 Research Article
Research Article
Medication Assisted Treatment: Examining Enrollment and Demographic Factors of Treatment
Patrick J Aragon1* and Antwana L Drayton2
1Department of Clinical Psychology, Florida Institute of Technology, USA
2Department of Psychology, University of North Florida, USA
Patrick J Aragon, Department of Clinical Psychology, Florida Institute of Technology, USA.
Received Date: September 15, 2023; Published Date: October 18, 2023
Abstract
Opioid Use Disorder (OUD) has been a long-standing epidemic concern related to the continuous growth of variations of the substance and its’ potency. Due to the versatility of the substance to be both an illicit drug and also a prescription medication, the interest in controlling and monitoring its’ use creates a greater public health concern. Treatment overtime has been revitalized to directly address the social, biological, and physiological difficulties of patients with OUDs. Medication Assisted Treatment (MAT) has been explored and has become one of the most widely used plans for treatment of Substance Use Disorders (SUDs) related to pain management issues, dependency, withdrawal, and likelihood of maintaining sobriety. The use of MAT has been proven to be a positive and worthwhile addition to the treatment of OUDs. However, there are gaps in the administration and enrollment of individuals into the programs and facilities that offer MAT services. As this deficit is acknowledged, the current study was posed to examine the relationships among demographic factors relative to OUDs and MAT services. Data from a sample of 973 adults with a diagnosis of OUD relative to all opioid related substances, was analyzed in this study. Relationships among gender, race, employment, education, and types of treatment were explored. Types of treatment included Suboxone and Vivitrol. Overall, this study found that Suboxone treatment was administered more often than Vivitrol treatment. Also, outpatient service members used MAT services more often than inpatient members. Chi-square analyses and an Analysis of Variance were both utilized, indicating gender differences and educational differences. Likewise, specific race differences and employment attainment computed no significant conclusions. Contributions to the findings, limitations of the exploration, and future research directions are all discussed.
Keywords: Demographics; treatment; recidivism; medication; opioid; Vivitrol; Suboxone
Introduction
Individuals have been utilizing mind-altering and mood-altering substances throughout history so understanding the nature of illicit drug abuse and addiction is pivotal to addressing the substance use [1] However, scientific and technological advances have led to an increase in substance potency and the creation of new substances. These shifts create noted substance use difficulties that emerge with each variation of these naturally occurring substance forms. The depiction of these substances often used for healing has undergone significant scrutiny when the chemical makeup creates more addictive difficulties than positive outcomes. These addictions increase the importance of addressing and monitoring the costly and often tragic effects and impacts of use. Specifically, the use of opioids and the continuous altering of the substance warrants exploration due to the constant shift of production and therefore treatment of those with related ailments.
Review of the Literature
The theme of substance use continues to negatively impact individuals’ lives and their family, school, workplace, and community roles. It is reported that over 2 percent of the worlds’ population has alcohol or illicit drug addiction [2]. What has become evident is that the amount of destruction experienced by the individuals and those closest to them exceeds intoxication, addiction, and dependence. More specifically, drug use is reported to be responsible, both directly and indirectly, for more than 11.8 million deaths per year. Directly, drug use results in over 350,000 overdose deaths yearly. Indirectly, the use of these substances affects mental and physical health, causing premature death related to the disease by way of various risk factors [3]. Risk factors such as environmental markers are essential to consider when evaluating the likelihood of sustained recovery and medication access. However, the financial costs of treatment and lack of adequate resources contribute to disparities in substance abuse treatment completion, identifiable within socioeconomic factors differences [4,5]. Therefore, this study will examine the utilization of treatment options relative to identified demographic and ecological factors associated with Opioid Use Disorder (OUD).
Opioid Use Disorder
Of the eight categories listed in the DSM-V for diagnostic considerations, OUD is included and specific to this study. Opioids are a class of drugs that includes prescription pain relievers, oxycodone, hydrocodone, codeine, morphine, fentanyl, and heroin [6]. There are continued fluctuations of opioid users from one substance to another, both across a population and within individual case histories. The impact continues to be acknowledged in cases of users in medical and non-medical fields. Historically, Opioids were utilized as a common pain medication within medical operations, traumatic injuries, and even common coughs and sleeplessness [7,8]. However, the awareness of differences in potency and chemical compositions created a need for a controlled administration of the substance, which exposed potential misuse, leading to addiction and, ultimately, the disorder.
Biological Component of Opioids: Opioid receptors are widely studied. Due to their crucial role in mood disorders, pain management, and drug addiction, research is utilized to establish structural and mechanistic insights into their purpose and function (Shang & Filizola, 2015). Opioid receptors belong to the G-protein coupled receptors. These receptors are the most abundant class of cell-surfaced receptors and the target of at least one-third of approved and marketed drugs (Vortherms and Roths, 2005). The four major subtypes of opioid receptors are the Delta, Mu, Kappa, and Zeta receptors. They mediate the human body’s response to most hormones, neurotransmitters, drugs. They are also involved in the sensory perception of vision, taste, and olfaction (Dhaliwal and Gupta, 2019). The traditional model proposes that the binding of an opioid to a receptor activates an associated G-protein, which then triggers a biological response (Filizola and Devi, 2012). Different types of opioid receptors bind to their respective agonist counterparts. Dopamine is responsible for the rewarding effects produced by opioid administration that lead to positive reinforcement. However, similar to positive reinforcement are the issues and concerns that arise in terms of genetic variances associated with increased dependence on opioids. Likewise, despite their analgesic effects, opioid drugs are accompanied by various side effects. These side effects include but are not limited to vomiting, nausea, constipation, tolerance, and addiction (Feng et al., 2012).
Use of Opioids for Pain Management: According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2016, 11.4 million people (4.4 percent of the total population) misused opioids [9]. 97.4 percent of people misused prescription pain relievers, and 8 percent of individuals’ being heroin users. Moreover, 5.4 percent is a combination of prescription and heroin users. Additionally, 2.1 million Americans were diagnosed with OUD, and only 20 percent of individuals with OUDs received specialty addiction treatment.
In 2018, Florida providers wrote 53.7 opioid prescriptions for every 100 people, compared to the average U.S. rate of 51.4 opioid prescriptions [10]. Of the 4,698 reported drug overdose deaths in Florida in 2018, nearly 68 percent (3,189 fatalities) involved opioids. Deaths involving synthetic opioids other than methadone (mainly fentanyl and fentanyl analogs) were high at 2,091but remained stable. Similarly, deaths involving heroin and prescription opioids remained steady at 680 and 1,282 in 2018. Related to Neonatal Abstinence Syndrome (NAS) and Neonatal Withdrawal Syndrome (NOS), which occurs when a woman uses opioids during pregnancy, the 2017 rate of NAS/NOWS in Florida was 7.3 cases per 1,000 hospital births [11].
Treatment
Historically, addiction and mental illness were misunderstood and treated with identical methods. Lack of understanding and technological advances permitted the separation and hospitalization of individuals that did not fit into the social norms. Before the 1800s, pain was regarded as a consequence of aging, and therefore, no regulation of the use of substances such as cocaine and opioids existed [12]. This lack of regulation resulted in widespread marketing and a prescription for many ailments [13]. Around the 1900s- 1930s, continued discord was illustrated in treatment forms. Medical supervisors of asylums and prisons were granted the authority to “asexualize” those with mental health and substance use disorders, considering these individuals degenerates [14]. Also, street heroin abuse and iatrogenic morphine dependence sparked the passing of the Harrison Control Act of 1914, which influenced avoidance of opiates [15]. This Act caused individuals to be recognized as deluded and malingering and encouraged individuals in need of opiates, such as cancer patients, to essentially avoid the medication until they likely died [12]. Another consequence of this Act was its restrictions of prescribing to addicts eliminated a safe, legal way to obtain the substance. Attempts at facilitating clinics and centers for morphine and narcotics were created but closed for legal reasons, likely related to instances of inhumane and unlawful research practices [16].
Over time, the idea of treating pain and related under-treatment of pain was revisited. Research and trials were again developed to address severe pain and the positive or negative effects of opioid use. The World Health Organization (WHO) and American Pain Society launched investigations into operational definitions of pain and cancer treatment instead of chronic pain management [17,18]. The Joint Commission published standards for pain management in the 2000s that would require organizations to quantify pain assessments as regulated by the Institute of Medicine (Baker, 2017). This publication facilitated the need to prescribe opiates more generously with backing from pharmaceutical companies, insurance companies, and federal healthcare funds allocated to those in compliance.
However, the negative consequences became apparent in the physicians’ felt requirement to prescribe opiates. These consequences were illustrated in the over-prescription of opiates, patient’s reliance on the substance, pharmaceutical companies introducing new formulations, and an overall increase of opioid consumption [19]. Additional consequences were related to pressure and stigma that failure to prescribe would conclude that the physician is acting inhumanely, and possible litigation for under-treatment of pain was possible. Most noticeably, there was a rise in additional deficits and disabilities due to the overprescription, a rise in federal charges against pharmaceutical companies and physicians, and most importantly, a rise in opioidrelated misuse and deaths. As a response to the current epidemic, we are experiencing, laws and policies were created to limit the prescription of opiates and address the addiction that is likely to occur. However, individuals found alternative methods to address those addictions, using the black market and street heroin and increased use and preference for fentanyl [12,20]. Emphasis on alternative methods and combined treatment methods have been implemented to address further the epidemic we face. As it relates, empirical data and literature will be explored relative to treatment funding as well as types and phases of treatment.
Phases of treatment
The early forms of substance use treatment became viewed as cruel and unusual punishments, with the medical community acknowledging that addiction can be treated through more humane methods. The idea was accepted that brain chemistry is altered through regular substance use, leading to behavioral changes and unavoidable drug-abusing behaviors, and created drug dependence that is likely best treated by pharmacological and therapeutic methods. Individuals experience different stages and phases of addiction treatment compared to previous experiences. Intake involves meeting with a professional to discuss treatment options with a personalized treatment plan based on assessing the medical, emotional, behavioral, and social functioning. The inclusion of co-occurring and dual diagnoses treatment allows for additional treatment options to be explored that address the mental illnesses coupled with a substance use disorder [21]. These treatment options can be identified in phases of treatment and additional options for individuals diagnosed and battling with OUDs.
Detoxification Phase: Detoxification is the stage in which an individual is experiencing withdrawal syndromes that may involve uncomfortable and possibly dangerous symptoms. Supervision, monitoring, and pharmacological interventions are utilized to assist in detoxification [22]. These interventions address the markedly unpleasant and often dangerous symptoms individuals’ experience. Historically, detoxification was misunderstood in terms of certain substances, which often made the process more difficult, created complications, and potentially lead to death. Due to continuous scientific research and studies, professionals better understand utilizing substances to ease certain drugs’ withdrawal symptoms, including heroin and prescription opioids [23]. A medically supervised detox utilizes certain medications that depend on the specific substance that is being abused [24]. While the specific pharmacotherapeutic procedure is likely to differ, the type of substance dependence and the potential severity associated with the withdrawal symptom is often similar.
Rehabilitation and Support Phase: Like the timeframe and extent of detoxification, the necessity and types of treatment programs available and explored by the individual are similar. Inpatient treatment programs are utilized to separate the individual from the environments conducive to continuous substance use and prove harmful and problematic. The facilities offer continuous care and monitoring for the individual in an environment meant to assist in rehabilitation. These environments serve as a positive alternative to teach new ways of life for the individual and their road to recovery. They are also geared towards individuals with severe and extensive addictions and often used to stabilize that individual. Residential treatment also offers 24-hour care but is often in a non-hospital setting, focusing on the individual’s resocialization. The residential treatment programs can be short-term or long-term stays, relative to the individual’s needs and their substance of choice as main factors [25]. The program uses the staff, residents, and established social comradery to help individuals establish accountability and routine to return to society [21] eventually.
Outpatient and Rehabilitation Programs: However, individuals with family and work obligations tend to have difficulty finding inpatient facilities that can accommodate their schedules for extended periods. Even with facilities that have programs specific to families, and work-study, the idea is that the individual will eventually enter back into society and learn to maintain recovery with the support of the systems they developed during inpatient or residential treatment [25]. Outpatient programs are then a good option for those individuals that need recovery assistance that would allow them to maintain those responsibilities. Likewise, outpatient services are more equipped to manage milder addictions and sustain sobriety. There are also intensive outpatient programs that are direct services for individuals with substance use disorders or co-occurring mental and substance use disorders that do not require medical detoxification or 24-hour supervision [26]. Still, they are designed to establish psychosocial supports and facilitate relapse prevention and coping mechanisms; they have been essential in the continuum of care for those individuals. Transitional, aftercare, and recovery support programs are also utilized, such as sober living homes and halfway houses, to assist in continued recovery care relative to the individual needs’ accountability before going back to their homes. Additionally, in all treatment programs, Alcoholics Anonymous (A.A.) and Narcotics Anonymous (N.A.) meetings are offered, required, and encouraged by the facilities to ensure continued engagement in the recovery community.
Recovery Support Groups: Self-help therapy, such as Narcotics Anonymous (N.A.) and Alcoholics Anonymous (A.A.) groups, emphasize that individuality and one single treatment method will not produce effective recovery [27,28]. In these groups and meetings, individuals discuss the difficulties and experiences they have had with substance use disorders, the effect on their family and their lives, and their recovery process. The literature on the components of N.A. and A.A. that make it beneficial has had limited research. However, it has been shown that individuals referred to 12-step groups had better alcohol and drug use outcomes at six-months, and ultimately 12-step involvement being a partial mediator between outcome and condition [29]. Studies have also shown that the interconnectedness of spirituality, self-efficacy, coping, and social support are intricate components that facilitate change [30]. Individuals who engage in these groups tend to have higher levels of social support from peers and benefit more than individuals with fewer friends and less stable social network composition. Essentially, the stages of recovery of the individuals and felt level of the community assist in abstaining from substance use.
Additional factors that have been considered to the effectiveness of recovery support groups are the inclusion of other protective components. For instance, sponsorship is an essential component of recovery, and studies have shown that having a sponsor increased involvement and recovery outcomes [31]. Likewise, an individual’s view on natural supports such as family and perceived environmental stressors can affect their likelihood of completing treatment requirements and maintaining sobriety. For instance, court-ordered participants have indicated that recovery support groups tend to be the most beneficial aspects of drug court, which encouraged completion of the program [32]. However, similar to the literature, factors such as their environment, culture, and family support can also become indicators that hinder the likelihood of recovery maintenance [33]. Because of the limited nature of how support groups work, more literature would need to be conducted to illustrate further the effectiveness of support groups related to perceived environmental stressors.
Therapeutic and Psychosocial Treatment Phase: An essential addition to substance use disorders is the utilization of therapeutic techniques in conjunction with substance abuse treatment. With the shifting view of substance use disorders, scientists and medical professionals understand that the therapy aspect of treatment is specific to addressing long-term recovery by getting to the core of the reasons for addiction [22]. This aspect addresses the issues they have experienced in the past and will likely face in the future but with alternative and more positive coping mechanisms in play to address those issues to deter them from relapse. Individual therapy often addresses core difficulties, trigger identification, coping mechanisms, time management, and reconstruction of thinking patterns.
Additionally, Group and Family therapy are often encouraged to help resolve issues that have contributed to the individual’s substance use and are likely to hinder the recovery process [24]. It is also utilized to foster connection and cohesion with the support system that the individual is likely to need during re-entry into society. Likewise, case management and peer recovery are offered to assist in the tangible aspects that would hinder an individual from re-acclimating to society. Occupational, educational, and vocational exploration are often included in this treatment aspect.
Medication-Assisted Treatment (MAT)
In addition to traditional substance use disorder treatments such as inpatient or outpatient, MAT has been implemented. This treatment combines medications such as methadone, buprenorphine, or naltrexone, with counseling and behavioral therapies. These three FDA-approved medications are used to treat cravings and to prevent relapse. The three medications are ligands that bind to and target the mu-opioid receptors that are necessary for the therapeutic activity. However, they differ in their intrinsic activities at the mu-opioid receptor and the pharmacokinetic and pharmacodynamics properties. They also differ in the mechanisms that confer relapse-prevention protection to the treated individual. While methadone has been recognized as one of the older and more widely utilized forms of MAT for OUD, there have also been many difficulties with regulation regarding weaning and sex differences.
Methadone: Methadone has a proven success rate in the treatment of OUD. However, individuals on this medication have a lower likelihood of successful titration without implementing an alternative medication or substance [34]. Likewise, similar to opioid abuse and dependence, individuals utilizing methadone often undergo detoxification and withdrawal from the substance itself due to its inherent properties. For this particular study, the use of methadone, while acknowledged as a potential treatment, will not be explored in this study.
Buprenorphine and Suboxone: Buprenorphine is a partial agonist. The medication activates the opioid receptors to a lesser extent than full agonists [35]. While Buprenorphine can have similar effects as full agonists (i.e., fentanyl, heroin, morphine, and oxycodone), it loses effectiveness at higher doses [36]. Buprenorphine can be used as a pain reliever, but when taken correctly, it does not create the euphoric state that is associated with substances such as morphine or heroin. It has also been demonstrated to have a good safety profile, low physical dependences, and flexible dosing schedules [37]. Likewise, it will prevent withdrawal symptoms and reduce cravings for opiate drugs when used correctly.
Medications such as Subutex and Suboxone contain buprenorphine. Subutex was developed first, and opioid users have been found to inject the drug intravenously to obtain the high they would experience from other drugs such as heroin and prescription medications. Therefore, Suboxone was created to combat that tendency. Suboxone contains both buprenorphine and naloxone. Naloxone is an opioid antagonist, which blocks the effects of the opioids at the receptor site [36]. Buprenorphine and naloxone have been evaluated as an analgesic combination used to reduce potential abuse, including inpatient-controlled paradigms [38]. If an individual attempts to inject Suboxone, they will go into precipitated withdrawal, which tends to distress the individual. Severe addictions, or those diagnosed with a moderate or severe diagnosis code, are seeing more use of Suboxone than Subutex because of naloxone and the reduced likelihood of abuse. Suboxone is administered as a sublingual tablet, placed under the tongue until it is dissolved. Suboxone is available in two dosage strengths: 2 mg buprenorphine with 0.5 mg naloxone and 8 mg buprenorphine with 2 mg naloxone. Appropriate dosage and titration of medication to the individual will be specific to the facility and individual’s needs. Suboxone provided sublingually was developed to reduce the potential of abuse in supervised dosing and make it more difficult to remove [39]. The sublingual version dissolves faster than the tablets and reduces the likelihood that individuals will misuse the substance later through crushing or snorting, as is the case with the tablets. Suboxone is the focus of this particular study.
Naltrexone and Vivitrol: Naltrexone is a long-acting antagonist at the opioid receptors that block the subjective and objective responses of the medication that is produced by intravenous opioid use [40]. Naltrexone has also been studied as favorable and effective treatment for alcohol use disorder relative to reduced drinking and the number of drinks consumed on such days, compared to placebos [41]. Likewise, studies have shown that naltrexone treatment efficacy improves alcohol abstinence over time across various outcome measures for individuals who completed treatment and were highly compliant with taking the medication (Blanco-Gandia & Rodriguez-Arias, 2018; [42]. Additional studies have indicated that oral naltrexone helps reduce heroin cravings. Highly motivated patients have shown favorable treatment success rates during naltrexone therapy, remaining opioid-free longer than less motivated patients [43]. However, studies have also shown that extended-release naltrexone versus oral naltrexone tablets can improve adherence and decrease discontinuation, as it is administered as an intramuscular injection approximately every 28 days and not daily [44,45].
Family support, psychotherapy, and counseling, combined with naltrexone therapy, showed a greater likelihood of remaining opioid-free. Research has indicated that naltrexone is beneficial in reducing opioid use. Retention such as contingency management is vital in treating opioid dependence with naltrexone [46]. Vivitrol is an FDA-approved extended-release injectable form of naltrexone. An individual must be at least seven to ten (and sometimes fourteen days) post-detox from opioid use before utilizing Vivitrol. It is a once-monthly extended-release injectable (380 mg) non-addictive and non-narcotic and should be used as part of a management program that includes psychosocial support [47,48]. Studies have indicated that individuals utilizing Vivitrol and remained in management programs have had higher senses of control over their use and lower recidivism rates [49]. Although Vivitrol is made available to many facilities, the utilization appears to be more prominent in high-restriction treatment facilities.
Suboxone and Vivitrol Comparison: The medication that individuals choose is often related to their stage of sobriety and availability of medications. For instance, patients who are not already opioid-free, Suboxone is preferable to Vivitrol, when both are clinically appropriate and indicated [50]. Suboxone addresses severe OUDs of individuals in which complete detoxification would be dangerous and difficult. Likewise, although both medications are comparably effective and safe options, agonists (Suboxone) treatment is often encouraged when induction or initiation into antagonist (Vivitrol) treatment is not successful [51]. Individuals with more severe OUDs have reported that Vivitrol effectiveness decreases before the next injection, and individuals experience cravings for opioids [52]. This occurrence increases the likelihood of opioid overdose death, injury, or coma if an individual tries to challenge the opioid blockade [53]. However, Suboxone can be misused and abused. Individuals prescribed Suboxone may take more than prescribed to receive an opiate high [54]. Individuals may abuse Suboxone recreationally, finding that places with high heroin abuse rates also report Suboxone abuse. For example, Suboxone can be snorted, and the film strips can be dissolved and then injected, with injections causing a much more intense high than snorting the pills [55,56].
In terms of reducing overdose deaths, Vivitrol appears to be more cost-effective. The benefit is expressed in the individual’s increased quality of life and years of opioid abstinence [57]. It is also reflected in the decrease in the need for high-cost healthcare services such as emergency department visits and the cost of overdose deaths. The extended-release component allows for more extended periods of not needing to return for dosages and craving reduction [45]. However, it does not appear to be more costeffective using generally accepted value thresholds for quality of life, willingness to pay, and the high price [57]. Individuals are often unable to pay for the extended-release injection and the reduction of effectiveness over the days tends to vary. However, suppose state addiction treatment payers can assist and offset the payment required for the injection. In that case, the medication could be a cost-effective option for reducing opioid overdose deaths [58].
Relatedly, Suboxone prescriptions appear to be written more than Vivitrol. Assumptions indicate more familiarity with Suboxone, less painful detoxification processes, and euphoric association differences between the two [59,60]. Both medications are met with significant insurance barriers, such as extensive pre-authorization processes. However, the monthly injection’s high cost is often met with more barriers than that of Suboxone. Therefore, while both medications’ success rates have appeared to be high, individuals with insurance and means to engage in inpatient treatment are more likely to engage in Vivitrol treatment; however, this is relative to education on Vivitrol and the severity of OUD.
Access to treatment options is often dependent upon race, income, geography, and insurance status rather than individual preferences of medical or psychiatric indicators. A cross-sectional study indicated that counties that were of highly segregated African American/Black and Hispanic/Latino communities utilized more methadone facilities [61]. In contrast, those counties with highly segregated Caucasian/White communities utilized more buprenorphine facilities. Additional studies indicate that buprenorphine treatment has increased in higher-income areas with lower percentages of African American/Black, Hispanic/ Latino, and low-income residents. In comparison, methadone rates remain stable over time and continue to collect in urban low-income areas [62]. Black/African Americans in the U.S. with OUDs were less likely to receive buprenorphine than Whites [63]. The individuals who were able to self-pay or had private insurance represented nearly 74 percent of those who received buprenorphine treatment from 2012-2015. Buprenorphine is also an office-based treatment program that often only works for patients with access to primary care practitioners to prescribe and administer, likely inaccessible to low-income or uninsured individuals. The use of Vivitrol generated minimal information on the demographics of its users, as the effect of race has not been explored thoroughly. However, the general observation has been that Caucasian males are more likely to seek and obtain substance use treatment than other populations. Therefore, those related treatment indicators such as insurance, income, race/ethnicity, and geographic location also imply barriers for patients and clinicians who do not meet the favored criteria.
Rationale for Proposed Study
The growing frequency of OUD and overdose deaths involving opioids has reached epidemic levels since the 1990s [64]. Between 2002 and 2018, the prevalence of heroin use and disorder has nearly doubled (Han, Volkow, Compton, & McCance-Katz, 2020). The use of illicit synthetic opioids such as fentanyl has also increased in the United States. It is reported that approximately two-thirds of people who primarily use heroin have also reported a comorbid utilization of prescription opioids (Rosenblum et al., 2007). According to the literature, the” first opioid of choice” is frequently a prescription opioid and not heroin [65]. Taken together, there are different routes for an individual to develop an OUD which contributes to a continued public health concern. Relatedly, the need to further understand the available treatment options dedicated to addressing the disorder remains to be a necessity in research.
Addictive use of substances such as opium and heroin, along with drug-related crime (especially in poor urban communities), increased concern of those with social, religious, and political leadership (Center for Substance Abuse Treatment, 2005). The increasing challenges in the face of the individuals using opioids are related to access to the substance relative to treatment access. The development of MAT uses medications, in conjunction with counseling and behavioral therapies, to provide a different approach to treating the substance use disorder [9]. The goals of using MAT are to focus on increasing the individuals’ survival rate, increase maintenance of treatment, decrease delinquency amongst the substance users, assist in maintaining employment, and improve pregnant women’s birth outcomes using the substance. The development of Vivitrol and Suboxone medications is related to continued research of identified substances that can assist the patient in achieving and maintaining recovery.
There is empirical support that MAT is a positive reduction of opioid use disorder-related symptoms, reducing the risk of infectious disease transmission and criminal behavior associated with substance use [10]. Individuals utilizing buprenorphine/ naloxone (Suboxone) of 16 mg or more per day were 1.82 times more likely to stay in treatment and decreased the number of opioid-positive drug tests by 14.2 percent [66,11]. Likewise, extended-release injectable naltrexone (Vivitrol) produced 90 percent confirmed abstinent weeks compared to 35 percent in a placebo study group produced in Russia [25,44]. The substances’ effectiveness is similar to treatment but different in administration and obtaining the medications. Thus, this research aims to explore the use of the identified MATs and how they have been utilized to treat OUD.
In detail, this study evaluates the application of Suboxone and Vivitrol in a treatment facility to assess how these medications address opioid addiction and recidivism (or the likelihood of relapse). By evaluating the adherence of individuals to the proposed treatment methods of MAT through outpatient and inpatient treatment options, the objective is to assess how identified demographic factors affect the adherence to the treatment and admission to the available programs. Additionally, the objective is to evaluate how these treatment options can be assessed to provide additional support for MAT services and modifications for future use related to demographic markers.
Objectives and Hypotheses
Objective 1: To determine if there is a notable difference in the enrollment into MAT from individuals utilizing inpatient and outpatient services. Although medically assisted “detoxification” treatment is considered to have restricted efficiency as a standalone treatment route, it often functions as the link between abstinence and maintenance treatment (National Collaborating Centre for Mental Health, 2008). A hospital setting permits a higher level of medical supervision and safety for individuals who require intensive monitoring [67]. Inpatient treatment also allows for interruption of cyclic drug use even in the absence of medically dangerous symptoms. With more comprehensive inpatient settings, individuals can focus attention on the precipitating familial, vocational, medical, and psychiatric issues.
However, outpatient treatment options require the individual to be subjected to the daily situations they are likely to encounter on discharge, which is likely to promote more effective coping skills but the equal risk of relapse. The reported rate of successful completion of opioid detoxification varies between 4% and 100% in studies, with higher rates in studies conducted in an inpatient setting [68, 67]. Additionally, MATs are exercised after individuals have completed detoxification and sustained abstinence for at least a week or more, which may present as problematic for outpatient settings [69]. Considering this information, it is expected that there will be more individuals enrolling in MAT that have utilized inpatient services than outpatient services alone.
Hypothesis 1
There will be higher rates of inpatient MAT treatment enrollment than outpatient.
Objective 2: To determine if there is a notable difference in seeking and enrolling into MAT options of Vivitrol and Suboxone. Vivitrol and Suboxone are proven to both be plausible MAT options. Buprenorphine products have steadily become the most commonly prescribed and accessible forms of evidence-based opioid treatment [12,51]. Extended-release injectable naltrexone was developed to provide sustained opioid receptor blockage, improve long-term adherence, and improve overall effectiveness [45]. There are, however, differences in the administration of the treatment and the adherence to the treatment regimen. Both medications are equally safe and effective.
Hypothesis 2
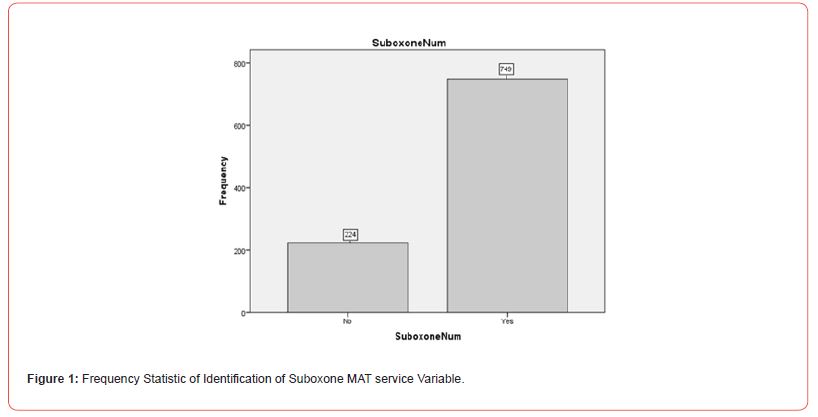
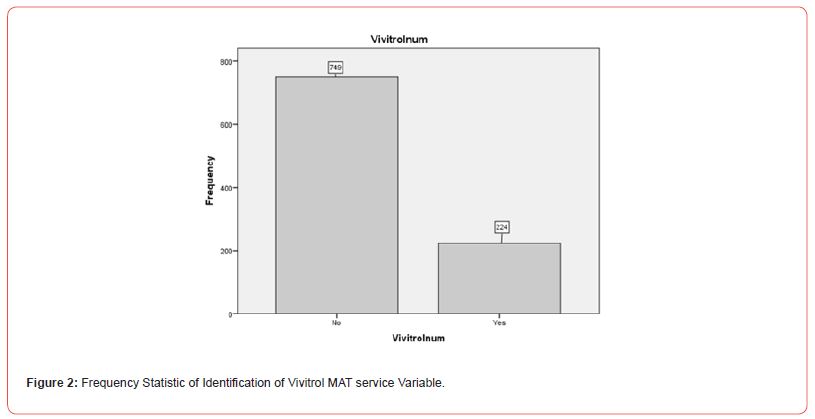
There will be higher rates of Suboxone MAT enrollment than Vivitrol MAT enrollment as it relates to the cost differential Figure 1 and Figure 2.
Objective 3: To determine if there is a noted gender difference for engagement of MAT. Substance abuse treatment has been shown to benefit both women and men engaging in comprehensive services such as educational, housing, income support services, and posttreatment services [70]. Men and women differ concerning the patterns of substance use disorders, their physiological responses to the substances, psychiatric comorbidities discovered, and barriers to treatment [71]. Men tend to engage in treatment through recommendation or mandate by social institutions such as employers or the criminal justice system whereas, women tend to enter treatment through social work referrals (Grella & Joshi, 1999).
Hypothesis 3
There will be more MAT treatment enrollment by males than females.
Objective 4: To determine if there are noted differences among enrollment into MAT programs as it relates to race/ethnicity. There are noted concerns about the structural and programmatic barriers associated with MAT provisions and utilization [72]. Many of the concerns are related to the racial/ethnic disparities represented. For instance, racial/ethnic minorities with OUD often suffer worse health outcomes that are related to their involvement with the criminal justice system, increased exposure to violence, and experiences with medical complications [73,74]. White individuals are more likely to engage in treatment due to access to care, awareness of care, and financial and community resources exercised for substance use care. Likewise, studies show that racial/ethnic minorities experienced lower treatment retention rates and completion and more prolonged treatment episodes than their White counterparts.
Hypothesis 4
Caucasian males will utilize MAT services more than any other demographic group.
Objective 5: To determine if there are income and employmentrelated differences amongst individuals that engage in MAT services. The literature provides that individuals meeting criteria for disability and low-income backgrounds count on Medicaid assistance to offset the cost of healthcare [72]. However, many states and programs within states do not permit Medicaid payments for services provided by an opioid treatment program. Likewise, several insurance companies do not cover the cost of these programs. Nonwhite racial/ethnic groups, which generally have lower income than whites and experience more significant healthcare disparities, are the fastest-growing population of opioid users in the United States [75,76]. The ability to afford the treatment, more established treatment facilities, and additional tangible resources to maintain treatment all represent barriers for lower-income individuals. Although some states expanded Medicaid coverage for substance use disorder treatment, low socioeconomic groups likely do not have coverage [77-79,74]. Considering this information, it is expected that employed individuals will be more likely to engage in the MAT programs than their unemployed counterparts. Those under the poverty line will likely be offered Vivitrol more than those employed due to the medication’s lasting effects but are likely to utilize Suboxone more due to cost.
Hypothesis 5
Individuals who are employed will have greater enrollment admission to Suboxone and Vivitrol MAT programs than unemployed individuals.
Objective 6: To determine the effect of education level on engagement in MAT. Individuals with low education levels often experience limited job opportunities and poor economic prospects, which leaves them vulnerable to drug addiction. These individuals are likely to reside in rural areas, likely have fewer resources to address drug addiction, and are likely vulnerable to financial incentives to participate in operations related to opioids [80].
Hypothesis 6
Higher educational attainment will increase an individual’s prospect of enrollment to Suboxone and Vivitrol MAT programs as it relates to employment status.
Methods
Via an application and initial review by the Florida Institute of Technology Institutional Review Board (Project #21-056), the IRB informed the researchers of the project’s exempt status, with permission granted for use of archival data. The data was provided by a data collection and storing system generated by Gateway Community Services (GCS). Established in 1978 and located in Northeast Florida, GCS is a facility with various treatment and recovery-based forms of services, including detoxification, behavioral and psychosocial rehabilitation (such as counseling, case management, and peer recovery) MAT. This program also provides patient-centered care that produces a combination of individual and group counseling and support groups. They also provide inpatient (residential) and outpatient treatment options with selfpay, private, and public insurance options. Additionally, they offer medications such as Suboxone and Vivitrol, with education for the use of either. This facility was chosen due to the assortment of treatment programs offered to the patient, extensive knowledge of use and diagnoses of substance use disorders, and the longevity of the facility’s commitment to substance use.
Sample
A 2018-2019 data sample was used from GCS. The data from 973 adult treatment participants at GCS was included for analyses. The participants ranged in age from 18 to 85-years-old, each experiencing different recovery stages that range from 1-750 days. There was also a range of substance use diagnoses available. For this research, the emphasis was placed on heroin and other opioid diagnoses with various substance use diagnoses and opioid treatment. However, the individuals included were specific to opioid-related diagnoses and engaged in MAT services. Individually identifiable information was removed before analysis to protect participant anonymity, and group summary results were included. However, individuals were provided informed consent at the time of data collection.
Variables
Demographic information was collected for each of the individuals. This demographic information included: age (no date of birth), sex, race, ethnicity, marital status, parental status, education level, employment status, annual family income, length of program enrollment in days, and reason for discharge from the program. Other variables explored were the primary, secondary, and tertiary substance use diagnoses; individuals identifying as completing treatment (Yes or No); those using MAT treatment (Suboxone (Yes or No); Vivitrol (Yes or No); and the individuals identified as using heroin/opioids (Yes or No). To illustrate inpatient services, individuals identified as engaging and completing designated inpatient services. To illustrate outpatient services, variables such as which outpatient services were included for analysis were included. The questionnaire was not included for this study due to lack of access of the variables that were not utilized in the study.
Data Modification: Archival data was originally collected by GCS staff evaluators who administered client assessments upon client application and entry to the treatment facility. Additionally, GCS staff entered and coded the data into the central GCS database. The individuals provided information on their drug of choice when completing the assessment. Likewise, urinalysis was collected at the entry of the facility. Individuals involved with MAT and Vivitrol services are also drug screened before receiving medication to ensure that individuals are detoxed and do not have other substances in their system that would interfere with the substance’s treatment effectiveness at the time of administration. At the time of administration, authorization of release forms and multiple consent forms were collected from the individual for treatment and collection of the information utilized. The data used for the current study represented a 2018-2019 data sample for the facility.
Results
Participants
A total of 1023 participants were utilized in the sample. Of this total, 50 cases were removed due to missing values and overlapping information that did not maintain the parameters necessary for discrimination regarding compliance data. As distinguishing between individuals identified as using one or the other MAT services was important, participants who did not use one or the other, or identified as using both MATs offered at the facility during their engagement in the program, were all removed. Therefore, 973 cases remained and were reviewed for this study.
Among the remaining 973 participants, 49% identified as Male (n = 477) and 51% identified as Female (n = 496). Relative to race, 86.9% (n = 846) identified as White, 6.1% (n = 59) identified as Black, 5.7% (n = 55) identified as Multi-Racial, and individuals identifying as “Other” in the table configuration were composed of 1.0% (n = 10) identifying as American Indian/Alaskan, 0.1% (n = 1) Hawaiian/Pacific Islander, and 0.2% (n = 2) Asian for a total of 1.34% (n=13). Of the participants, 4.5% (n = 44) identified as being of Hispanic decent and 95.5% (n = 929) identified as Non-Hispanic. See Table 1 for further participant demographic information.
Pertaining to employment, 30.5% (n = 297) of individuals identified as having some source of employment, and 69.5% (n = 676) identified as unemployed. See Table 2 for further participant employment and education information.
Table 1: Means and Standard Deviation for Adult Demographic Information.
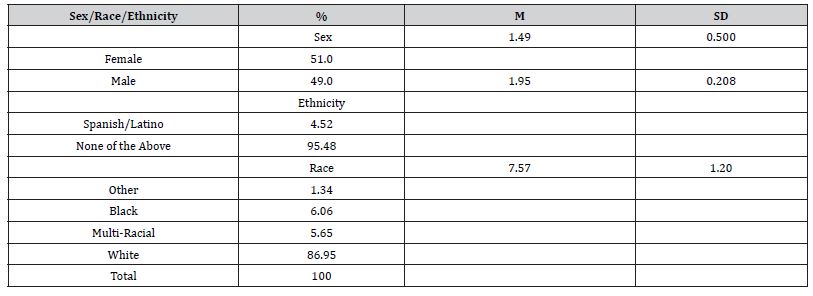
Table 2: Means and Standard Deviation for Adult Demographic Information.
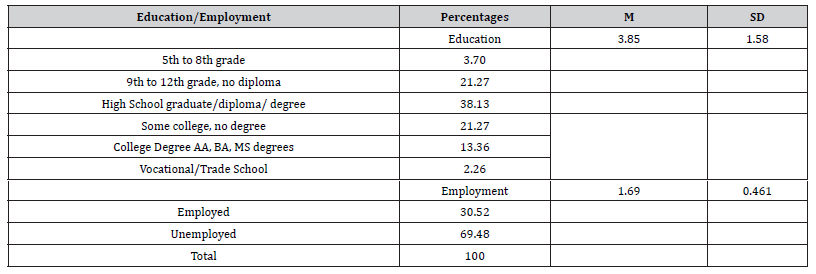
As it relates to education, 36% (n = 36) identified as having a 5th to 8th-grade education, 21.3% (n = 207) identified as having a 9th to 12th-grade education with no diploma, 38.1% (n = 371) identified as having a High School Diploma, 21.3% (n = 207) identified as having some college but no degree, 2.3% (n = 22) identified as having Vocational or Trade degrees, and 13.4% (n = 130) identified as having an Associates, Bachelors, or Master’s degree.
Statistical Analyses
Inpatient and Outpatient Enrollment: When analyzing the data for inpatient and outpatient services, it was discovered that 51.2% (n = 498) of the patients involved in MAT services utilized a service identified as “Medical Services.” This episode is to be identified as both inpatient and outpatient services. This episode of care was controlled for, and analysis was further conducted on episodes of care that were identified as inpatient versus outpatient services.
To explore whether there were differences between individuals utilizing inpatient and outpatient MAT services, a Chi-Square was conducted illustrating Suboxone use (yes or no), Vivitrol use (yes or no), and Program Value (inpatient or outpatient). The results indicated that there was a significant difference between Inpatient and Outpatient MAT service users (X2(36.53, N=475) = 1, p<.01). However, there were more outpatient (51.2% (n = 243) MAT service users than inpatient (48.8% (n = 232) MAT service users. Likewise, of the participants, 32.3% (n = 153) utilized Suboxone and were of outpatient services and, 42.5% (n = 202) utilized Suboxone in inpatient services. Relatedly, 18.9% (n = 90) utilized Vivitrol in an outpatient service and 6.3% (n = 30) used Vivitrol in an inpatient episode. See Figure 3 and Figure 4 for further information on the Chi-square distribution output of inpatient versus outpatient on Suboxone MAT services.
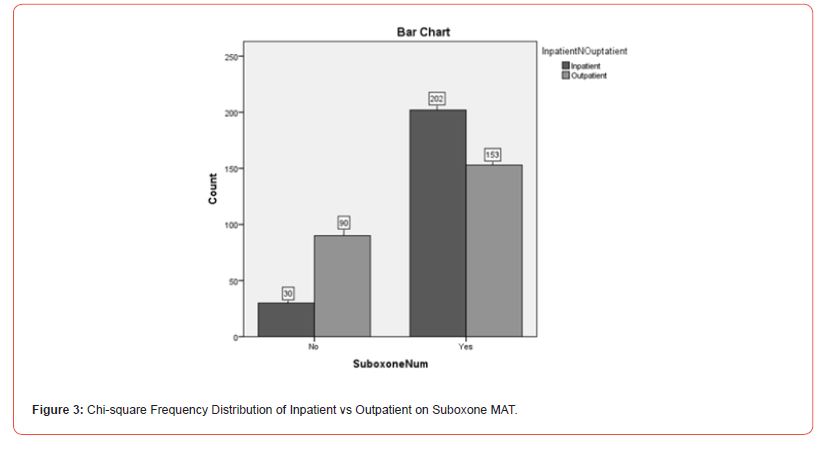

This information did not support the hypothesis that there would be more inpatient service enrollment than outpatient. When controlling for “Medical Services,” more outpatient service episodes utilized MAT services than individuals in inpatient episodes. Conversely, more individuals in inpatient episodes appeared to utilize Suboxone services than those in outpatient episodes.
MAT Service Differences Selection: To explore whether there were differences in Suboxone and Vivitrol use, a Chi-square analysis illustrating Suboxone use (yes or no) and Vivitrol use (yes or no) was conducted. The results indicated that there was a significant difference between Suboxone and Vivitrol users (X2(973, N=973) = 1, p<.01). Of the participants, 77% (n = 749) identified as having utilized Suboxone and 23% (n = 224) identified as using Vivitrol. See Figure 5 for further information on the Chi-square distribution output of Suboxone versus Vivitrol MAT services.
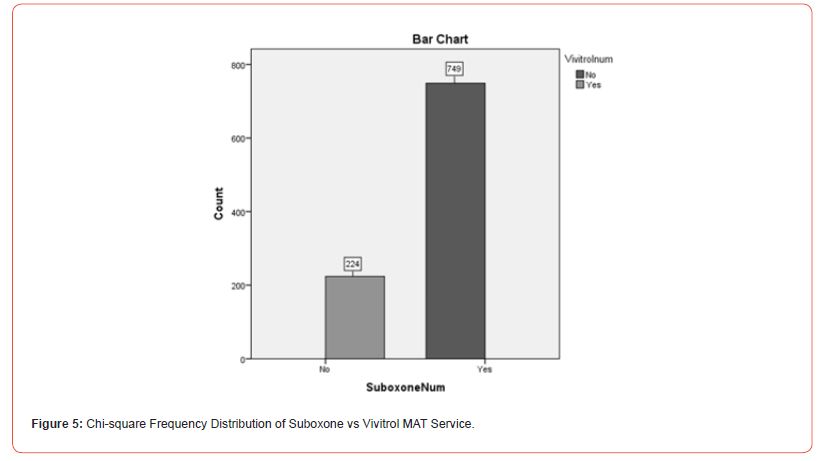
This information supported the hypothesis that there would be more Suboxone MAT enrollment than Vivitrol MAT enrollment related to cost differential. The process of enrolling into Suboxone appears to illustrate a preference for the substance when both Suboxone and Vivitrol are available. Factors such as costeffectiveness, the process of enrollment, and adherence are likely to play a part in selection of Suboxone to Vivitrol.
MAT Enrollment and Gender Differences: To explore whether there were differences in Suboxone and Vivitrol use related to gender differences, a Chi-square analysis illustrating Suboxone use (yes or no), Vivitrol use (yes or no), and Gender (male or female) was conducted. The results indicated that there was a significant difference (X2(14.72, N=973) = 1, p<.01) for Suboxone and Vivitrol use. Analyses indicated that 82.1% (n = 407) of Females and 71.7% (n = 342) of Males chose Suboxone MAT services. Likewise, 17.9% (n = 89) and 28.3% (n = 135) of Males chose Vivitrol MAT services. See Figure 6 and Figure 7 for further information on the Chi-square distribution output of Patients Gender on Suboxone and Vivitrol MAT services.
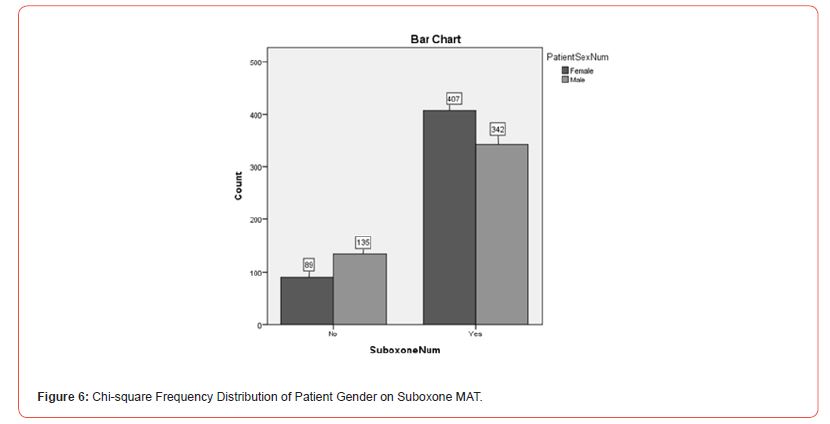
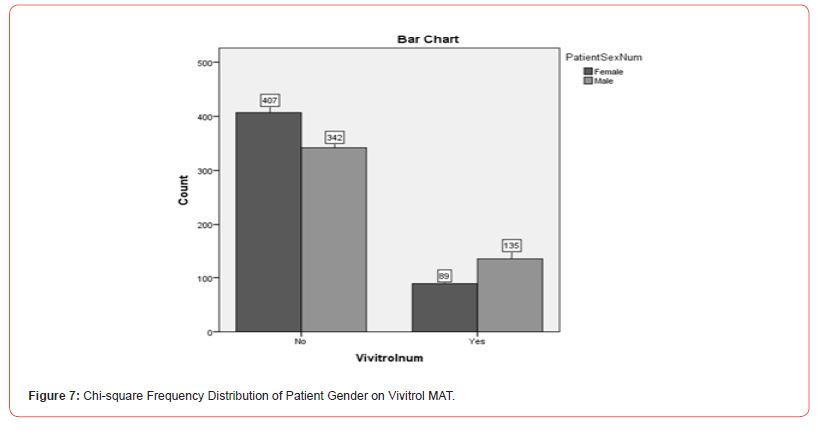
This information did not support the hypothesis that there was more female MAT treatment enrollment than male enrollment. It appears that more women were selecting Suboxone treatment for opioid use than men in this particular facility. Likewise, it is noted that although women outnumbered men, there were slightly more men selecting Vivitrol treatment enrollment compared to women.
Caucasian/White Male MAT Service Differences: To explore demographic differences with the assumption that Caucasian/ White Males being more expected to enroll in MAT services than Non-White Male demographic groups, a Chi-square analysis was utilized with Suboxone (yes or no), Vivitrol (yes or no), and White Male (yes or no) identifications. There was a significant difference (X2(6.988), N=973) = 1, p <.05). Of the participants, 42.3% (n = 412) identified as White Males, and 57.7% (n = 561) identifying as Non-White Male demographic standing. Of the White Males, 40.1% (n = 300) utilized Suboxone and 50.0% (n = 112) used Vivitrol. See Figure 8 and Figure 9 for further information on the Chi-square distribution output of White Male’s versus Non-White (Other Demographic Representatives) on Suboxone and Vivitrol MAT services.
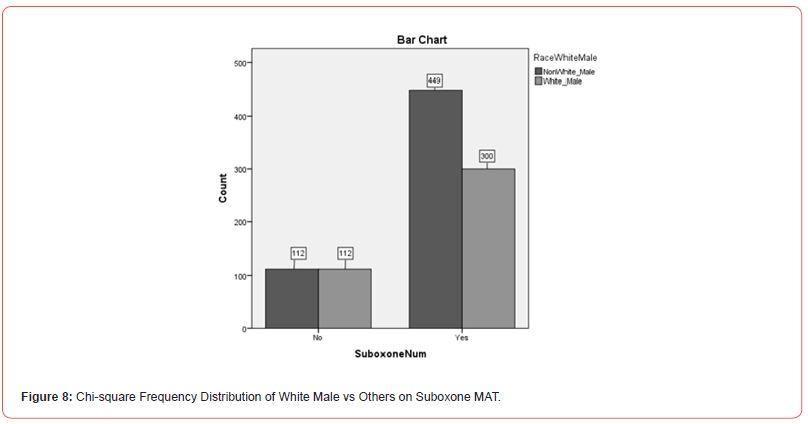
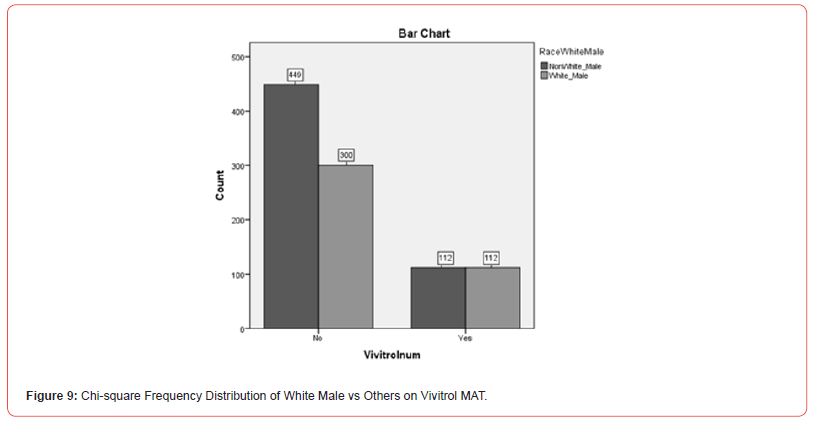
This information did not support the hypothesis that Caucasian/ White Males would be more likely to utilize MAT services than any other demographic group. Although they accounted for approximately 42% of the population, 45% of the population of individuals utilizing MAT services were Caucasian/White females. Likewise, neither group accounted for more than 50% of the population.
Employment Differences and MAT services: To explore employment differences and utilization of MAT services, a Chi- Square analysis illustrating Suboxone (yes or no), Vivitrol (yes or no), and Employment (employed vs. not employed) was conducted. There was not a significant difference (X2(.866, N=973) = 1, p >.05). Unemployed individuals accounted for 69.5% (n = 676) and Employed individuals accounted for 30.5% (n = 297). Unemployed individuals utilizing Suboxone were 70.2% (n = 526) of the population, and employed individuals using Suboxone were 29.8% (n = 223). Of the individuals using Vivitrol, 67% (n = 150) were unemployed, and 33% (n = 74) were employed. See Figure 10 and Figure 11 for further information on the Chi-square distribution output of Employed versus Unemployed on Suboxone and Vivitrol MAT services.
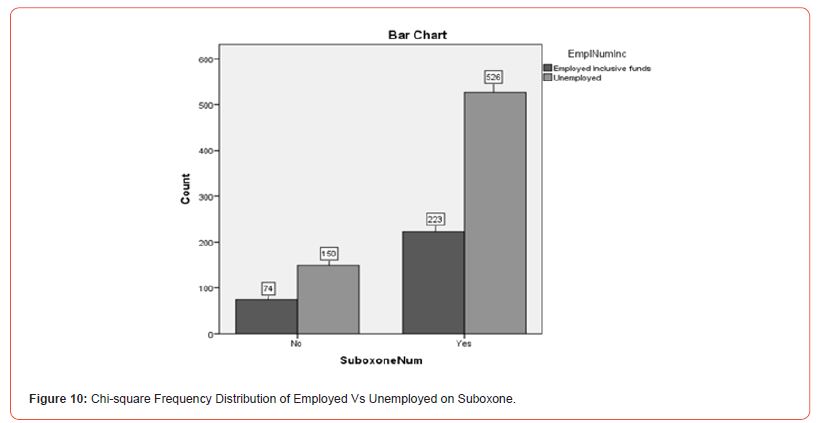

This information did not support the hypothesis that employed individuals will be more likely to be admitted to MAT programs. Unemployed individuals outnumber employed individuals, which illustrates that employment is not predictive of enrollment to the programs.
Educational Attainment, Employment, and MAT Service Differences: To explore differences between MAT services and Higher Educational attainment, a Chi-square analysis was conducted. To illustrate this distinction, analyses of Suboxone (yes or no), Vivitrol (yes or no), and Education (Higher Education or High School Diploma and Those Having Less Than a High School Diploma) were conducted. The results indicated that there were statistical differences as it relates to education and MAT services (X2(20.02), N=973) = 1, p <.01). Suboxone users without higher education accounted for 51.5% (n = 501) and with higher education accounted for 25.5% (n = 248). Vivitrol users without higher education accounted for 11.6% (n = 113), and with higher education accounted for 11.4% (n = 111) of the total population. See Figure 12 and Figure 13 for further information on the Chisquare distribution output of Higher Education versus High School Diploma and Less on Suboxone and Vivitrol MAT services.

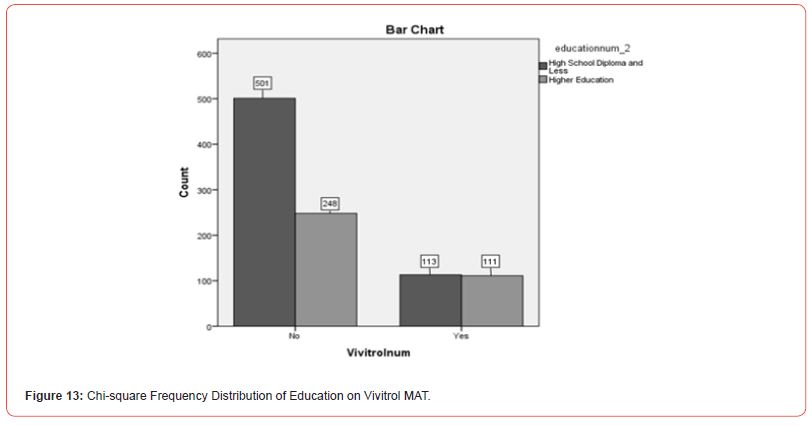
An Analysis of Variance (ANOVA) test was run to explore how higher educational attainment affects individuals’ likelihood of enrollment to MAT services programs as it relates to employment status. This ANOVA test was used to illustrate variance amongst variables such as Suboxone (yes or no), Vivitrol (yes or no), Employment (employed or unemployed), and Education (interval clustering). There was no significant effect of educational attainment on employment [F (5,967) =.721, p=.608].
There was, however, a significant effect of Suboxone and Vivitrol use on educational attainment at the interval clustering level. [F (5,967) = 11.41, p< .01]. A Tukey Post Hoc test indicated that Suboxone (M =.77, SD=.421), Vivitrol (M =.23, SD=.421), and Education attainment (M =3.85, SD=1.58) were statistically significant at the College Degree comparison relative to other educational identification such as 5th to 8th grade (p<.01), 9th to 12th grade, no diploma (p<.01), High School Graduate/Diploma/ Degree (p<.01) and Some College, No Degree (p<.01). However, there was no statically significant difference between College Degree and Vocational/Trade (p=.65). Therefore, obtaining a college degree and engaging in Suboxone or Vivitrol treatment did not happen by chance and having post-secondary education made a difference.
Discussion
Impact of Study
Over the past decades, Opioid Use Disorder has continuously been a global epidemic and public health problem. The call for proper treatment and access to care has been sharply increasing as the mortality rates of opioid-related deaths also increase [81]. The utilization of MAT services has been explored to combat those deaths. Despite national data projections of the prevalence of OUDs surpassing approximately 5 million and growing in the United States, only a fraction of the population received MAT treatment services in the past ten years [82,83]. The engagement of this study explored the population that uses MAT services to understand better the trajectory of use, enrollment, and program-related functionality. It also provided indications for populations that are still needing to receive access to care.
The inpatient and outpatient hypothesis indicated that individuals in outpatient treatment settings are more likely to engage in MAT services than in inpatient settings. Some have suggested that the benefits to inpatient services such as medically supervised withdrawal from substances, removal of outside influences, psychosocial support, and continued monitoring would reduce relapse potential [69]. However, it is noted that facilities use short inpatient treatment stays, and often facilities rarely distinguish between patients who receive medications in inpatient or outpatient services because they fall under an umbrella of care. Nonetheless, facilities could increase their prescribing rate by identifying needed services for inpatient and outpatient individuals, including linkage to follow-up services and medication management [84]. In order to gain more clarity in the distinction of inpatient and outpatient services, more defined identification and coding should be used to assist with assessing unmet program needs.
Next, the results indicated that there were more Suboxone MAT service users than Vivitrol service users. The distinction between the two substances was made and able to be readily identified. Fifty participants illustrated the use of both, meaning that they engaged in both of the substances at one point in their treatment trajectory. The participants were removed to ensure that the data would be correctly observed. However, the results indicated a significant difference between the two, with approximately 77% being Suboxone MAT users, and therefore, the 50 participants were not likely to affect the results in general. This information was predicted relative to the literature on selecting services and benefits for engaging in both services. Explored reasons are related to the idea that Vivitrol discontinuation rates appear to be higher in the first injection related to cost, insurance, and retention rates, compared to Suboxone use, which also deters desirability of MAT by patients [45]. Likewise, other rationale includes the administration structure of Suboxone, the candidacy for office-based treatment pathways, and reduction of the high need for strict adherence to medication management compared to Vivitrol [85]. These similar benefits are likely reasons for exploration in the GCS, but further research would be beneficial to explore as both treatments have proved effective.
Relative to demographic hypotheses, gender differences were explored. Women represented more of the MAT population service use than men. The literature supports the idea that men were more likely to engage in all MAT services and more likely to engage in MAT service trials and research which represented a possible bias in the literature [86]. A vital notation to be made is that men were selecting Vivitrol treatment options more than women, even though they were outnumbered as a whole. Vivitrol treatment has been proven to be well-tolerated by pregnant women who choose to detoxify off opioid drugs during gestation completely, which tends to be opposed by most women [87]. Although pregnancy was not asked of participants, future studies would benefit from inclusion of this criteria to illuminate the impact of pregnancy as it relates to the preference for Vivitrol treatment. There was also a declared need for more women involvement in MAT services in general, especially considering the high rate of pregnant women with OUDs [88]. Relatedly, GCS has a program dedicated to pregnant women and substance use but is also engaged in child welfare services and drug court, which could have accounted for the higher engagement rate of women in the MAT services. Further analysis would have to be conducted to illustrate and assess a possible link of related episodes of care to women’s exploration of MAT services. Further research should also be explored on the use of MAT services by women related to social functioning, psychological symptoms, treatment barriers, and gender differences [89].
Additionally, racial differences were explored. Caucasian men were projected to use MAT services more than any other demographic group. Although Caucasian men accounted for a high percentage of the population, they did not account for a statistically significant portion of the individuals that sought MAT services at GCS. It is important to note that Caucasian men and women accounted for approximately 87 percent of the total population of individuals in MAT services. This information does correlate with literature in that White individuals are more likely to utilize MAT services even though these services have been proven to be beneficial to other demographic populations [90]. Additional studies should be conducted to explore the racial disparities to reduce the racial gap of individuals engaging in these OUD treatment services.
Further, employment differences were explored in this research. Individuals employed did not account for a significant portion of the population of those in MAT services. This information represents that employment is not indicative of enrollment in the program. It would be advantageous to explore the additional rationale for engagement in the programs related to cost such as insurance and private pay instead of employment rates. This detailed information was not collected in the study, which would be beneficial to analyze in correlation. Likewise, literature exploring employment acknowledges that treatment duration and engagement is not impacted by employment [91,92,89]. However, older age increases the odds for employment, associations between unemployment and poorer health outcomes have been well-studied, and women tend to report being unemployed more than men in MAT services. Therefore, with consideration to these factors for future studies, the outcome would likely be more salient with the literature. Likewise, future literature should be explored to understand further how MAT services such as selecting various MAT substances correlate with continued employment and job maintenance.
Related to employment demographic information, educational attainment and MAT services were explored. There was no significant effect of employment on educational attainment, according to the results of this study. MAT services on education attainment relative to levels of education were significantly affected where individuals illustrating higher education achievement and college degree achievement showed a significant difference in choosing to engage in MAT services. The literature supports the idea that individuals with higher education, precisely a graduate degree, likely had more positive attitudes towards MAT services such as Vivitrol use [93]. The literature also supported the idea that employed individuals or students were nearly 2.5 times more likely to graduate in drug court-related programs than individuals who were not [94]. Likewise, offering MAT services to those employed or educated individuals was projected to improve graduation rates for drug courts. Although these results were indicated, there are still many individuals who do not seek higher education and engage in MAT services. Future research should explore the inter-correlation of employment and education on MAT services. Research should also be geared towards understanding if higher education is a factor for individuals in the programs and ways to provide increased education for those interested but hesitant due to lack of awareness.
Limitations and Areas for Future Study
The first significant limitation was the inability to distinguish between inpatient and outpatient services that have affected the first hypothesis test. Although “medical services” was able to be controlled with the idea that there was an equal distribution of the patients in the episode, it would have been preferred to make the distinction that could account for both inpatient and outpatient services more seamlessly. This information would be beneficial to establishing the relationship between the individuals that used Suboxone and Vivitrol and placement in the programs. Future research should focus on how programs effectively make this distinction to account for the services that are working well for individuals in MAT services.
Additionally, there was minimal information for how many times an individual’s service count (the number of services an individual received) was presented and an inability to have a direct indicator for follow-up for a year or more after completing the episode. This information means that there is no way to evaluate whether or not the individual checked into another treatment facility, is since deceased, or relapsed and did not return to the facility. This difficulty is the same for individuals that leave the Vivitrol or Suboxone program. Having the information for these episodes of care and the timeline of the individuals’ treatment would allow for additional information that gives a better understanding of the completion of care and likely barriers to completion of care.
Another limitation is related to the fact that the study was specific to one treatment facility and cannot account for the statistics; however, the attempt of using such a large sample size was to be able to generalize to more demographics. Also, connecting with other treatment facilities to evaluate their use of data collection and treatment forms would allow for more generalizability.
Conclusion
In conclusion, to acknowledge the public health difficulty of opioid use disorder, the likelihood of enrollment into MAT services was explored. The research concluded that more outpatient serviced individuals have used MAT services than their inpatient counterparts. In comparison to one another, Suboxone treatment is still being utilized more than Vivitrol treatment. Demographic information explored that more women than men have been using MAT services. Furthermore, individuals that have obtained degrees greater than a high school diploma represent a significant population of note for MAT services as well. Likewise, employment does not have an acknowledged effect on engaging in MAT services despite education being a qualifying factor. However, without follow-up data for the individuals’ that completed services, such as a survey tracking their current standing or use of MAT, it is not possible to identify what path the individuals’ took after completing the episode of care or current enrollment in treatment. Likewise, using additional treatment facilities and a direct clarification of episodes of care would be beneficial to further assessment of the route of the individuals in the programs.
In order to prevent relapse, assess for improvements, and sustain recidivism, all of the limitations must be addressed. It is important to educate the staff as well as the individuals receiving treatment, to continue to understand their rights and the benefits of maintaining sobriety. By increasing awareness of the options for individuals with opioid related substance use disorders, there could be a decrease in the number of lives claimed by this opioid epidemic. Future research should be geared towards addressing the demographic related issues, limitations, and comparison of other treatment facilities to identify and attend to barriers to treatment.
Conflict of interest
None.
Acknowledgment
None.
References
- Musto D F (1996) Drug abuse research in historical perspective. Committee on Opportunities in Drug Abuse Research, Editor. Pathways of addiction: opportunities in drug abuse research: 284-94.
- Ritchie H, Roser M (2019) Drug use. Our World in Data.
- GBD 2017 Risk Factor Collaborators (2018) Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159): 1923-1994.
- Guerrero E G, Marsh J C, Duan L, Oh C, Perron B, et al. (2013) Disparities in completion of substance abuse treatment between and within racial and ethnic groups. Health services research 48(4): 1450-1467.
- Saloner B, Cook B L (2013) Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health affairs 32(1): 135-145.
- Maglione M A, Raaen L, Chen C, Azhar G, Shahidinia N, et al. (2018). Effects of medication assisted treatment (MAT) for Opioid Use Disorder on functional outcomes: a systematic review. Journal of substance abuse treatment 89: 28-51.
- CDC Coordination C (2018) Implementing the CDC Guideline for Prescribing Opioids for Chronic Pain.
- Świeboda P, Filip R, Prystupa A, Drozd M (2013) Assessment of pain: types, mechanism and treatment. Pain 1: 2-7.
- McCance-Katz E F (2018) SAMHSA/HHS: an update on the opioid crisis. Substance Abuse and Mental Health Services Administration.
- NIDA (2020) Prescription opioids and heroin have similar effects, different risk factors.
- NIDA (2020) How effective are medications to treat opioid use disorder?.
- Jones C M, Campopiano M, Baldwin G, McCance-Katz E (2015) National and State Treatment Need and Capacity for Opioid Agonist Medication-Assisted Treatment. American journal of public health 105(8): e55-e63.
- Meldrum M L (2003) A capsule history of pain management. Jama 290(18): 2470-2475.
- Stern A (2005) Sterilized: In the Name of Public Health. American Journal of Public Health 95(7): 1128-1138.
- Meldrum M L (2003) Opioids and pain relief: a historical perspective.
- Kentucky Educational Television (2017) Lexington’s Narcotic Farm: A Pioneering Institution in Drug Treatment.
- Campbell J N (1996) APS 1995 presidential address. In Pain Forum 5(1): 85-88.
- WHO (1986) Cancer pain relief. Geneva: WHO.
- Tucker J D, Kathryn L (2004) Medico-Legal Case Report and Commentary: Inadequate Pain Management in the Context of Terminal Cancer-The Case of Lester Tomlinson. Pain Medicine: 5(2).
- Morales K B, Park J N, Glick J L, Rouhani S, Green T C, et al. (2019) Preference for drugs containing fentanyl from a cross-sectional survey of people who use illicit opioids in three United States cities. Drug and alcohol dependence 204: 107547.
- National Institute on Drug Abuse (2018) DrugFacts: Comorbidity: Substance Use Disorders and Other Mental Illnesses.
- National Institute on Drug Abuse (2018) Drugs, Brains, and Behavior: The Science of Addiction: Treatment and Recovery.
- National Institute on Drug Abuse (2019) DrugFacts: Treatment Approaches for Drug Addiction.
- National Institute on Drug Abuse (2018) Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition): Types of Treatment Programs.
- NIDA (2020) Drug Addiction Treatment in the United States.
- McCarty D, Braude L, Lyman D R, Dougherty R H, Daniels A S, et al. (2014). Substance abuse intensive outpatient programs: assessing the evidence. Psychiatric Services 65(6): 718-726.
- Rasmussen S (2000) Addiction treatment: Theory and practice. Sage.
- Steps T (1981) Twelve steps and twelve traditions. New York, NY: Alcoholics Anonymous World Services.
- Timko C, DeBenedetti A, Billow R (2006) Intensive referral to 12‐Step self‐help groups and 6‐month substance use disorder outcomes. Addiction 101(5): 678-688.
- Groh D R, Jason L A, Keys C B (2008) Social network variables in alcoholics anonymous: A literature review. Clinical psychology review 28(3): 430-450.
- Rynes K N, Tonigan J S (2012) Do social networks explain 12-step sponsorship effects? A prospective lagged mediation analysis. Psychology of Addictive Behaviors 26(3): 432-439.
- Gallagher J R, Wahler E A (2018) Racial disparities in drug court graduation rates: The role of recovery support groups and environments. Journal of Social Work Practice in the Addictions 18(2): 113-127.
- Gallagher J R (2013) African American participants’ views on racial disparities in drug court outcomes. Journal of Social Work Practice in the Addictions 13(2): 143-162.
- Dervan L A, Yaghmai B, Watson R S, Wolf F M (2017) The use of methadone to facilitate opioid weaning in pediatric critical care patients: a systematic review of the literature and meta‐analysis. Pediatric Anesthesia 27(3): 228-239.
- Lewis J W (1985) Buprenorphine. Drug and alcohol dependence 14(3-4): 363-372.
- Johnson R E, Fudala P J, Payne R (2005) Buprenorphine: considerations for pain management. Journal of pain and symptom management 29(3): 297-326.
- Johnson R E, Strain E C, Amass L (2003) Buprenorphine: how to use it right. Drug and alcohol dependence 70(2): S59-S77.
- Robinson G M, Dukes P D, Robinson B J, Cooke R R, Mahoney G N (1993) The misuse of buprenorphine and a buprenorphine-naloxone combination in Wellington, New Zealand. Drug and alcohol dependence: 33(1): 81-86.
- Lintzeris N, Leung S Y, Dunlop A J, Larance B, White N, et al. (2013) A randomized controlled trial of sublingual buprenorphine–naloxone film versus tablets in the management of opioid dependence. Drug and alcohol dependence 131(1-2): 119-126.
- Gonzalez J P, Brogden R N (1988) Naltrexone. Drugs 35(3): 192-213.
- Sawicka M, Tracy D K (2017) Naltrexone efficacy in treating alcohol-use disorder in individuals with comorbid psychosis: a systematic review. Therapeutic advances in psychopharmacology 7(8-9): 211-224.
- Volpicelli J R, Rhines K C, Rhines J S, Volpicelli L A, Alterman A I, et al. (1997) Naltrexone and alcohol dependence: role of subject compliance. Archives of General Psychiatry 54(8): 737-742.
- Volpicelli J R, Alterman A I, Hayashida M, O'Brien C P (1992) Naltrexone in the treatment of alcohol dependence. Archives of general psychiatry 49(11): 876-880.
- Krupitsky E, Nunes E V, Ling W, Illeperuma A, Gastfriend D R, et al. (2011) Injectable extended-release naltrexone for opioid dependence: a double-blind, placebo-controlled, multicentre randomised trial. The Lancet 377(9776): 1506-1513.
- Morgan J R, Schackman B R, Leff J A, Linas B P, Walley A Y (2018) Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for Opioid Use Disorder in a United States commercially insured population. Journal of substance abuse treatment 85: 90-96.
- Johansson B A, Berglund M, Lindgren A (2006) Efficacy of maintenance treatment with naltrexone for opioid dependence: a meta‐analytical review. Addiction 101(4): 491-503.
- Syed Y Y, Keating G M (2013) Extended-release intramuscular naltrexone (VIVITROL®): a review of its use in the prevention of relapse to opioid dependence in detoxified patients. CNS drugs 27(10): 851-861.
- VIVITROL S, TREAT W T VIVITROL Treatment. (n.d.)
- Rieckmann T, Garvey K T, Srikanth P, Andrich L, Gregg J (2015) The Vivitrol pilot program (VPP): initial quantitative findings from an extended-release naltrexone study. In Addiction Science & Clinical Practice 10(S1): A54.
- Knopf A (2018) Buprenorphine better than Vivitrol in cost‐effectiveness study. Alcoholism & Drug Abuse Weekly, 30(48): 1-4.
- Lee J D, Nunes Jr E V, Novo P, Bachrach K, Bailey G L, et al. (2018) Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X: BOT): a multicentre, open-label, randomised controlled trial. The Lancet 391(10118): 309-318.
- Knopf A (2019) Patients report Vivitrol decreasing in effectiveness by week 3. Alcoholism & Drug Abuse Weekly 31(23): 4-5.
- Binswanger I A, Glanz J M (2018) Potential risk window for opioid overdose related to treatment with extended-release injectable naltrexone. Drug safety 41(10): 979-980.
- Cicero T J, Ellis M S, Surratt H L, Kurtz S P (2014) Factors contributing to the rise of buprenorphine misuse: 2008–2013. Drug and alcohol dependence 142: 98-104.
- Bazazi A R, Yokell M, Fu J J, Rich J D, Zaller N D (2011) Illicit use of buprenorphine/naloxone among injecting and noninjecting opioid users. Journal of Addiction Medicine 5(3): 175-180.
- Ferrant O, Papin F, Clin B, Lacroix C, Saussereau E., et al. (2011) Fatal poisoning due to snorting buprenorphine and alcohol consumption. Forensic science international 204(1-3): e8-e11.
- Murphy S M, Polsky D, Lee J D, Friedmann P D, Kinlock T W, et al. (2017) Cost‐effectiveness of extended-release naltrexone to prevent relapse among criminal justice‐involved individuals with a history of Opioid Use Disorder. Addiction 112(8): 1440-1450.
- Jackson H, Mandell K, Johnson K, Chatterjee D, Vanness D J (2015) Cost-effectiveness of injectable extended-release naltrexone compared with methadone maintenance and buprenorphine maintenance treatment for opioid dependence. Substance abuse 36(2): 226-231.
- Andraka-Christou B, Capone M J (2018) A qualitative study comparing physician-reported barriers to treating addiction using buprenorphine and extended-release naltrexone in US office-based practices. International Journal of Drug Policy 54: 9-17.
- Nguyen T, Andraka-Christou B, Simon K, Bradford W D (2019) Provider-directed marketing may increase prescribing of medications for Opioid Use Disorder. Journal of substance abuse treatment 104: 104-115.
- Goedel W C, Shapiro A, Cerdá M, Tsai J W, Hadland S E, et al. (2020) Association of racial/ethnic segregation with treatment capacity for Opioid Use Disorder in counties in the United States. JAMA network open 3(4): e203711-e203711.
- Amiri S, McDonell M G, Denney J T, Buchwald D, Amram O (2020) Disparities in access to opioid treatment programs and office-based buprenorphine treatment across the rural-urban and area deprivation continua: a US nationwide small area analysis. Value in Health 24(2): 188-195.
- Cioe K, Biondi B E, Easly R, Simard A, Zlheng X, et al. (2020) A systematic review of patients’ and providers’ perspectives of medications for treatment of Opioid Use Disorder. Journal of Substance Abuse Treatment 108146.
- Rudd R A, Seth P, David F, Scholl L (2016) Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Morbidity and mortality weekly report 65(50-51): 1445-1452.
- Cicero T J, Ellis M S, Surratt H L, Kurtz S P (2014) The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA psychiatry 71(7): 821-826.
- Mattick R P, Breen C, Kimber J, Davoli M (2014) Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane database of systematic reviews (2): CD002207.
- Day E, Strang J (2011) Outpatient versus inpatient opioid detoxification: a randomized controlled trial. Journal of Substance Abuse Treatment 40(1): 56-66.
- Day E (2005) Opiate detoxification in an inpatient setting. National Treatment Agency.
- Nunes E V, Gordon M, Friedmann P D, Fishman M J, Lee J D, et al. (2018). Relapse to Opioid Use Disorder after inpatient treatment: Protective effect of injection naltrexone. Journal of substance abuse treatment 85: 49-55.
- Marsh J C, Cao D, D’Aunno T (2004) Gender differences in the impact of comprehensive services in substance abuse treatment. Journal of Substance Abuse Treatment 27(4): 289-300.
- Chen L Y, Strain E C, Crum R M, Mojtabai R (2013) Gender differences in substance abuse treatment and barriers to care among persons with substance use disorders with and without comorbid major depression. Journal of addiction medicine 7(5): 325.
- McElrath K (2018) Medication-assisted treatment for opioid addiction in the United States: critique and commentary. Substance use & misuse 53(2): 334-343.
- Alegria M, Carson N J, Goncalves M, Keefe K (2011) Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. Journal of the american academy of Child & adolescent Psychiatry 50(1): 22-31.
- Pro G, Utter J, Haberstroh S, Baldwin J A (2020) Dual mental health diagnoses predict the receipt of medication-assisted opioid treatment: Associations moderated by state Medicaid expansion status, race/ethnicity and gender, and year. Drug and alcohol dependence 209: 107952.
- Colby S, Ortman J M (2015). Projections of the size and composition of the US population: 2014 to 2060.
- Wu L T, Zhu H, Swartz M S (2016) Treatment utilization among persons with Opioid Use Disorder in the United States. Drug and alcohol dependence 169: 117-127.
- Ali M M, Teich J L, Mutter R (2017) Reasons for not seeking substance use disorder treatment: variations by health insurance coverage. The journal of behavioral health services & research 44(1): 63-74.
- Buck J A (2011) The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Affairs 30(8): 1402-1410.
- Andrews C M, Pollack H A, Abraham A J, Grogan C M, Bersamira C S, et al. (2019) Medicaid coverage in substance use disorder treatment after the Affordable Care Act. Journal of substance abuse treatment 102: 1-7.
- Ho J Y (2017) The contribution of drug overdose to educational gradients in life expectancy in the United States, 1992–2011. Demography 54(3): 1175-1202.
- Jun Ma, Yan-Ping Bao, Ru-Jia Wang, Meng-Fan Su, Mo-Xuan Liu, et al. (2019) Effects of medication-assisted treatment on mortality among opioids users: a systematic review and meta-analysis. Mol Psychiatry 24: 1868-1883.
- Zheng W, Nickasch M, Lander L, Wen S, Xiao M, et al. (2017) Treatment outcome comparison between telepsychiatry and face-to-face buprenorphine Medication-Assisted Treatment (MAT) for opioid use disorder: a 2-year retrospective data analysis. Journal of addiction medicine 11(2): 138.
- Andrilla C H A, Patterson D G, Moore T E, Coulthard C, Larson E H (2020) Projected contributions of nurse practitioners and physician’s assistant to buprenorphine treatment services for opioid use Disorder in rural areas. Medical Care Research and Review 77(2): 208-216.
- Hagedorn H, Kenny M, Gordon A J, Ackland P E, Noorbaloochi S, et al. (2018) Advancing pharmacological treatments for opioid use disorder (ADaPT-OUD): protocol for testing a novel strategy to improve implementation of medication-assisted treatment for veterans with opioid use disorders in low-performing facilities. Addiction science & clinical practice 13(1): 25.
- Tran T H, Griffin B L, Stone R H, Vest K M, Todd T J (2017) Methadone, buprenorphine, and naltrexone for the treatment of opioid use disorder in pregnant women. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy 37(7): 824-839.
- Ling S, Mangaoil R, Cleverley K, Sproule B, Puts M (2019) A systematic review of sex differences in treatment outcomes among people with opioid use disorder receiving buprenorphine maintenance versus other treatment conditions. Drug and alcohol dependence 197: 168-182.
- Towers C V, Katz E, Weitz B, Visconti K (2020) Use of naltrexone in treating opioid use disorder in pregnancy. American journal of obstetrics and gynecology 222(1): 83.e1-83. e8.
- Krans E E, Kim J Y, James III A E, Kelley D, Jarlenski M P (2019) Medication-Assisted Treatment Utilization Among Pregnant Women With Opioid Use Disorder. Obstetrics and gynecology 133(5): 943-945.
- Van Reekum E A, Rosic T, Hudson J, Sanger N, Marsh D C, et al. (2020) Social functioning outcomes in men and women receiving medication-assisted treatment for opioid use disorder. Biology of sex differences 11(1): 20.
- Stahler G J, Mennis J, Baron D A (2021) Racial/Ethnic Disparities in the Use of Medications for Opioid Use Disorder (MOUD) and Their Effects on Residential Drug Treatment Outcomes in the US. Drug and Alcohol Dependence 226: 108849.
- Brydsten A, Hammarström A, San Sebastian M (2018) Health inequalities between employed and unemployed in northern Sweden: a decomposition analysis of social determinants for mental health. International Journal for Equity in Health 17(1): 59.
- McBrien H, Luo C, Sanger N, Zielinski, Bhatt M, et al. (2019). Cannabis use during methadone maintenance treatment for opioid use disorder: a systematic review and meta-analysis. CMAJ open 7(4): E665.
- Andraka-Christou B, Gabriel M, Madeira J, Silverman R D (2019) Court personnel attitudes towards medication-assisted treatment: A state-wide survey. Journal of substance abuse treatment 104: 72-82.
- Gallagher J R, Wahler E A, Lefebvre E, Paiano T, Carlton J, et al. (2018) Improving graduation rates in drug court through employment and schooling opportunities and medication-assisted treatment (MAT). Journal of Social Service Research 44(3): 343-349.
-
Patrick J Aragon* and Antwana L Drayton. Medication Assisted Treatment: Examining Enrollment and Demographic Factors of Treatment. Curr Tr Clin & Med Sci. 3(4): 2023. CTCMS.MS.ID.000570.
-
Opioid Use Disorder (OUD), Mental Health, Pain, Detoxification, Buprenorphine, Suboxone, psychotherapy
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






