 Mini Review
Mini Review
What Does Shortness of Breath Mean in Acute Pneumonia?
Igor Klepikov, Pediatric surgeon, Washington, USA.
Received Date: May 06, 2023 Published Date: June 24, 2023
Introduction
One of the most characteristic and relatively early signs of acute pneumonia (AP) is shortness of breath. The appearance of this sign in patients with AP is usually identified with respiratory insufficiency and may be accompanied by hypoxemia [1-3], which, in turn, serves as a marker of the severity of the disease and a prognostic indicator [4-7]. One of the main reasons for the rapid respiratory rhythm and the feeling of lack of air is considered to be the blockade of gas exchange in the area of inflammatory infiltration and blood bypass through unventilated areas [8-11]. If part of the inhaled air cannot reach the level of gas exchange membranes and maintain adequate oxygen saturation of the blood, then logically it is necessary to increase its concentration in the lung ventilation system. Such a conclusion currently determines the direction of early care for such patients, once again confirming the basic rule that the solution to any problem is determined by understanding its essence.
Existing ideas about the mechanism of respiratory disorders in patients with AP logically put forward the supply of oxygen as first aid, which has now reached the level of therapeutic instinct. The immediate provision of oxygen inhalations to patients is facilitated by the fact that such therapy does not require an official prescription and order of medicines [12]. For example, in the UK, according to expert estimates, 34% of patient trips in an ambulance are associated with oxygen supply [13]. The hope for the effect of oxygen therapy increased especially significantly during the SARS-CoV-2 pandemic, when long-term confidence in the effect of antibiotics in patients with COVID-19 pneumonia disappeared. This was noted not only by a noticeable revival of the discussion regarding the diagnosis of the level of respiratory disorders and various options for providing patients with oxygen, including artificial ventilation, but also by the introduction of these methods into the category of strategic decisions [14-27].
Strengthening of oxygen and ventilation support for patients with AP does not have a noticeable effect on the results of treatment of this contingent, and methods of such assistance are fairly classified as auxiliary [20]. Despite its secondary role and a very dubious effect on the overall result, methods of correction of gas exchange and lung ventilation attract a lot of attention in the treatment of patients with AP. For example, a number of specialists concentrate their efforts on careful monitoring of such patients in order to carry out intubation in a timely manner and transfer to artificial ventilation of the lungs, if such a need arises [28-30]. Evidence of the palliative nature of such efforts is highlighted by the statistics of final results, which indicate a sharp increase in mortality among intubated patients with AP [31,32]. And although, as noted above, many authors consider hypoxemia as a prognostic criterion for the severity of pneumonia, however, a more detailed analysis shows that the overall results of treatment of these patients and the mortality rate do not depend on the level of oxygen saturation in the blood and the success of its correction [24,27,33].
Interpretations of lung ventilation disorders, common today in patients with AP, can acquire a completely different edition if you pay attention and analyze well-known evidence and facts that are not given the necessary importance in this disease. Although today it is claimed that almost 500 causes contributing to the appearance of shortness of breath have been identified, its main triggers are still disorders in the cardiovascular and respiratory systems [34]. At the same time, the following conditions were and remain fundamentally important for understanding the chronology of current deviations and choosing adequate medical care.
First of all, the lungs and the heart are so inextricably linked with each other that changes in the function of one organ necessarily cause reciprocal shifts in the function of the other, and the main functional purpose of each of these organs can be fully realized only in interaction [35-39]. Isolated performance of its function by both the lung tissue and the cardiovascular system is impossible to imagine even theoretically, since the main joint function of these two systems - the gas exchange chain - can be realized only with their mutual work.
Secondly, in order to provide targeted pathogenetic care, it is very important to have an accurate understanding of the causes of emerging lung ventilation disorders. It is well known that pathologies incomparable in their pathogenesis, such as myocardial infarction or pneumothorax, are also accompanied by shortness of breath, but no one hopes to help the patient in such situations only by supplying oxygen, although it is usually used in such cases. At the same time, modern interpretations of respiratory disorders in patients with AP do not explain why some patients may not have obvious shortness of breath at all, and those who have signs of respiratory disorders do not always develop hypoxemia. In addition, these differences do not demonstrate a direct dependence on the volume of inflammatory transformation of lung tissue.
Finally, normal gas exchange requires not only a sufficient supply of oxygen to the alveoli of the lungs, but also the equivalent removal of carbon dioxide. At the same time, as is known, both the delivery of oxygen and the removal of carbon dioxide occur along the same route, but only in different directions. Therefore, if it is assumed that the blockade of part of the alveoli by the inflammatory process leads to hypoxemia, then hypercapnia should be observed with the same frequency. However, excess carbon dioxide in the blood usually occurs in the late stages of the disease and serves as one of the markers for transferring patients to auxiliary ventilation. Up to this point, patients do not receive any support in removing carbon dioxide, but, regardless of the level of oxygen in the blood, they are usually provided with insufflation of the latter. With this approach to oxygen therapy, the question inevitably arises about the side effects of such widespread use of oxygen.
The answer to this question follows from the already known information that not only the lack of oxygen, but also its excess are undesirable for the vital activity of the body [40,41]. Excessive oxygenation can reduce respiratory activity and contribute to further accumulation of carbon dioxide, if such a trend has already been noted [42]. Therefore, in patients at risk of carbon dioxide retention, lower oxygenation rates (88-92%) are considered preferable, and it is not recommended to start oxygen therapy when the blood is saturated to 90-93% (42-45). Taking into account the risks associated with the arbitrary use of oxygen therapy, the British Thoracic Society has in recent years pursued a policy of recognizing oxygen as a drug with the appropriate formulation and documentation [46].
The increased interest in oxygen therapy, which has been observed for many years in the treatment of patients with AP, is explained by the fact that this method is very simple, easily accessible and in fact the only one that is used when a patient with shortness of breath needs help. The first part of the medical duty is considered fulfilled if the patient is provided with oxygen insufflation and a pulse oximeter is installed, but, as further observation shows, this action does not lead to a noticeable normalization of breathing, even if blood oxygen saturation reaches a satisfactory level. The lack of proper effect from such therapy indicates that it does not affect the causes that cause a change in the respiratory rhythm. As the results of our studies conducted more than 30 years ago have shown, the cause, in particular, of shortness of breath in patients with AP is not a violation of diffusion at the level of inflamed unventilated segments of the lungs, but a completely different mechanism.
The reason for conducting the study in question was the prevailing circumstances. At that time, patients with abdominal pain syndrome AP were often admitted to the surgical department (where the author of these lines worked). In the former Soviet Union, where this part of the work was carried out, a directive was adopted on the conduct of cervical novocaine vagosympathetic blockade (CVSB) in such cases for differential diagnosis with surgical pathology of the abdominal organs. If the patient suffered from abdominal AP syndrome, then a few minutes after the blockade (the appearance of Claude Bernard-Horner syndrome), the pain not only disappeared, but the condition of the patients improved markedly. Focusing on this general effect of this procedure, comparative rheopulmonograms (CRPG) were recorded in 22 patients with AP at the time of hospitalization. Detailed information about such manipulations and studies cannot be presented in a journal article, but these data have been published and, if necessary, are quite achievable [47].
The initial parameters of the rheopulmonograms indicated the predominance of ventilation over blood flow with a corresponding shift in their ratio coefficient. The results of CRPG after CVSB showed a decrease in the frequency and a slight increase in the depth of respiratory excursions with a parallel decrease in the number of heartbeats and a decrease in the amplitude of the systolic wave. In general, there was an alignment of the ratio between lung ventilation and blood flow. Such a noticeable effect, which was recorded literally within a few minutes after the remote vegetative blockade, as well as the nature of the observed normalization of indicators, can leave no doubt that the mechanism of disturbances in the work of the cardiopulmonary apparatus in patients with AP is reflex spasm of the vessels of the small circulatory circle. This reaction is protective in nature, aimed at reducing blood flow to the area of increasing edema and infiltration. With the rapid development of the inflammatory process, such a reaction becomes progressive and uncoordinated. This mechanism makes it difficult to pump blood through the lungs, reduces blood flow in a small circle and hinders adequate gas exchange. The body tries to compensate for the resulting complex of disorders by increasing the frequency of respiratory excursions and strengthening the work of the heart. An increase in the concentration of oxygen in the respiratory tract in this situation cannot, even theoretically, eliminate the described mechanism of disorders in AP.
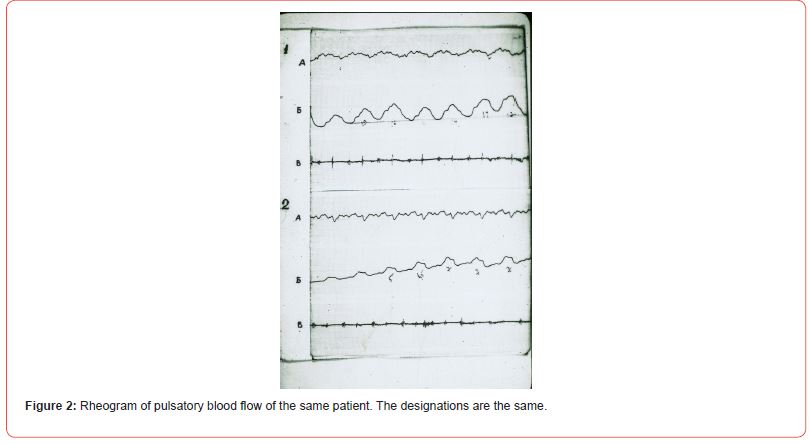
In this regard, it should be noted that a similar result was obtained after a session of cupping therapy (CPT), the use of which was not recommended, but was not officially prohibited. CRPG recordings were performed in 14 more patients with AP at the time of hospitalization. There were no patients with pain syndrome in this group, and the procedure itself was significantly different from performing CVSB. However, the analysis of the results showed that after CPT, a normalizing shift in rheopulmonography indicators was observed, which was identical to the changes observed after CVSB [47]. The identical effect of CPT is probably due to both reflex effects from peripheral receptors and unloading of pulmonary vessels due to accelerated deposition of part of the circulating blood in the surface tissues. As an illustrative example of changes in the rheogram of the lungs in patients with AP, the following are records of CRPG in one of the observations after performing CVSB (Figures 1 and 2).

To a brief description of the experience of using two techniques that help, in particular, improve lung ventilation, it should be added that this assessment of their action was based on objective indicators of lung respiratory function and blood flow in their vessels. This is a fundamentally different approach to the certification of the treatment methods used, which is why it differs significantly from the generally accepted assessment of oxygen therapy. The latter, as is known, is based on subjective feelings and maintaining the oxygenation index at a level characteristic of healthy (!) people. It is not by chance that experts began to come to the conclusion that high oxygenation in patients with AP [42-45] is inappropriate, indirectly confirming the old postulate about the so-called “norm in pathology”, when shifts of the body constants to certain limits are a reflection of compensation, and not serious violations.
In the process of work, the third method of emergency care for patients after the diagnosis of AP was also used, which consisted in short-term general cooling of the body and limbs of patients using cold wraps or baths. The influence of this method on the basis of subjective assessment and general indicators of the main functional constants turned out to be more effective compared to CVSB and CPT, but, unfortunately, we were unable to obtain objective data in such situations.
Recently, additional objective data have appeared confirming the important pathogenetic role of generalized blood flow disorders in the small circle of blood circulation in patients with acute inflammation of the lung tissue. Several specialists drew attention to the discrepancy between the amount of damage to the lung tissue and the occurrence of hypoxemia. To find out the reason for this discrepancy, an analysis of computed tomography data of the lungs in such patients was used. The data obtained showed a decrease in blood volume in small (less than 2 mm in diameter) vessels of a small circle, which the authors consider as a result of generalized spasm and thrombosis [48,49]. Widespread thrombosis of this segment of the vascular system of the body is unlikely to be compatible with the patient’s life, however, the spasm of these vessels confirms our results and conclusions presented above.
Thus, at present there is objective information indicating a completely different mechanism of dyspnea in patients with AP and explaining the low effectiveness of existing treatment approaches. This implies a fundamental revision of the pathogenesis of the disease and the priorities of medical care. Mandatory oxygen supply is not required for all patients with AP and should be determined by the dynamics of oxygenation. Currently, the basis of modern care for patients with AP during hospitalization is the urgent provision of oxygen insufflation and the choice of etiotropic drugs. Oxygen supply often has the character of a mandatory routine measure and proceeds against the background of waiting (especially in the first 48-72 hours) for the results of the action of etiotropic agents, which are mainly represented by antibiotics. During the period when the effect of etiotropic therapy is evaluated, not every organism is able to independently eliminate the circulatory disorders that have arisen, which can progress further, deepening the overall complex of disorders. With this approach to the principles of AP treatment, there is inevitably a need for timely identification of those situations when the patient needs intubation and transfer to auxiliary ventilation [28-32].
A critical analysis of the mechanisms of dyspnea shows that the initial cause of its development in AP is not the first two links in the gas exchange chain, which are considered to be lung ventilation and gas diffusion in the alveoli, but a generalized change in pulmonary blood flow. Reflex spasm of the pulmonary vessels disrupts blood flow in the lungs, reduces the volume of blood passing through healthy areas of the lungs, and helps to reduce blood oxygen saturation. Insufficient capacity of the small circulatory circle forces the body to enhance the massaging effect of ventilation and divert part of the circulating blood to facilitate the work of the lungs. The subsequent decrease in total blood flow affects the delivery of oxygen to the tissues of the body, and persistent violation of pulmonary circulation has a detrimental effect on the factors of stabilization of lung tissue, including surfactant, which ultimately provokes the development of respiratory distress syndrome [47]. In general, the presence of dyspnea in a patient with AP is an early sign of the emerging cascade of circulatory disorders and is secondary in nature. Its correction by oxygen supply and auxiliary ventilation of the lungs is not able to eliminate them, which is clearly demonstrated by the current results of treatment of this category of patients.
Conflict of interest
The author states that he has no conflict of interest.
Funding
This manuscript is a full initiative of the author and does not have any funding.
Acknowledgements
None.
References
- Ewig S, Ruiz M, Mensa J, Marcos MA, Martinez JA, et al. (1998) Severe community-acquired pneumonia. Am J Respir Crit Care Med 158: 1102-1108.
- Burki NK, Lee LY (2010) Mechanisms of dyspnea. Chest 138: 1196-1201.
- Parshall MB, Schwartzstein RM, Adams L, Banzett RB, Manning HL, et al. (2012) An official American thoracic society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 185: 435-452.
- Sumit R Majumdar, Dean T Eurich, John-Michael Gamble, A Senthilselvan, Thomas J Marrie (2011) Oxygen Saturations Less than 92% Are Associated with Major Adverse Events in Outpatients with Pneumonia: A Population-Based Cohort Study. Clinical Infectious Diseases 52 (3): 325-331.
- Fu L, Wang B, Yuan T, Chen X, Ao Y, Thomas F, et al. (2020) Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect 80: 656-665.
- Xie J, Covassin N, Fan Z, Singh P, Gao W, et al. (2020) Association between hypoxemia and mortality in patients with COVID-19. Mayo Clin Proc 95: 1138-1147.
- Ahmed Ehsanur Rahman, Anika Tasnim Hossain, Harish Nair, Mohammod Jobayer Chisti, David Dockrell, et al. (2022) Prevalence of hypoxaemia in children with pneumonia in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Global Health 10(3): E348-E359.
- Rider AC, Frazee BW (2018) Community-Acquired Pneumonia. Emerg Med Clin North Am 36(4): 665-683.
- Pfeifer M, Hamer OW (2020) COVID-19-Pneumonie [COVID-19 pneumonia]. Internist (Berl) 61(8): 793-803.
- Respiratory failure.
- Hepokoski M L, Odish M, Malhotra A (2018) Prone positioning in acute respiratory distress syndrome: why aren't we using it more?. Journal of thoracic disease 10(Suppl 9): S1020-S1024.
- O'Driscoll BR, Howard LS, V Mak, Earis J, on behalf of the BTS Emergency Oxygen Guideline Development Group, et al. (2017) British Thoracic Society Guideline for oxygen use in adults in health care and emergency settings. BMJ Open Respiratory Research 4: e000170.
- Hale KE, Gavin C, O'Driscoll BR (2008) Audit of oxygen use in emergency ambulances and in a hospital emergency department. Emerg Med J 25: 773-776.
- Salluh JIF, Ramos F, Chiche JD (2020) Delivering evidence-based critical care for mechanically ventilated patients with COVID-19. Lancet Respir Med 8(8): 756-758.
- Truog RD, Mitchell C, Daley GQ (2020) The toughest triage — allocating ventilators in a pandemic. N Engl J Med 382: 1973-1975.
- M L Ranney, V Griffeth, A K Jha (2020) Critical Supply Shortages — The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. N Engl J Med 382: e41.
- Johns Hopkins Center for Health Security (2020) Ventilator stockpiling and availability in the US.
- V E Schaye, J A Reich, B P Bosworth, id T. Stern, Frank Volpicelli, et al. (2020) Collaborating Across Private, Public, Community, and Federal Hospital Systems: Lessons Learned from the Covid-19 Pandemic Response in NYC. NEJM Catalyst Innovations in Care Delivery:1(6).
- Gafford, Galloway K, Webster S, Emerson M, Riojas K, et al. (2021) The Vanderbilt Open-Source Ventilator: From Napkin Sketch to Ready to Save Lives in Three Weeks. IEEE Robotics & Automation Magazine 28(1): 101-114.
- Attaway AH, Scheraga R G, Bhimraj A, Biehl M, HatipoÄŸlu U (2021) Severe covid-19 pneumonia: pathogenesis and clinical management 372: n436.
- Roca O, Coral B, Messika J, Samper M, Sztrymf B, et al. (2019) An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med 199: 1368-1376.
- Alison E Thompson, Benjamin L Ranard, Ying Wei, Sanja Jelic (2020) Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med 180(11): 1537-1539.
- D L Fink, NR Goldman, J Cai, K H El-Shakankery, G E. Sisley, et al. (2021) Ratio of Oxygen Saturation Index to Guide Management of COVID-19 Pneumonia. Annals of the American Thoracic Society 18 (8): 1426-1428.
- Shang X, Wang Y (2021) Comparison of outcomes of high-flow nasal cannula and noninvasive positive-pressure ventilation in patients with hypoxemia and various APACHE II scores after extubation. Ther Adv Respir Dis: 17534666211004235.
- Tan W, Xu DY, Xu MJ, Wang ZF, Said, et al. (2021) The efficacy and tolerance of prone positioning in non-intubation patients with acute hypoxemic respiratory failure and ARDS: a meta-analysis. Ther Adv Respir Dis: 17534666211009407.
- Tan W, Xu DY, Xu MJ, Wang ZF, Said, et al. (2021) The efficacy and tolerance of prone positioning in non-intubation patients with acute hypoxemic respiratory failure and ARDS: a meta-analysis. Ther Adv Respir Dis: 17534666211009407.
- Maheen Sheikh, Huzaifa Ahmad, Romesa Ibrahim, Imran Nisar, Fyezah Jehan (2023) Pulse oximetry: why oxygen saturation is still not a part of standard pediatric guidelines in low-and-middle-income countries (LMICs). Pneumonia 15(1): 3.
- Rollas K, Ersan G, Zincircioglu (2021) Septic shock in patients admitted to intensive care unit with COVID-19 pneumonia. Eurasian J Pulmonol 23: 95-100.
- D A Berlin, R M Gulick, F J Martinez (2020) Severe Covid-19. N Engl J Med 383: 2451-2460.
- Gattinoni L, Gattarello S, Steinberg I, Mattia Busana, Paola Palermo, et al. (2021) COVID-19 pneumonia: pathophysiology and management. Eur Respir Rev 30: 210138.
- Merad M, Martin J C (2020) Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol 20: 355-362.
- Singh AP, Shady A, Gbaje E (2021) Factors associated with survival in patients with COVID -19 admitted to a community hospital in New York City. J Lung Pulm Respir Res 8(2): 27-33.
- Olav L Schjørring, Thomas L Klitgaard, Anders Perner, Jørn Wetterslev, Theis Lange, et al. (2021) Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. N Engl J Med 384: 1301-1311.
- Shortness of breath.
- Voelkel, Norbert F, Quaife, Robert A, Leinwand, et al. (2006-10-24) Right Ventricular Function and Failure Report of a National Heart, Lung, and Blood Institute Working Group on Cellular and Molecular Mechanisms of Right Heart Failure. Circulation 114 (17): 1883-1891.
- Nixon J V (2010) The AHA Clinical Cardiac Consult. Lippincott Williams & Wilkins 136: 9781608316229.
- Cor Pulmonale (2015) Pulmonary heart disease information. Patient | Patient.
- Cor pulmonale (2015) MedlinePlus Medical Encyclopedia.
- Pulmonary heart disease.
- Martin L (1997) Scuba Diving Explained: Questions and Answers on Physiology and Medical Aspects of Scuba Diving. Lawrence Martin: 9780941332569.
- World Health Organization (2009) Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization 20: 9789241547659.
- Domino KB (2019) Pre-emergence Oxygenation and Postoperative Atelectasis. Anesthesiology 131 (4): 771-773.
- (2015) British national formulary: BNF 69 (69 ed.). British Medical Association.
- Chu DK, Kim LH, Young PJ, Zamiri N, Almenawer SA, et al. (April 2018) Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 391 (10131): 1693-1705.
- Siemieniuk RA, Chu DK, Kit LH, Güell-Rus MR, Alhazzani W, et al. (2018) Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ 363: k4169.
- Hoda Ranjbar, Shruti Dorai (2021) Improvements and Shortcomings in Emergency Oxygen Prescribing: A Quality Improvement Initiative at an Acute Tertiary Care Hospital. EMJ.
- Klepikov (2022) The Didactics of Acute Lung Inflammation. Cambridge Scholars Publishing: 320.
- Muhunthan Thillai, Chinmay Patvardhan, Emilia M Swietlik, Tom McLellan, Jan De Backer, et al. (2021) Functional respiratory imaging identifies redistribution of pulmonary blood flow in patients with COVID-19. Thorax 76: 182-184.
- W Dierckx, W De Backer, M Links, Y De Meyer, K Ides et al. (2022) CT-derived measurements of pulmonary blood volume in small vessels and the need for supplemental oxygen in COVID-19 patients. Journal of Applied Physiology 133(6): 1295-1299.
-
Igor Klepikov*. What Does Shortness of Breath Mean in Acute Pneumonia?. Curr Tr Clin & Med Sci. 3(4): 2023. CTCMS. MS.ID.000567.
-
shortness of breath, acute pneumonia, hypoxemia, COVID-19, carbon dioxide, thrombosis, lungs, inflammation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






