 Mini Review
Mini Review
Knowledge Gaps of The Morbidity and Mortality of COVID-19: Testosterone & Sex Differences
Aksam Yassin1,2* and Bassam Albaba1
1Dresden International University, Dresden, Germany
2Weill Cornell Medical School, Urology, New York, USA
Aksam Yassin, Dresden International University, Centre of Medicine and Health Sciences, Prevetion, Germany.
Received Date: February 21, 2023 Published Date: March 02, 2023
Introduction
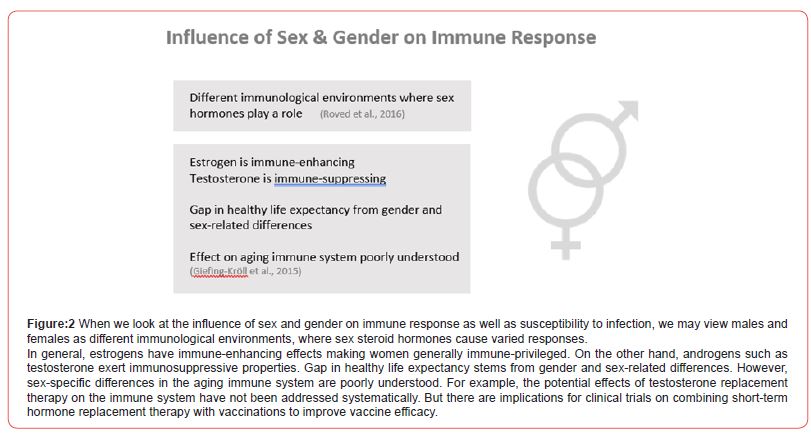
The current COVID‐19 pandemic has a male bias in morbidity/ severity and mortality. This is consistent with previous coronavirus pandemics such as SARS‐ CoV and MERS‐CoV, and viral infections in general (Figure 1). Data from previous coronavirus epidemics‐ SARS‐CoV (2002) and Middle Eastern respiratory syndrome coronavirus (MERS, 2012) showed differences in their manifestation based on sex, with men being consistently more severely affected than women. Reports of COVID‐19 suggest a sex imbalance, with men at a higher risk of more severe disease and increased mortality (Figure 2).

Publicly available data from the Global Health 50/50 research initiative showed an increased mortality in men, despite similar numbers of COVID‐19 cases in men and women. In addition to mortality, hospitalizations and admissions to intensive care units (ICU) showed men more affected than women (Figure 3). A review of data in several countries showed that there were 50% more men requiring hospitalization compared to women, with ICU admission being three to fourfold higher. A meta‐analysis of 15 independent studies found men had an odds ratio of 1.31 to develop a severe COVID‐19 infection compared to women. Early reports by the Centers for Disease Control and Prevention (CDC) observed higher hospitalization rates for men (Figure 4).
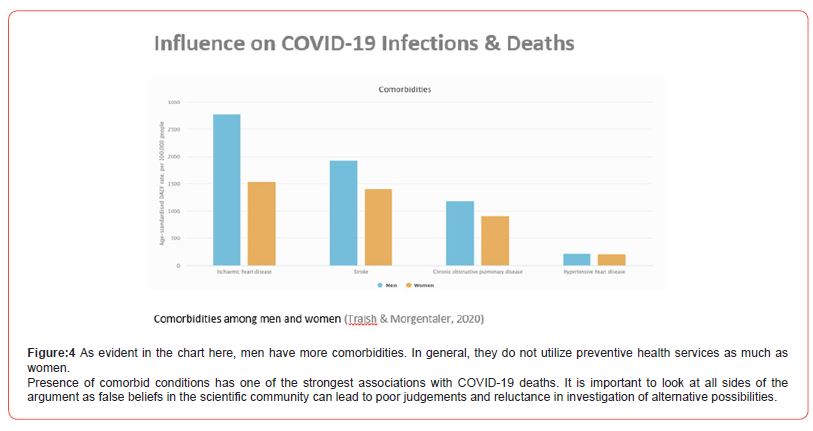
There are, however, some limitations to this data particularly as the interaction between age and sex remains unclear. It was reported that the relative risk of dying from COVID‐19 was consistently elevated in men across all age groups with the differences increasing until the age range 60-69 years. Thereafter, the sex difference in survival decreases and was at its lowest for ages ≥80. The sex disparities in COVID‐19 morbidity and mortality are multifactorial. They may potentially be caused by the sexdifferences in comorbidities, behaviors and hormonal influences. There is a need to collect sex and age‐disaggregated data to better understand disease pathology, study the sex differences and guide clinical care. Furthermore, the consistencies with previous coronavirus pandemics may suggest that the public health policies and risk stratification should take sex into consideration for future pandemics. Moreover, more research is needed to clarify inflammatory and immunity disparities to close some knowledge gaps in these concerns (Figures 5 & 6).
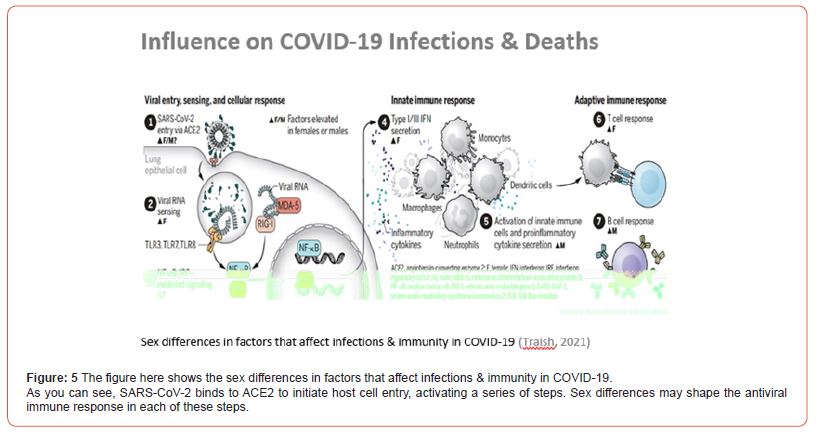
There is overwhelming evidence to suggest that male gender is at a higher risk of developing more severe Covid‐19 disease and thus having poorer clinical outcomes. However, the relationship between testosterone (T) and Covid‐19 remains unclear with both protective and deleterious effects on different aspects of the disease suggested. Here, we review the current epidemiological and biological evidence on the role of testosterone in the process of SARS‐CoV‐2 infection and in mediating Covid‐19 severity, its potential to serve as a biomarker for risk stratification and discuss the possibility of T supplementation as a treatment or preventative therapy (Figure 7).
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Yassin A, Sabsigh R, Al‐Zoubi R, Aboumarzouk OM, Alwan M, et al. (2023) Testosterone and Covid‐19: An update, Review. Rev Med Virol 33(1): e2395.
- Alwani M, Yassin A, Al‐Zoub R, Aboumarzouk OM, Nettleship J, et al. (2021) Sex‐based differences in severity and mortality in COVID‐19. Rev Med Virol 31(6): e2223.
- Ridwan Shabsigh (2022) Health Crisis Management in Acute Care Hospitals (Book). SBH Health System & Weill Conell Medical College.
- Batiha O, Al-Deeb T, Al-Zoubi E, Alsharu E (2020) Impact of COVID-19 and other viruses on reproductive health. Andrologia, 52(9): e13791.
- Giefing-Kröll C, Berger P, Lepperdinger G, Grubeck-Loebenstein B (2015) How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell 14(3): 309-321.
- Roved J, Westerdahl H, Hasselquist D (2017) Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Hormones and Behaviour 88: 95-105.
- Traish A, Morgentaler A (2020) What’s testosterone got to do with it? A critical assessment of the contribution of testosterone to gender disparities in COVID-19 infections and deaths. Androgens: Clinical Research and Therapeutics 2(1): 18-35.
- Traish A (2021) Sex steroids in COVID-19 mortality in women. Trends in Endocrinology & Metabolism 32(8): 533-536.
-
Aksam Yassin* and Bassam Albaba. Knowledge Gaps of The Morbidity and Mortality of COVID-19: Testosterone & Sex Differences. Curr Tr Clin & Med Sci. 3(3): 2023. CTCMS.MS.ID.000563.
-
Intensive care units, Sex‐differences, Pathology, Preventative therapy, Testosterone, Sex imbalance, Hormonal influences, Coronavirus
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






