Research Article
Research Article
A Pilot Study of a Diabetes Project ECHO for Healthcare Trainees
Nicole Ehrhardt1*, Sanjana Rao2 and Annette Aldous3
1The George Washington University as Assistant Professor of Medicine and is currently at the University of Washington Medicine Diabetes Institute, USA
2The George Washington University and now an internal medicine resident at the University of Miami, USA
3The George Washington University Milken Institute School of Public Health, Washington, USA
Nicole Ehrhardt, Assistant Professor of Medicine UW Medicine Diabetes Institute, 750 Republican Street Building F, Floor 3, Seattle, WA 98109, USA.
Received Date: December 8, 2022; Published Date: December 16, 2022
Abstract
Background: As the prevalence of diabetes increases and the number of specialists, decline advanced diabetes training for those joining clinical practice is needed. One model to improve access to care for diabetes may be the tele-mentoring ECHO model. ECHO programs have traditionally targeted primary care providers, but no one has evaluated its use in those in pre-clinical practice such as physician assistant students (PAS).
Methods: Over 3 cycles of ECHO sessions from 2018-2021, we engaged 42 PA students. Using didactics and case-based learning via videoconferencing, the ECHO model allowed participants to receive tele-mentoring from an endocrinologist, a diabetes educator, and rotating specialists. Pre and post course surveys measured self-efficacy (13 questions), confidence in management (6), factual knowledge (12) and prescribing practices (11).
Results: Twenty-three PAS completed at least 50% of sessions; 18 completed both evaluations. On a Likert scale, self-efficacy increased from 3.18 (slightly competent) pre-intervention to 4.79 (competent) post (p<.0001). Confidence increased from 3.32 (neutral) to 5.33 (somewhat confident) (p<.0001). PAS correct answers for factual knowledge increased after intervention to 5.76 (p<0.01) Students’ anticipated frequency of prescribing diabetes medication (n=12) increased from 1.73 (rarely) to 3.11 (sometimes) (p<.001) and of technology from 1.46 to 2.79 (p<.001).
Conclusions: Our ECHO model is the first to evaluate healthcare trainees. PAS showed improved DM self-efficacy, knowledge, and comfort prescribing medications. However, overall participation of students in live sessions was low. Further research is needed to assess incorporation of pre-recorded/ “OnDemand” ECHO sessions into healthcare trainee curriculum and evaluate patient level benefit.
Introduction
It is no secret that diabetes and its complications, deaths, and consequent societal burden have significantly impacted the United States over the last 30 years. Between 1990 and 2010, the prevalence of diabetes tripled and incidence doubled, with nearly half of the US diabetes population having poorly controlled diabetes. [1, 2] Specifically in Washington D.C., approximately 12.3% of the district’s adult population were reported to have diabetes in 2014 and it was the fifth leading cause of death with 144 deaths, above chronic respiratory lower diseases, Alzheimer’s, HIV/ AIDS, or homicides. [3,4] Despite this urgent need to aggressively address the diabetes epidemic, studies demonstrate a shortage of adult endocrinologists to satisfy current and future demand. [5] While the number of endocrine specialists continue to decline, NP and PA providers numbers continue to grow [6] and rapidly join the primary care work force. These providers’ training in complex diabetes management is limited. Lack of endocrine expertise is concerning as it is well established that early, active endocrinologist involvement in longitudinal diabetes care results in delayed development of diabetes-related complications and improved survival. [4, 5]. In contrast, individuals with poor access to care are closely linked with poor glycemic control and consequent higher morbidity and mortality due to a multitude of sociodemographic barriers, including financial struggles, lack of social support, and educational insufficiency. [7-11] Therefore, there is growing interest worldwide in shifting the paradigm of healthcare delivery to connect complex endocrine patients in underserved communities with limited specialty expertise.
Recently, telemedicine has been increasingly implemented as a means to improve access to quality care for those who face geographic barriers. [12] With regards to diabetes care, incorporation of telemedicine has resulted in better glycemic control and high patient satisfaction. [13,14] A recent review of telemedicine and diabetes showed that the telemedicine platform was feasible and effective but also concluded that telehealth in diabetes should focus on how to leverage technology “to increase access to marginalized patient.” [13] Project ECHO (Extension for Community Healthcare Outcomes) may be one way to improve access to care in vulnerable populations. ECHO, an innovative and collaborative telemedicine model, was first established at the University of New Mexico Health Sciences Center to improve access to treatment for hepatitis C in rural communities. [15] After being recognized as safe and effective, the model has been utilized for a myriad of health conditions, including HIV, osteoporosis, chronic pain, autism, behavioral health in geriatric populations, dermatological disease, and diabetes. [15- 21] Using a specialized didactics framework and practice-based learning via videoconferencing technology, Project ECHO allows front-line clinicians and healthcare workers in underserved areas to receive “tele-mentoring” from trained specialists in academic centers and thereby, gain confidence and support to manage complex chronic diseases. The method has not only been deemed cost-effective, but also sustainable, as it engages primary care provided in a learning system, where they can go on to serve as knowledgeable resources in their communities. Project ECHO is currently being adopted globally in efforts to dramatically increase access to specialty treatment in both rural and urban underserved regions. In this article we are the first to report on the use of the ECHO model for health care professional students or those in preclinical practice.
Methods
Building Partnerships
In September 2018, George Washington University launched the first ECHO project in the National Capital Area supported by the MERCK Bridging the Gap grant titled: Reducing Disparities in Diabetes Care with the La Clinica Del Pueblo’s (LCDP) Primary Care Providers. LCDP is a non-profit, federally qualified health center (FQHC) that primarily serves the Latino and immigrant populations of the Washington, DC region. This then expanded to multiple federally funded healthcare systems across the national capital area for a total of 3 cycles of ECHO with PAS participating in each cycle and further educational grants from Merck and Novo Nordisk with last cycle being completed at University of Washington given faculty movement but highlighting to ability to remotely give these programs.
Echo Sessions Development and Operation:
Using the Zoom telecommunication platform, specialists were able to engage with FQHC providers and PAS. The chronic disease targeted was diabetes. The core team of mentors included an endocrinologist and a diabetes educator, who led tele-mentoring sessions and case-based discussions on complex diabetes management. There were also rotating specialists from cardiology, mental health, podiatry, renal, ophthalmology that discussed prevalent diabetes-related complications with primary care providers. Over the course of 6 months and 14-16 total bi-monthly sessions, providers (n=65) (result reported elsewhere) and PA students (n=42) enhanced their diabetes knowledge and confidence in providing high quality care to underserved individuals with the disease
Structure of an ECHO Session:
Didactics: After participant attendance is noted, the endocrinologist or another specialist, gives brief lectures on a diabetes-related topic. Topics covered range from insulin initiation and management to diabetes and co-morbid depression, to individualizing HbA1C goals, to cultural sensitivity in the Latino community. Each topic held specific learning objectives that were delineated for participants before the sessions. Topics were selected by specialists and then reviewed by primary care clinic directors prior to finalizing the curriculum.
Case presentations: During each session, a de-identified, multi-disciplinary patient case relating to the week’s topic was discussed among PCPs and students with recommendations made for management by the specialists for cased based learning.
Evaluation
ECHO participants completed a survey before and after taking the course. The survey was designed to measure 1) self-assessed competency in providing high-quality diabetes care, 2) confidence in complex diabetes management, and 3) factual knowledge. For the 2nd and 3rd cycles, questions about current and anticipated prescribing practices were added. Survey items were developed following literature review of identifying quality care standards in diabetes management and evaluations used by previous diabetes ECHOs. 2, 21,22 Specific surveys included 20 measures of selfefficacy and confidence in individualized diabetes care, awareness of patients’ socio-contextual determinants of health, screening for diabetes-related (Table 1).
Table: 1Pre-post questionnaire for self-efficacy (14 questions), confidence in management (6 questions) and prescribing practices (11 questions). Questions for self-efficacy and confidence reported on a 5 and 7 point Likert scale respectively and prescribing practices reported on a 4- point Likert scale.
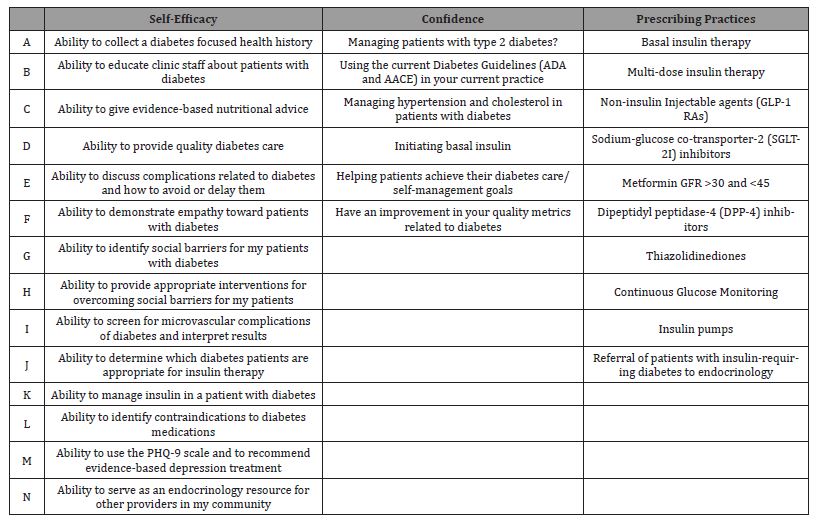
Complications, and knowledge of evidence-based medicine guidelines. Furthermore, there were 14 measures of factual accuracy with regards to complex diabetes management. All competency survey measures were reported on a 7-point Likert scale: not competent, vaguely competent, slightly competent, average amongst peers, competent, very competent, and teach others. Confidence survey measures were reported on a 7-point scale ranging from confident to absolutely confident. Factual survey item responses were question dependent as some involved checking all the right answers and others were basic multiple choice. Prescribing and referral practices for diabetes medications and technology were reported on a 4-point scale: always, sometimes, rarely, or never.
Statistical analysis
Introduction
For each student, we calculated the mean response (competency, confidence, prescribing) or the total number of correct answers (knowledge) for each domain and time period. We compared these summary scores as well as individual survey items between time periods using a one-sample (paired) Student’s t-test. In addition to the p value, we report the mean response or number of correct answers by time period and the difference between time periods.
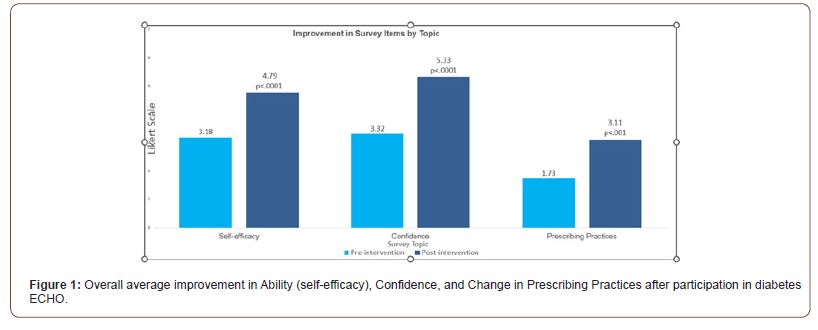
Results
Over 3 cycles of ECHO sessions from 2018-2021, we engaged 42 PA students. The average session participant attendance was 52% (range 0%-100%) for students. Twenty-three PAS completed at least 50% of sessions and eighteen of these completed pre and post evaluation, with average attendance of 76% (range 56%-100%). On a 7-point Likert scale, self-efficacy increased from 3.18 (slightly competent) pre-intervention to 4.79 (competent) post (p<.0001). Confidence increased from 3.32 (neutral) to 5.33 (somewhat confident) (p<.0001) (Figure 1).
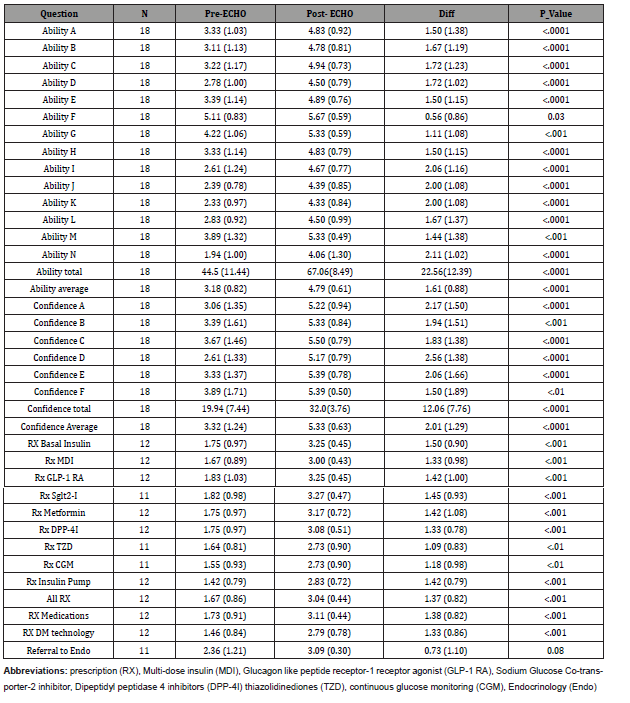
On factual knowledge questions, PAS were able to answer an average of 5.67 out of 12 correctly after the intervention, compared to 3.78 before (p<0.01). PAS’ belief in their competence to be an endocrinology resource in the community increased from 1.94 to 4.06 (p<.0001). Twelve students completed a pre-post questionnaire on current and anticipated prescribing practices (cycles 2 and 3). Average current referral to endocrine for management of insulinrequiring diabetes increased from 2.36 (rarely) to 3.09 (sometimes) (p=.08). Students’ anticipated frequency of prescribing diabetes medications increased from 1.73 (rarely) to 3.11 (sometimes) (p<.001). Specifically, anticipated prescribing practices for newer diabetes medications with cardiovascular and renal indications (GLP-1 receptor agonists and SGLT-2 inhibitors) increased from 1.79 to 3.25 (p<.001) while prescribing for basal insulin went from 1.75 to 3.25 (p<.001), and for multi-dose insulin from 1.67 to 3.00 (p <.001). Anticipated prescribing of diabetes technology (continuous glucose monitoring and insulin pumps) increased from 1.46 to 2.79 (p<.001). Full results are shown in (Table 2).
Table: 2Pre and Post Confidence, Ability and Perception of Prescribing Practices in Physician Assistant Students’ that participated in ECHO.
Discussion
In 2003 the ECHO model was first launched to support access for hepatitis c treatment[15]. It has now been adopted nationally and international as a tool to help combat diseases in multiple specialties including diabetes. There has been and are ongoing evaluations of these programs to shown provider and patient level benefit for use of this tool [22]. A unique feature of our study is its’ emphasis on incorporating “early learners” such as PA students into ECHO sessions. We strove to expand our audience beyond PCPs already in clinical practice and target participants in medical residencies, 4th year medical students and also PA and NP students given studies have shown that PAs and NPs are playing an increasingly prominent role in the primary care of medically complex patients. [23] However, despite the wide adoption of the ECHO model, to our knowledge our ECHO for diabetes is the first to evaluation it’s benefit for students and use it to increase knowledge prior to clinical practice. Our pilot data shows the PAS students increase their confidence and ability and knowledge to support patients living with diabetes. Additionally, medical and technology inertia in diabetes is high for example despite newer medication and technology for diabetes becoming available use remain low especially in those of lower social-economic means and in minority populations [24, 26]. Our data shows that ECHO may help those such as PA students who rapidly become part of the PCP workforce, especially in rural and underserved be more likely to prescribe these needed therapies for diabetes. Despite increase in confidence and knowledge, Students did report increased anticipation rather than decreased numbers of referrals to endocrine. This may be because this was one of their first true experiences with the complexity of diabetes management and also, they may have been better understanding of appropriate person to refer to a specialist after ECHO. However, we did not ask why they would increase their referrals, so this is speculation.
We also recognize the limitations of our current study. Notably, our sample size of PAS is low and can affect statistical significant. We also acknowledge the overall retention of students and mean attendance for the session also was lower than anticipated. Informal discussion/feedback from students about the lower attendance highlights students’ discomfort in asking preceptors during clinical rotations for “time off” from direct patient care in order to attend sessions. Given low attendance, there is ongoing evaluation of using recorded sessions or “on-demand” learning of ECHO sessions as part of the endocrine curriculum for a PA Program. There is also a need to follow students who participated in ECHO and evaluate their comfort and ability as compared to their peers once they are in clinical practice and evaluate if ECHO as part of their pre-clinical educational curriculum translated to improved patient outcomes.
In summary, our diabetes Project ECHO model is the first to evaluate value for healthcare professional students. PAS students did increase their confidence and ability to support patients living with diabetes and anticipated more use of diabetes mediations and technology after participation in the live ECHO session. Further research is needed to assess benefit once in clinical practice and also as an OnDemand/pre-recorded model to make it more accessible for student learning.
Funding/Support
We grateful acknowledge Merck foundation disparities of healthcare grant: “Bridging the Gap” and Merck and Novo Nordisk Educational grants as support for our ECHO program
Disclosures
Dr. Ehrhardt has been on an advisory board for Novo Nordisk and Dexcom and received investigator-initiated grants from Dexcom and Educational Grants from Novo Nordisk and Merck.
Ethical Approval
ECHO program was considered exempt from IRB given educational program. This program was reviewed by George Washington IRB for cycle 1-2(2018) and cycle 3 University of Washington (STUDY:00011372: Diabetes ECHO (10/16/2020). All data was kept secure in the REDCAP database. All pre-post surveys were conducted by Redcap. At the beginning of pre-post surveys participants could select “I do not wish to be included in research” if desired” and were excluded from analysis if box was checked.
Previous Presentations
These data from cycle one was present at the Annual Conference on the Science of Dissemination and Implementation in Health, co-hosted by the NIH and Academy Health Dec 2019 as a poster and then combined cycles at The American Diabetes Association national meeting in June 2022 as a virtual poster presentation.
Author Contributions
Nicole Ehrhardt, MD led the design of the study, reviewed the data analysis, drafted the manuscript and tables and figures, and completed all revisions and final review of the paper. Nicole Ehrhardt performed all duties of the primary author. Sanjana Rao contributed significantly to data analysis review and to the manuscript and completed all revisions and final review of the paper. Annette Aldous was the lead on the data analysis and significantly contributed to the manuscript and completed all revision and final review of paper.
Acknowledgement
Megan Phelps, University of Washington Medical student helped with initial poster presentation and figures
Conflict of Interest
No Conflict of interest.
References
- Edward W Gregg, Yanfeng Li, Jing Wang, Nilka Rios Burrows, Mohammed K Ali, et al. (2014) Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med 370(16): 1514-1523.
- Matthew F Bouchonville, Brant W Hager, Jessica B Kirk, Clifford R Qualls, Sanjeev Arora (2018) Endo Echo Improves Primary Care Provider and Community Health Worker Self-Efficacy in Complex Diabetes Management in Medically Underserved Communities. Endocr Pract 24(1): 40-46.
- (2022) The Burden of Diabetes by State.
- (2022) DOH DC health.
- Robert A Vigersky, Lisa Fish, Paul Hogan, Andrew Stewart, Stephanie Kutler, et al. (2014) The clinical endocrinology workforce: current status and future projections of supply and demand. J Clin Endocrinol Metab 99(9): 3112-3121.
- David I Auerbach, Douglas O Staiger, Peter I Buerhaus (2018) Growing ranks of advanced practice clinicians implications for the physician workforce. N Engl J Med 378(25): 2358-2360.
- Janice C Zgibor, Thomas J Songer, Sheryl F Kelsey, Allan L Drash, Trevor J Orchard (2002) Influence of health care providers on the development of diabetes complications. Diabetes Care 25(9): 1584-1590.
- Beatriz Hemo, Danit R Shahar, Dikla Geva, Anthony D Heymann (2018) Adherence to quality of care measurements among 58,182 patients with new onset diabetes and its association with mortality. PLoS One 13(12): e0208539.
- Kerry A McBrien, Christopher Naugler, Noah Ivers, Robert G Weaver, David Campbell, et al. (2017) Barriers to care in patients with diabetes and poor glycemic control-A cross-sectional survey. PLoS One 12(5): e0176135.
- Anne Scott, Duncan Chambers, Elizabeth Goyder, Alicia O Cathain (2017) Socioeconomic inequalities in mortality, morbidity and diabetes management for adults with type 1 diabetes: A systematic review. PLoS One 12(5): e0177210.
- David Beran, Margaret Ewen, Richard Laing (2016) Constraints and challenges in access to insulin: a global perspective. Lancet Diabet Endocrinol 4(3): 275-285.
- William Barbosa, Kina Zhou, Emma Waddell, Taylor Myers, E Ray Dorsey (2021) Improving Access to Care: Telemedicine Across Medical Domains. Annu Rev Public Health 42: 463-481.
- Ole W Rasmussen, F F Lauszus , M Loekke (2015) Telemedicine compared with standard care in type 2 diabetes mellitus: a randomized trial in an outpatient clinic. J Telemed Telecare 22(6): 363-368.
- Jennifer K Raymond, Cari L Berget, Kimberly A Driscoll, Kaitlin Ketchum, Cynthia Cain, et al. (2016) CoYoT1 Clinic: innovative telemedicine care model for young adults with type 1 diabetes. Diabetes Technol Ther 18(6): 385-390.
- Sanjeev Arora, Karla Thornton, Glen Murata, Paulina Deming, Summers Kalishman, et al. (2011) Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med 364(23): 2199-207.
- E Michael Lewiecki, Matthew F Bouchonville, David H Chafey, Arthur Bankhurst, Sanjeev Arora (2016) Bone Health ECHO: telementoring to improve osteoporosis care. Womens Health (Lond) 12(1): 79-81.
- Ruth E Dubin, John Flannery, Paul Taenzer, Andrew Smith, Karen Smith, et al. (2015) ECHO Ontario Chronic Pain & Opioid Stewardship: Providing Access and Building Capacity for Primary Care Providers in Underserviced, Rural, and Remote Communities. Stud Health Technol Inform 209: 15-22.
- Kristin Sohl, Micah O Mazurek, Rachel Brown (2017) ECHO Autism: Using Technology and Mentorship to Bridge Gaps, Increase Access to Care, and Bring Best Practice Autism Care to Primary Care. Clin Pediatr (Phila) 56(6): 509-551.
- Angela G Catic, Melissa L P Mattison, Innokentiy Bakaev, Marisa Morgan, Sara M Monti, et al. (2014) ECHO-AGE: an innovative model of geriatric care for long-term care residents with dementia and behavioral issues. J Am Med Dir Assoc 15(12): 938-942.
- Hal Lewis, Mirna Becevic, Danny Myers, Dyann Helming, Rachel Mutrux (2018) Dermatology ECHO-an innovative solution to address limited access to dermatology expertise. Rural Remote Health 18(1): 4415.
- Matthew F Bouchonville, Margaret M Paul, John Billings, Jessica B Kirk, Sanjeev Arora (2016) Taking Telemedicine to the Next Level in Diabetes Population Management: a Review of the Endo ECHO Model. Curr Diab Rep 16(10): 96.
- Carrol Zhou, Allison Crawford, Eva Serhal, Paul Kurdyak, Sanjeev Sockalingam (2016) The Impact of Project ECHO on Participant and Patient Outcomes: A Systematic Review. Acad Med 91(10):1439-1461.
- Perri A Morgan, Valerie A Smith, Theodore S Z Berkowitz, David Edelman, Courtney H Van Houtven, et al. (2019) Impact Of Physicians, Nurse Practitioners, And Physician Assistants On Utilization And Costs For Complex Patients. Health Aff (Millwood) 38(6): 1028-1036.
- Rozalina G McCoy, Holly K Van Houten, Yihong Deng, Pinar Karaca Mandic, Joseph S Ross, et al. (2019) Comparison of Diabetes Medications Used by Adults With Commercial Insurance vs Medicare Advantage, 2016 to 2019. JAMA Netw Open 4(2): e2035792.
- Lauren A Eberly, Lin Yang, Utibe R Essien, Nwamaka D Eneanya, Howard M Julien, et al. (2021) Racial, Ethnic, and Socioeconomic Inequities in Glucagon-Like Peptide-1 Receptor Agonist Use Among Patients With Diabetes in the US. JAMA Health Forum 2(12): e214182.
- Nicole C Foster, Roy W Beck, Kellee M Miller, Mark A Clements, Michael R Rickels, et al. (2019) State of Type 1 Diabetes Management and Outcomes from the T1D Exchange in 2016-2018. Diabetes Technol Ther 21(2): 66-72.
-
Nicole Ehrhardt*, Sanjana Rao and Annette Aldous. A Pilot Study of a Diabetes Project ECHO for Healthcare Trainees. Endo & Diab Opn Acc J. 1(1): 2022. EDOAJ.MS.ID.000503.
-
Homicides, Longitudinal diabetes care, Telemedicine, Co-morbid depression, Socio-contextual determinants, Diabetes complications, Chronic respiratory lower diseases, Myriad, Didactics, Insulin, Socio-contextual determinants of health
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.