 Research Article
Research Article
Prognostic Impact of Solid And Cystic Intracranial Metastases on Survival in Patients With Lung Cancer: A Retrospective Analysis
Eda Erdıs* and Birsen Yucel
Department of Radiation Oncology, Medical School of Cumhuriyet University, Turkey
Eda Erdıs, Department of Radiation Oncology, Medical School of Cumhuriyet University, Turkey.
Received Date: July 14, 2023 Published Date: July 25, 2023
Abstract
Objective: Brain metastases are the most common intracranial tumors in adults. Lung cancer is the most common tumor that metastasizes to the brain. In our study, the effect of metastasis nature on survival was investigated in patients diagnosed with lung cancer and developed brain metastases.
Method: In this study, the data of 271 patients who applied to Cumhuriyet University Radiation Oncology Center between 2007 and 2018 and were diagnosed with brain metastasis were retrospectively analyzed. Survival analysis was determined by Kaplan Meier Analysis and for independent prognostic factors by Cox Regression Analysis.
Results: 271 patients with lung cancer and brain metastasis were included in the study. At the time of diagnosis, 163 (60%) of the patients were in the metastatic stage. There was no difference between the groups in terms of age, RPA, KPS, histopathological subtype and treatment type (p>0.05). However, since there were fewer metastatic lesions in patients with cystic nature, a statistically significant difference was found between the groups in terms of the number of lesions (p<0.05). The median survival of patients after metastasis is 6 months, 1-year survival 43% in patients with cystic metastasis, and 3 months and 1-year survival in solid nature patients is 21%. In univariate analysis, RPA(p<0.001), histological subtypes (p=0.009), age (p=0.019), number of lesions (p=0.001), total crainal RT+SRS (p<0.001), metastatectomy (p=0.001) statistically significant. According to multivariate analysis, age >50, RPA I-III, number of lesions >3 and total cranial RT alone adversely affected the survival of the patients. The cystic type of metastasis improved survival (HR: 0.68, 95% CI: p=0.005).
Conclusion: In patients who developed brain metastasis due to lung cancer, the nature of the metastasis was cystic, positively affecting survival.
Keywords: Lung cancer; Brain Metastasis; Prognostic Factors; Survival; Solid; Cystic
Introduction
Brain metastases are one of the most important causes of morbidity and mortality in cancers with systemic spread. They are the most common intracranial tumors in adults [1]. Lung cancer is the most common tumor that metastasizes to the brain [2]. Therefore, understanding the impact of metastasis on survival outcomes and effective management strategies in lung cancer patients who develop brain metastases are crucial. Intracranial metastasis, the spread of cancer cells from a primary lung tumor to the brain, is a common and challenging complication in patients with lung cancer. The presence of intracranial metastatic components can have a significant impact on patient prognosis and survival. Understanding the survival impact of intracranial metastases is very important to guide treatment decisions and improve patient outcomes [3-7]. The aim of this study is to investigate the effect of metastasis nature on survival in patients diagnosed with lung cancer and subsequently developing brain metastases. To identify prognostic factors and examine their relationship with survival through retrospective analysis of patient data.
Material and Methods
This study was performed in accordance with the principles of the declaration of Helsinki and approved by the local ethical commitee (Sivas Cumhuriyet University Ethical Commitee). The data of 271 patients with lung cancer with brain metastases who applied to the Department of Radiation Oncology, Faculty of Medicine, Cumhuriyet University between 2007-2018 and were treated, were evaluated retrospectively. Demographic, clinical and histopathological data of the patients, age, gender, comorbidity, presence of hypertension, primary diagnosis, RPA, number of lesions, metastasectomy status and SRS parameters were obtained by examining patient files and hospital records. The performance status of the patients was made according to the Karnofsky Performance Score. Prognostic groups called RPA (Recursive Partitioning Analysis) have been determined by the Radiation Therapy Oncology Group (RTOG) according to their survival status [8]. RPA Group I includes patients under 65 years of age, with a Karnofsky Performance Status (KPS) of at least 70 and no extracranial organ metastases, with a median survival of 7.1 months. Group III refers to patients with KPS less than 70, and the median survival is 2.3 months. Group II was evaluated as all patients not included in RPA Group I and Group III, and the median survival was 4.2 months [8]. However, nowadays; In addition to age, performance status and extracranial disease spread, factors related to intracerebral tumor (number, size, type of primary tumor) and number of extracerebral organ involvement also have prognostic importance [9]. Three-dimensional conformal radiotherapy was applied to the patients in the Eclipse (ver. 8.6; Varian Medical Systems, Inc. Palo Alto, CA, USA) planning system on the Varian DHX device, with a total of 30 Gy of whole brain radiotherapy, 10 fractions x 3 Gy. Stereotactic Radiotherapy was administered with a Tomotherapy device (Tomo H VoLO planning system, Accuray Inc. Madison, WI, USA). A dose of 24 Gy was prescribed for metastatic lesions <2 cm, 18 Gy for metastatic lesions of 2-3 cm, and 15 Gy for lesions >3 cm [10].
Statistical analysis
SPSS version 22.0 was used for analysis. Descriptive tests were performed to determine the characteristics of the patients (median, mean, standard deviation, etc.). Survival times were calculated by Kaplan-Meier analysis. Multivariate analysis Cox regression analysis was performed to evaluate the prognostic factors and to evaluate the independent factors affecting survival. p value of ≤0.05 was considered statistically significant.
Results
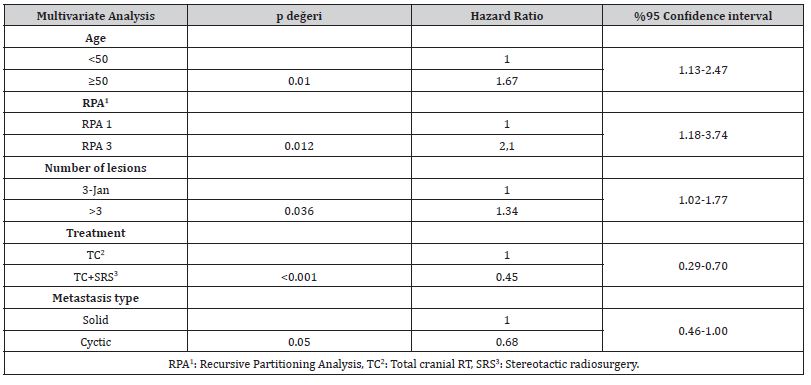
A total of 271 patients, 236 (13%) men and 35 (13%) women, who applied to our clinic with lung ca with brain metastases were included in the study. Comorbidity was present in 102 (38%) patients. 86% of all brain metastases contained solid and 14% cystic components. There was no difference between the groups in terms of age, RPA, KPS, histopathological subtype and treatment type, metastasectomy, presence of extracranial metastases and metastasectomy (Table 1). Since there were fewer metastatic lesions in patients with cystic nature, a statistically significant difference was found between the groups in terms of the number of lesions (p<0.05). The median survival of patients after metastasis is 6 months, 1-year survival 43% in patients with cystic metastasis, and 3 months and 1-year survival in solid nature patients is 21%. In univariate analysis, RPA (p<0.001), histological subtypes (p=0.009), age (p=0.019), number of lesions (p=0.001), total crainal RT+SRS (p<0.001), metastatectomy (p=0.001) statistically significant (Table 2). According to multivariate analysis, age >50, RPA I-III, number of lesions >3 and total cranial RT alone adversely affected the survival of the patients. The cystic type of metastasis improved survival (HR: 0.68, 95% CI: p=0.005) in Table 3.
Table 1:Demographic information.
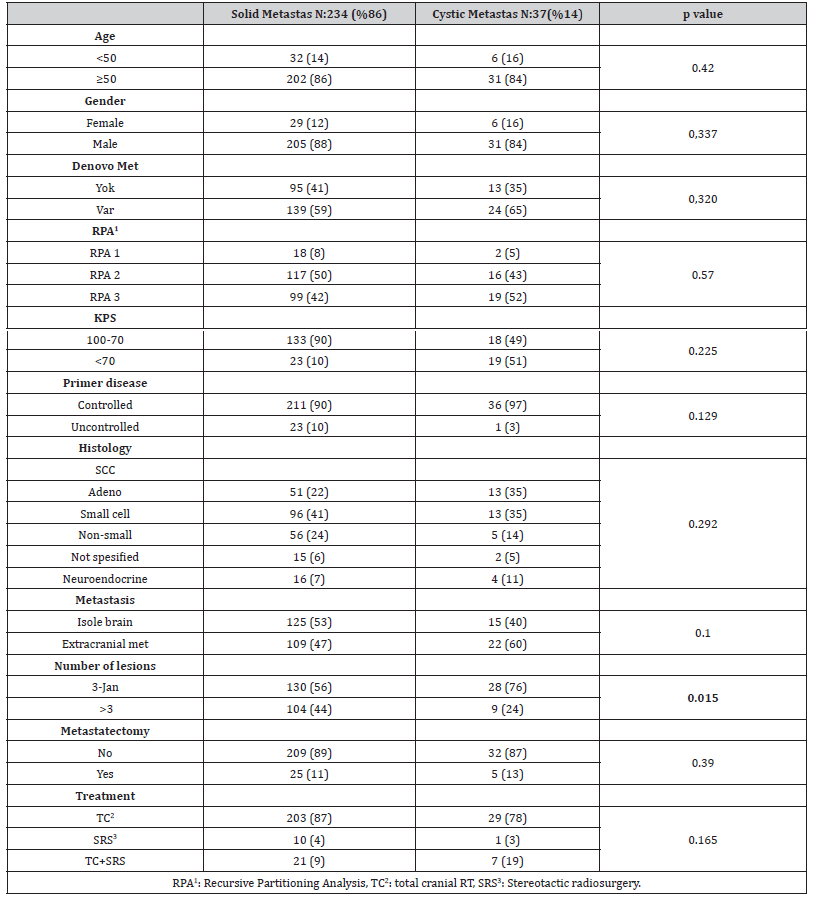
Table 2:Evaluation of parameters affecting survival with univariate analysis.

Table 3:
Discussion
Intracranial metastasis is a major complication in patients with lung cancer, and understanding its impact on survival is crucial for optimizing treatment strategies. In this study, we evaluated the effect of intracranial metastatic components on survival in patients with lung cancer and brain metastases. Our findings show that the presence of cystic metastases in brain lesions is associated with better survival compared with solid metastases. This is an interesting observation as cystic components in brain metastases are less reported. The underlying reasons for this association are not fully understood and require further investigation.
It is possible that the cystic nature of the metastasis is indicative of a less aggressive tumor biology or a slower growth rate, leading to a more favorable prognosis. In addition, cystic lesions may be more amenable to therapeutic interventions such as surgery or radiosurgery, which can contribute to improved survival outcomes. We also identified several other factors that significantly affect survival in patients with intracranial metastases. Age, KPS and RPA classification emerged as important predictors of survival. This highlights the importance of considering overall disease burden and patient performance status in determining prognosis. Histologic subtypes, age, and number of metastatic lesions were also found to affect survival, with older age, certain histologic subtypes, and greater number of lesions associated with worse outcomes. Treatment modalities such as total cranial radiotherapy and combined stereotactic radiosurgery and metastasectomy showed a positive effect on survival in univariate analysis. These findings are in line with established treatment approaches for brain metastases, which often use a combination of radiotherapy and surgery to achieve local control. It should be noted, however, that the decision to pursue such interventions should be made on a case-by-case basis, taking into account the patient’s overall clinical condition, extent of extracranial disease, and location and number of brain metastases.
Multivariate analysis revealed that over 50 years of age, RPA I-III, more lesions, and total cranial radiotherapy alone were independent prognostic predictors of worse survival. These findings highlight the importance of individualized treatment approaches, taking into account patient-specific factors. We observed a significant correlation between the nature of metastasis and survival outcomes in patients with cystic metastases showing better survival compared to those with solid lesions. There is controversy regarding the prognosis and treatment strategies of cystic BM. In a retrospective study, it was shown in a study that the survival time of patients with cystic brain metastases was shorter than in patients with solid brain metastases [11]. Xu et al. conducted a study specifically investigating the treatment and prognosis of solid and cystic brain metastases in patients with nonsmall cell lung cancer. Their findings may provide further insight into outcomes and management approaches in this specific patient population. No significant correlation was found between the nature of metastasis and survival outcomes in non-small cell lung cancer patients with cystic brain metastases [11]. This highlights the need for further research to better understand the complexity of the disease and the impact of metastasis features on prognosis. It is important to acknowledge the limitations of our study. The retrospective and relatively small sample size of the analysis may have caused selection bias and limited the generalizability of the findings. Additionally, the study did not evaluate specific molecular changes or targeted therapies that could affect survival outcomes.
In conclusion, our study provides insight into the effect of intracranial metastatic components on survival in patients with lung cancer. The presence of cystic metastases in brain lesions was associated with improved survival, while factors such as RPA classification, histological subtypes, age, and number of lesions were also important predictors of prognosis. These findings highlight the importance of a multidisciplinary approach that considers individual patient characteristics in the management of lung cancer patients with intracranial metastases. More research is needed to confirm these findings and explore the underlying mechanisms that contribute to the observed survival differences.
Conclusion
Introduction
Introduction
Our study distorted the perception that patients with previous cystic brain metastases have a worse prognosis. Patients over 50 years of age with RPA3, more than 3 brain metastases had a shorter survival time regardless of cystic or solid brain metastases. Total cranial RT and SRS were found to be better in patients who were applied together compared to those who had only TCRT. Of course, prospective randomized studies are needed to substantiate the results.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgment
None.
References
- Nayak L, Lee E Q, Wen P Y (2012) Epidemiology of brain metastases. Current Oncology Reports14(1): 48-54.
- Barnholtz-Sloan J S, Sloan A E, Davis F G, Vigneau F D, Lai P, et al. (2014) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. Journal of Clinical Oncology 22(14): 2865-72.
- Soffietti R, Rudà R, Mutani R (2010) Management of brain metastases. J Neurol 249(10): 1357-1369.
- Mehta MP, Paleologos NA, Mikkelsen T, Paula D Robinson, Mario Ammirati, et al. (2010) The role of chemotherapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96(1): 71-83.
- Patchell RA, Tibbs PA, Walsh JW, R J Dempsey, Y Maruyama, et al. (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8): 494-500.
- Brem SS, Bierman PJ, Brem H, Butowski N, Chamberlain MCet al. (2007) Central nervous system cancers. J Natl Compr Canc Netw 5(4): 348-372.
- Ceresoli GL, Cappuzzo F, Gregorc V, Bartolini S, Crinò L, et al. (2004) Gefitinib in patients with brain metastases from non-small-cell lung cancer: a prospective trial. Ann Oncol 15(7): 1042-1047.
- Gaspar L, Scott C, Rotman M, T Phillips, T Wasserman, et al. (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37: 745-751.
- Gerdan L, Segedin B, Nagy V, M T Khoa, N T Trang, et al. (2014) Brain metastasis from non-small cell lung cancer: prognostic importance of the number of involved extracranial organs. Strahlenther Onkol 190(1): 64-67.
- Shaw E, Scott C, Souhami L, Luis Souhami, Robert Dinapoli, et al. (2000) Single dose radio surgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 9005. Int J Radiat Oncol Biol Phys 47: 291.
- Sun B, Huang Z, Wu S, Hz SB, Ding L, et al. (2016) Cystic brain metastasis is associated with poor prognosis in patients with advanced breast cancer. Oncotarget 7(45): 74006-74014.
- Xu YB, Zhang Y, Song Z, Wang W, Shao L (2021) Treatment and prognosis of solid and cystic brain metastases in patients with non-small-cell lung cancer. Cancer Management and Research 13: 6309-6317.
-
Eda Erdıs* and Birsen Yucel. Prognostic Impact of Solid And Cystic Intracranial Metastases on Survival in Patients With Lung Cancer: A Retrospective Analysis. Curr Tr Clin & Med Sci. 3(4): 2023. CTCMS.MS.ID.000568.
-
Tumors, Surgery, Cystic metastases, Cranial RT, Metastasectomy, extracranial disease
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






