteroid as per their clinical judgments. A study had showed that 64% of in-hospital patients receiving glucocorticoids equivalent to prednisolone ≥40 mg had developed hyperglycemia [22]. Corticosteroid induced hyperglycemia cases are increasing among preexisting diabetics. Steroid induced diabetes is a complicated disease outcome. As India had faced an epidemic of mucormycosis it is now extremely important to acknowledge the importance of good glycemic control in COVID 19 patients especially those are on corticosteroids. Glycemic control along with reducing incidence of hyperglycemia and glycemic variability is extremely important to achieve good outcome. In a RCT it had been seen that using correctional insulin matching with pharmacokinetic and pharmacodynamics property of prescribed steroid and adjusting the dose of insulin with respective corticosteroid dose had produced lower mean blood glucose and lower glycemic variability compared to conventional basal bolus arm [23].
Role of Other Drugs
ACE inhibitors and ARB regulate ACE-2. Mice model with coronavirus induced lung injury had shown improvement by losartan [24]. A retrospective study had suggested that viral pneumonia patients who were continuing ACE inhibitors, required a smaller number of endotracheal intubation and incidences of mortality [25]. There was a controversy regarding the increase in the risk of COVID 19 infection due to upregulation of ACE 2 by ACE I or ARB. But clinical studies are not supporting this hypothesis currently. In a record based observational study conducted in West Bengal it was found that increased age, male sex and presence of co-morbidities like diabetes, COPD were significantly associated with the incidence of moderate and severe COVID 19. ACE I or ARB usage were associated with less severe disease. Though this association was not achieved statistical significance [26]. European Society of Cardiology Council on Hypertension, European Society of Hypertension and American Heart Association had recommended continuing using ACE inhibitors and ARB [27-29].
Several studies had suggested the protective role of statins in pneumonia [30]. Hypothetically statins inhibit nuclear factor kappa B (NFkB) activation and may be beneficial in reducing the cytokine release syndrome [31]. One retrospective study including 2626 patients had concluded that antecedent use of statin use was associated with lower inpatient mortality in hospitalized with COVID-19 patients [32].
Conclusions
During the COVID-19 pandemic, diabetes patients should be aware that COVID-19 can impair glycemic control. They need to strictly adhere to guidelines for the management of diabetes. A healthy diet and physical activity schedule should be followed. If patients have symptoms like dry cough, excessive sputum production or fever, or shortness of breath or show sudden hyperglycemia, they should consult their physician urgently. Early identification and prompt treatment with Mab cocktail could be beneficial. Delaying testing should be discouraged strongly. SMS (social distancing, mask use correctly and sanitization) protocol should be followed like before even after taking vaccination. Possibility of breakthrough COVID 19 post vaccination is present. Scientists need to explore on booster dose of vaccine. Telemedicine, digital health and remote consultations need strengthening to serve mass. Inertia to insulin needs to be overcome. Other antidiabetes agents need proper evaluation of risk-benefit analysis before prescribing.
Acknowledgment
None.
Conflict of Interest
No Conflict of Interest.
References
- Akbar DH (2001) Bacterial pneumonia: comparison between diabetics and non-diabetics. Acta Diabetol 38(2): 77-82.
- Yang JK, Y Feng, MY Yuan, SY Yuan, HJ Fu, et al. (2006) Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med 23(6): 623-628
- Robert Allard, Pascale Leclerc, Claude Tremblay, Terry Nan Tannenbaum (2010) Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care 33(7): 1491-1493.
- Basem M Alraddadi, John T Watson, Abdulatif Almarashi, Glen R Abedi, Amal Turkistani, et al. (2016) Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans. Saudi Arabia 2014. Emerg Infect Dis 22: 49-55.
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, et al. (2020) Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis 94: 91-95.
- Onder G, Rezza G, Brusaferro S (2020) Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323(18): 1775-1776.
- Covid-19 surveillance group, Italy.
- CDC COVID-19 response team (2020) Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, february 12-march 28, 2020. MMWR Morb Mortal Wkly Rep 69(13): 382-386.
- Awadhesh Kumar Singh, Ritesh Gupta, Amerta Ghosh, Anoop Misra (2020) Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr 14 (4): 303-310.
- Dawei Wang, Bo Hu, Chang Hu, Fangfang Zhu, Xing Liu, et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronaviruse infected pneumonia in wuhan, China. JAMA 323(11): 1061-1069.
- Chen Y, Gong X, Guo J Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: a systematic review and meta-analysis.
- Lyudmyla Kompaniyets, Nickolas T Agathis, Jennifer M Nelson, Leigh Ellyn Preston, Jean Y Ko, et al. (2021) Underlying medical conditions associated with severe COVID-19 illness among children. JAMA network open 4(6): e2111182-e2111182.
- Shambo Samrat Samajdar, Priya Ann Sam, Saibal Moitra, Yogiraj Ray, Jyotirmoy Pal, et al. (2020) Risk Benefit Analysis in Reference to use of LMWH in COVID-19. J Assoc Physicians India 68(9): 52-61.
- Natale Vazzana, Paola Ranalli, Chiara Cuccurullo, Giovanni Davi (2012) Diabetes mellitus and thrombosis. Thromb Res 129(3): 371-377.
- Samajdar SS, Dasgupta S, Tripathi SK (2020) Management of Hyperglycemia in In-hospital COVID-19 Patients: A Review. Bengal Physician Journal 7(2): 31-34.
- Soo Lim, Jae Hyun Bae, Hyuk Sang Kwon, Michael A Nauck (2021) COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol 17(1): 11-30.
- Chien Ting Wu, Peter V Lidsky, Yinghong Xiao, Ivan T Lee, Ran Cheng, et al. (2021) SARS-CoV-2 infects human pancreatic β cells and elicits β cell impairment. Cell Metab 33(8): 1565-1576.
- Jan Wysocki, Minghao Ye, Maria José Soler, Susan B Gurley, Hong D Xiao, et al. (2006) ACE and ACE2 activity in diabetic mice. Diabetes 55(7): 2132-2139.
- Charlotte Steenblock, Stefanie Richter, Ilona Berger, Marko Barovic, Janine Schmid, et al. (2021) Viral infiltration of pancreatic islets in patients with COVID-19. Nat Commun 12(1): 3534.
- Stefan R Bornstein, Francesco Rubino, Kamlesh Khunti, Geltrude Mingrone, David Hopkins, et al. (2020) Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol 8(6): 546-550.
- Daniel J Drucker (2020) Coronavirus Infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr Rev 41(3): bnaa011.
- Donihi AC, Raval D, Saul M, Korytkowski MT, DeVita MA (2006) Prevalence and predictors of corticosteroid related hyperglycemia in hospitalized patients. Endocr Pract 12(4): 358-362.
- Lakhani Om J, Kumar Surender, Tripathi Sudhir, Desai Mitali, Seth Chandani (2017) Comparison of two protocols in the management of glucocorticoid-induced hyperglycemia among hospitalized patients. Indian J Endocrinol Metab 21(6): 836-844.
- Yang P, Gu H, Zhao Z, Wang W, Cao B, et al. (2014) Angiotensin-converting enzyme 2 (ACE2) mediates influenza H7N9 virus-induced acute lung injury. Sci Rep 4: 7027.
- Henry C, Zaizafoun M, Stock E, Ghamande S, Arroliga AC, et al. (2018) Impact of angiotensin-converting enzyme inhibitors and statins on viral pneumonia. Proc (Bayl Univ Med Cent) 31(4): 419-423.
- Bhattacharyya A, Halder S, Mandal T, Sadhukhan SK, Samajdar SS, et al. (2021) Effect of Angiotensin Converting Enzyme Inhibitors/Angiotensin Receptor Blockers on COVID-19 outcome: A Record Based Observational Study in West Bengal. J Assoc Physicians India 69(7): 11-12.
- (2020) Position statement of the ESC Council on hypertension on ACE-inhibitors and angiotensin receptor blockers.
- (2020) ESH statement on COVID-19.
- HFSA/ACC/AHA statement addresses concerns Re: using RAAS antagonists in COVID-19.
- Batais MA, Khan AR, Bin Abdulhak AA (2017) The use of statins and risk of community-acquired pneumonia. Curr Infect Dis Rep 19(8): 26.
- Yuan S (2015) Statins may decrease the fatality rate of Middle East respiratory syndrome infection. mBio 11;6(4): e01120.
- Aakriti Gupta, Mahesh V Madhavan, Timothy J Poterucha, Ersilia M DeFilippis, Jessica A Hennessey, et al. (2021) Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Nat Commun 12(1): 1325.
-
Shambo Samrat Samajdar*, Jyotirmoy Pal, Sougata Sarkar and Saibal Das. COVID 19 and Diabetes: What have we Learnt. Endo & Diab Opn Acc J. 1(1): 2022. EDOAJ.MS.ID.000504.
-
Microvascular complications, Cardiovascular disease, Morbidity, Hyper viscosity, Thrombosis, D-Dysregulated Immunity, Hypoglycemia, Chronic kidney disease, Pioglitazone, Inhibitors, Pharmacokinetic, Pharmacodynamics property
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.