 Research Article
Research Article
Working Culture of An Interprofessional Collaborative Care Model That Focuses on Military Families: Students’ Perspectives
Afua O. Arhin PhD, RN1, Sheila Cannon PhD, PMHCNS-BC, PMHNP-BC2, Gwen Lee Thomas PhD3, Stephanie Hodges DNP, FNP-C, CNEcl2* and Christy Swinson DNP, FNP-C, CMSRN2
1College of Health, Science, and Technology, Fayetteville State University, Fayetteville North Carolina, USA
2School of Nursing, Fayetteville State University, Fayetteville North Carolina, USA
3Quality Measures LLC, USA
Stephanie Hodges, School of Nursing, Fayetteville State University, Fayetteville North Carolina, USA.
Received Date: July 26, 2023; Published Date: August 01, 2023
Abstract
Innovative and collaborative practice models are surfacing across the country to strengthen interprofessional learning in an effort to improve quality patient outcomes, improve efficiency, and increase job satisfaction with health professionals. This study discusses student’s perspectives of participation in a unique interprofessional practice model that embodies psychosocial health of military families. The Collaborative Institute for Interprofessional Education and Practice (CI-PEP) was established at a university in southeastern North Carolina, and is staffed by faculty members, community members and healthcare students.
Students completed a pre and post survey using the Mayo High Performance Teamwork Scale (MHPTS) which posed questions about team leadership, understanding of roles, openness to asking for help, collaboration, decision sharing, and patient care through collaborative approaches. Survey findings concluded that team building interventions helped the team focus on client centeredness, respect for differences and elucidated the importance of early interprofessional role socialization for collaborative practice to be successful.
Introduction
Military Health
The stress of war and its impact on service members, veterans and their families are well documented. According to the American Psychiatric Association, preliminary data from the Veteran’s Administration showed that the suicide rate for 18-29-year-old male veterans rose 26% from 2015 to 2020 and the rate climbed to record high by 2021. Further, of the 1.7 million veterans who served in Iraq and Afghanistan, 20% suffer from post- traumatic stress disorder (PTSD) or major depression [1]. Recent studies have extensively documented chronic pain as a common co-morbidity to post-traumatic stress disorder and other mental health conditions prevalent in veterans [2].
Further, military families face unique stressors associated with deployment and reintegration. For example, veteran status has been associated with three times the rate of intimate partner violence than among civilians [3]. Therefore, it is clear that in promoting the biopsychosocial health of military families, a comprehensive approach, using interprofessional collaboration is essential. In this report, interprofessional collaboration of nursing psychology, social work and complementary and alternative medicine is a novel and effective approach in meeting the varied needs of this important sector of the population.
Interprofessional Collaboration
Innovative and collaborative practice models are surfacing across the country to strengthen interprofessional learning. Josiah Macy Foundation [4] supports the benefit of these models to interdisciplinary team learning to improve quality patient outcomes. The overriding need for interprofessional education and practice concept is the notion that teams accomplish more together than they do separately. There is also evidence that patient satisfaction and patient safety improves which gains effective and efficient cost savings [5] Yet teamwork training for interprofessional collaborative practice in health professional education has lagged dramatically behind the changes in practice [5]. This lag probably lies in the fact that moving towards interprofessional practice requires a fundamental shift in health professional’s attitudes towards such an approach as well as a change in existing socializations and workplace organizational structure [6]. Despite these challenges, an interprofessional practice was established to meet the needs of military families.
Setting
The Collaborative Institute of Education and Practice (CIPEP) is a Health Resources and Services Administration (HRSA) partly funded collaborative institute spearheaded and housed in the Department of Nursing of a state university located in the southeastern corner of North Carolina. The 2 day a week institute offers holistic services including complementary and alternative medicine to 750 military family clients. The institute is staffed by six faculty members from nursing, social work and psychology, two community members who offer complementary and alternative medicine, seven core clinical students from nursing, psychology and social work; as well as a number of students who rotate through the clinic for clinical or internship hours.
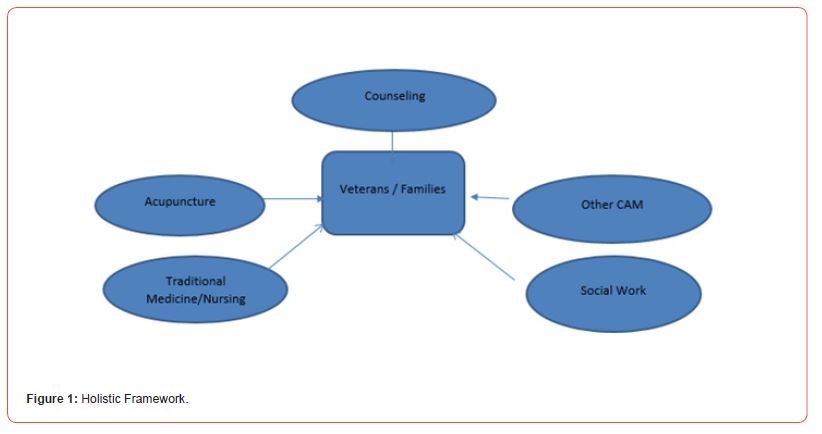
Holistic Theoretical Framework
To meet the needs of military families, a holistic theoretical framework is used to guide this interprofessional collaborative practice and is schematically represented in Figure 1. Families with reintegration problems as well as clients with post-traumatic stress disorder, and/or chronic pain typically seek care at the practice. Consequently acupuncture, individual and group counseling, as well as massage therapy are the most common collaborative treatment modalities in this practice [7].
Demographics of Participants
Four of the seven core clinical students are graduate students from psychology; two are undergraduate nursing students and one an undergraduate social work student. All students worked between eight and sixteen hours each week and all received stipends for their work in the practice. Four of the students identify themselves as white, two identify themselves as black and one as Asian. Five of the students are between the ages of 20 and 25, one is between 25 and 30 and one older than 30. This paper focuses on survey results for the seven core clinical students.
Methodology
CI-PEP was established as an interprofessional collaborative clinical site for undergraduate and graduate students majoring in nursing, social work, and psychology. As part of the evaluation of the site for students as inter-professional collaborators, survey instruments, specifically the Mayo High Performance Teamwork Scale (MHPTS) was administered to the seven core clinical students in the fall semester, six months after the practice was open, after receiving Institutional Board approval from the university.
In addition to the data-gathering, the faculty and students who worked in the practice in collaborative teams participated in a team building workshop led by an external consultant. The sessions included characteristics of an effective team, barriers/ challenges to performing as an effective team, and a case study to apply the information covered in the workshop. The MHPTS was administered again in the following spring semester, six months after the intervention. Paper copies of the MHPTS were administered to the students. The students were instructed to respond to the Scale based on their experiences as a collaborative team in the Institute. The responses were manually entered into an excel spreadsheet and frequencies were calculated.
MHPTS is a 16-item survey that poses questions about team leadership, understanding roles, openness to asking for help, collaboration, decision sharing, and patient care through collaborative approaches. The scale has been validated extensively in the literature for its reliability and validity. For example, in a study to develop and evaluate a participant rating scale for assessing high performance teamwork skills in simulation medicine settings Malec et al. (2007 ) [7] found that MHPTS showed satisfactory internal consistency and construct validity by Rasch (person reliability = 0.77; person separation = 1.85; item reliability = 0.96; item separation = 5.04) and traditional psychometric (Cronbach’s alpha = 0.85) indicators [8].
The purpose of this paper is to present the results of MHPTS
that was administered to students who participated in an
interprofessional practice pre and post a team building intervention./p>
Results
The results of the MHPTS Scale before and after the team building workshop are presented in Table 1.
Table 1: Mayo High Performance Team Scale.

When reviewing the clinical students’ pre and post responses on the Mayo High Performance Teamwork Scale, there were some slight improvements after the intervention. For example, 57% of the clinical students indicated during the fall semester that “each team member demonstrates a clear understanding of his/her role” and during spring semester, 80% of the students indicated that this occurred consistently. In addition, there was also a 23% improvement in the number of clinical students who indicated that “team members refer to established protocols and checklists for the procedure/intervention” on a consistent basis and a 29% improvement with regard to “team members call attention to actions that they feel could cause errors or complications.” Finally, there appeared to be a 20% decrease in the consistency of “disagreements or conflicts among team members are addressed without a loss of situation awareness” on a consistent basis.
Discussion
The survey results mirrored anecdotal information available to the team. During the first few months of CI-PEP practice, team leaders still appeared to be uncomfortable with other members from other disciplines, were still learning their roles and at times would revert back to working in silos, like they were used to in their traditional practice. “Silo-working” characteristics exhibited included not communicating as often to other team members regarding a client and not calling attention to actions of others that could cause complications. Another challenge faced by the interprofessional team in the early months was full understanding of how complementary and alternative medicine functioned. Because other disciplines in the practice are used to working with very concrete protocols, it took the team a while to understand, the approach and practice style of acupuncture. This misunderstanding led to some team dissension, affecting collaborative practice which was reflected in the early survey results. The team building intervention helped the team to focus on client centeredness, respect for differences and elucidated the importance of early inter professional role socialization for collaborative practice to be successful.
Conclusion
In collaborative practice, health professionals must learn to accept each profession with its own unique culture and learn to trust other professions of the team to have the same goals for client outcomes. Successful interprofessional collaborative practice is built on respect, trust and understanding of the unique and complementary perspectives of each profession while valuing the client’s views. The student perspective gathered from the MHPTS as well as anecdotes was important in assessing how well the team functioned interprofessionally and was instrumental in guiding the team building intervention. Role socialization was identified as the most salient theme that mitigated interprofessional collaboration in the first few months of practice.
Implications for Practice
The findings of this study support the growing evidence that, in spite of challenges, this model of interprofessional collaborative practice offers distinct advantages. This collaborative practice model not only provides community support services for military members and their families but offers an opportunity to evaluate the efficacy and challenges of interprofessional teams that have the capacity to inform and advance health systems. The use of an interprofessional collaborative model in healthcare programs of study allows students to benefit from this collaboration and gain an interprofessional perspective early in their healthcare careers.
Ongoing research and evaluation of interprofessional collaboration is needed to further enhance collaboration across disciplines as healthcare professionals understand their role as both individual and team member, while working together to improve patient outcomes.
Conflict of Interest
None.
Acknowledgment
None.
References
- American Psychiatric Association (APA) (2022) The critical need for health professionals trained to treat post- traumatic stress disorder and traumatic brain injury. Arlington, VA: American Psychiatric Association.
- Eun Jin Lee, Susan K Frazier (2011) The efficacy of acupressure for symptom management: A systematic review. Journal of Pain & Symptom Management 42(4): 589-603.
- Ruth Paris, Ellen R DeVoe, Abigail M Ross, Michelle L Acker (2010) When a parent goes to war: effects of parental deployment on very young children and implications for intervention. [Research Support, U.S. Gov't, Non-P.H.S.]. Am J Orthopsychiatry 80(4): 610-618.
- Josiah Macy Jr (2012) Foundation 2012 Annual Report: Accelerating Interprofessional Education.
- Canadian Interprofessional Health Collaborative (2010) A national interprofessional competency framework.
- Blue A Zoller J, Stratton Elam C, Gilbert J (2010) Interprofessional education in US medical schools. Journal of Interprofessional Care 24: 204-206.
- Arhin A, Gallop K, Mann J, Cannon S, Tran K, et al. (2015) Acupuncture as a Treatment Option in Treating Posttraumatic Stress Disorder-Related Tinnitus in War Veterans: A Case Presentation. J Holist Nurs 34(1): 56-63.
- James F Malec, Laurence C Torsher, William F Dunn, Douglas A Wiegmann, Jacqueline J Arnold, et al. (2007) The mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills. Simul HealthCare 2(1): 4-10.
-
Afua O. Arhin PhD, RN, Sheila Cannon PhD, PMHCNS-BC, PMHNP-BC, Gwen Lee Thomas PhD, Stephanie Hodges DNP, FNP-C, CNEcl* and Christy Swinson DNP, FNP-C, CMSRN. Working Culture of An Interprofessional Collaborative Care Model That Focuses on Military Families: Students’ Perspectives. Curr Tr Clin & Med Sci. 3(4): 2023. CTCMS.MS.ID.000569.
-
Health, Post- traumatic stress disorder (PTSD), depression, nursing psychology, education
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






