 Research Article
Research Article
An Empirical Evaluation on The Transmissions of Healthcare Associated Infections in Healthcare Structures in Piedmont Region
Cauli Alessandra, Polytechnic of Turin, Corso Duca degli Abruzzi 24,
Received Date: June 04, 2024; Published Date: June 25, 2024
Abstract
This report examined a population of data extracted in RedCap framework whom population of 174 inpatients from AOU S. Luigi in Orbassano (Turin) was the first eligible as statistical surveillance review of clinical data during the study period of seven months. Then, we selected 371 susceptible individuals from two wards of Gradenigo Hospital in Turin that we consider as an unicenter cohort of intensive care units. Some data indicate the possibility to measure the multi-resistance of the overall population of clinical inpatients while infectious statistical population of individuals draw a prospective scenario for future patients in the same conditions and for future audience segmentation of more populations of individuals evaluating the knowledge of healthcare structure in Piedmont Region from real data, reordered in RedCap they were processed in R Studio. Principal risk factors measured for explaining how age, length of stay, prescribed proton-pump inhibitor and prescribed antibiotic influenced Healthcare Associated Infection rate.
Keywords: Local health costs; HAIs, empirical process; nosocomial immunocompromised patients; community-acquired infectious patients; survival analysis; carbapenem resistant enterobacteria; pathogenicity; R Studio; Minitab, RedCap
Summary
Reasons for performing study: Information on precision medicine of intensive care units in the healthcare structures for infection prevention and control in Piedmont Region during surgical interventions.
Objective: To prevent clinical findings and environment interactions in healthcare structures among inpatients with nosocomial infectious diseases and community- acquired infections and to describe the distribution of genotypes of some groups of populations for studying hospital outbreaks.
Background: Nosocomial infectious diseases and pathogenicityrelated genes are studying through the mortality rate increase ranking all possible and new types of family of virus knowing the distribution of genotypes of involved individuals for assisting hospital outbreaks. It is well known that immunocompromised subjects who are in hospital settings especially long-term patients and constrained to the insertion of medical devices such as intravenous and urinary catheters and hospitalized patients at surgery are tracking by the quick sepsis-related organ failure assessment (qSOFA) score to measure multiple organ failure involving lungs, kidneys and liver. We aim to estimate the severity of acute illness presentation which it is associated with a higher mortality analysing the proportion of risk factors by means of the virulence and fitness factors studying the interactions regardless pathogens, host and treatments that is how Enterobacteria resistant to carbapenems, Pseudomonas aeruginosa, Klebsiella and Bukholderia mallei distribute onto immune system and innate immune system deducing human susceptibility to infections onto 90 days. During laboratory cross- contamination, Toll-like receptors are recognizing pathogenic profiles in extra-cells environment of humans and their sequential event reading permits to diagnostic several nosocomial infections such as Venereal lymphogranuloma, ozaenae, rhinoscleromae, pneumonia, tuberculosis and respiratory infections.
Study design: Retrospective cohort study.
Aim: To study the epidemiology of Carbapenemase-Producing Enterobacteriaceae (CPE) in Intensive Care Units (ICUs) and the effect of an infection control intervention.
Methods: Demographic data on the transmissions of HAIs involving admission and stool sampling dates from 24.464 Norovirus infected inpatients were used to estimate the proportion of community-acquired infections. The association between heterogeneous infections with age, sex are fixed effects whereas code wards are including as a random effect in the statistical analysis. A cross sectional point prevalence study (PPS) is conducted in a sample of large acute care hospitals in Piedmont Region. The surveillance methodology is based on the European Centre for Disease Prevention and Control (ECDC) PPS Protocol. ECDC HAI definitions had applied.
Results: This case study identified 669 infected of 24.551 adherent inpatients of which 87 are discarded because of future dates of birth in the sample, then the dimension of the multicenter cohort data is 24.464 rows collected from 44 hospitals in Piedmont Region. The unicenter cohort dataset characterizes 371 susceptible inpatients. The presence of a multi-drug resistant organism is documented for 5.7% of patients. There are 576 HAIs present in 471 patients. The prevalence of patients with a HAI is 1.9% (95%CI: 1.8–2.1). Hospital prevalence rates ranged from 0.6% (95%CI: 0.00- 5.90) to 2.35% (95%CI: 0.00-7.65). Length of stay ranged from 0 to 311 days. Seventeen patients had stayed to the same Ward of the Hospital, observed through a previous admission date. The most common HAIs are surgical site infection, pneumonia and urinary tract infection, comprising 64% of all HAIs identified.
Main limitations: The permanence of patients in hospital structure in Piedmont Region is conditioning the treatments, the outcomes of principal pathology and life tenure of the patient and it is a priori unknown especially in the case of intensive care units because of the complexity of morbidity.
Conclusions: The nosocomial infections are in majority in respect to the community- acquired infections.
Background
In the Coronavirus pandemic era, the covariates to expend during the sampling process of the Italian cities and regions flow to the national, European and world emergency plan on the daily, weekly, monthly calculation, etc. are evaluated and measured through the statistical incidences of the populations of individuals who are now entering into various hospitals to tackle a qualitative and quantitative study of prevalence related to the Healthcare Associated Infections (HAIs) in Turin during the second phases extended for a long time, from July 2021. The association with travel or hospitalization abroad is unknown and the global data in this topic it is not available yet unless it is studying in Italy requiring Region data on patients had to remain anonymous according to laboratory Medicine.
The categorical data representing the predominant characteristics of acute individuals are collected, divided into several compartments: in this case, the distribution of patients by hospital ward at a structural level is of interest to the various statistical units, with reference to both company methodologies and efficient administration of health services so that they are welcomed by patients; personal data and health profile data expand the medical accuracy of each individual patient. The collected data can be represented in contingency tables and graphs through the indexes or statistical indicators of central tendency and stochastic variability to obtain summary and initial verification measures on borderline cases or in the presence of anomalies or exceptions or extreme cases. Longitudinal studies through sampling on one or more populations of susceptible-infected-illdead or safe-immune-removed individuals, they are carrying out in a continuous, constantly updated and effectively maintained way during the healthcare treatment assistance processes increasing the calculation prospects. These stochastic processes will support the decision-making actions of several cooperating government Entities. The benefits are found and appreciated by the communities that they are subjected to statistical surveys thanks to the highly professionalizing technical and technological support system they facilitate survival analysis, introspective or extrinsic, based on the average risk of infection, depending on the prevalent features of an individual to become ill. For example, the implementation of multiple application services is using to retrieving information on HAIs of national hospitals and on patients and they are fundamental for building historical and time series of huge amounts of data available for a future time eventually to explore the consistency and correctness of many statistical studies. The mathematical algorithms we used for solving many applied problems are based on statistical methods in a reinforcement learning regime which they can be simplifying feature scaling and mean normalizations during data classification without altering the initial and the placement conditions of the experiments that they had been associated with random phenomena. In fact, the observations do not change during the data transfer phases but can be processed by means of several models and statistical methods of indispensable importance to optimize and define the extended fields or the limits of applicability of the statistical analysis of data that they measure the prevalence of risk factors in respect to selected indicators and they give a description as exhaustive as possible of the precision medicine of populations of the phenomenon under study. Furthermore, the results are presenting quickly in real-time, and they are the subject of considerations and opportunities for improvements in the scientific- social field. Having digital services with available big data means having teaching materials and open sources to advanced education of innovative, certified and enduring progress, with a collaborative spirit for all during in-depth studies, subjected to timely checks and reconsideration process, referring of obtained results, of corrective actions or processes to be undertaken, for example, to adapt and to replicate the statistical studies we are using, with respect to the changes in the reference protocols such as the follow-up period of surgical site infections, the presence of an earlier X-ray in case of pneumonia or others, to revise the language terminology that it is based on the institutional and work activity communications of interacting groups, to adjust the level of competence of the working group to the required level of competence to achieve the objectives of the working group and to increase coherence and internal and external cohesion by aligning multiple enhancing forces of the group itself, to design new horizons for international directed attitudes to guide the choices of international firms and leading markets, to promote training and scientific research for interdisciplinary transferring knowledge.
Related Works
Hospital outbreaks may be specified by how the transmission of infections is presenting that is via person-to-person contact or via contaminated surfaces, see for example [1] and [2] for further details. The proportion of nosocomial Norovirus (NoV) infections among inpatients testing positive for Norovirus in Denmark on years from 2002 to 2010 had estimated in [3] where the study of the distribution of NoV genotypes had presented as well.
Healthcare-associated infections associated with long-term catheterisation are mostly caused by Morganella morganii and the draft genome sequence of a clinical isolate is reported in [4] where authors identified potential virulence determinants which they could provide new drug targets. Statistical commonly used methods for transmissions of healthcare-associated infections had reviewed in [5] to facilitate future developments of appropriate models in this emerging field and applied to study the prevalence of HAIs in Europe, in the United States, Asia and Africa. In [6], it is showing that the majority of carbapenem-resistant Enterobacteriaceae (CRE) bacteraemias in endemic areas occurred in the SBI ward and that all CRE isolates were Klebsiella pneumoniae carbapenemaseproducing K. pneumoniae. Categories of carbapenemases and their properties detected through a proposed algorithm applied in [7] for infecting strains and screening of carriers.
A timeline and the distribution of identified CPEs and carbapenemase variants reported in [8], which it is a molecular and epidemiological characterization of carbapenemaseproducing Enterobacteriaceae in Norway, from 2007 to 2014. In particular, patients with urinary tract infections (UTIs) assessed in [9], by the prevalence and associated risk factors of multidrug resistant and CPE, at referral Hospital in Northwest Ethiopia. Then, in [10], is studying the molecular characteristics of carbapenemaseproducing Enterobacteriaceae (CPE) in post-acute-care hospitals (PACHs) in Israel, analyzing the temporal changes between 2008 and 2013. Similarly, this topic found in [11]. A lateral flow immunoassay (Carba5) developed and validated in [12], as one lateral flow for the detection of the five main carbapenemases. The study in [13] contributes to show that contact precautions were not effective in reducing the ESBL-Etransmission but they may have had a positive collateral effect on the CPE containment. A chord graph of a nice representation of KPC-21-harboring plasmid (pUR19829-KPC21) characterized the article in [14], in which authors analysed molecular epidemiology and risk factors of CPE Isolates in Portuguese Hospitals. An example of a prospective nationwide study, in 2011-12 is conducted in [15].
Authors identified high colonization prevalence of KPCproducing Enterobacteriaceae among patients in long-term acute care hospitals (LTACHs), in the Chicago region, for a single-day point prevalence survey during January–May 2011, in [16]. Bacteremia by CPE can be reduced by measures of Hospital Infection Control in pediatric hematology-oncology as well, resulted from referenced article [17].
The emergence of carbapenem-resistant Gram-negative bacilli in Mediterranean region imposes the need of indistinctly antibiotics, knowledge on hygiene, the reinforcement of infection control measures, and the early and accurate detection, with restriction of the usage of carbapenems, and it correlated to the spread of these multidrug resistant organisms in [18].
The report [19] regarded Antimicrobial Resistance and Healthcare Associated Infections, between 2004 and 2015, in UK and Ireland. Results presented in [20] indicated that systems for monitoring and detection of ESBL-producing bacteria in Egyptian hospitals have to be established while hospital infection control policies must restrict the consumption of extended-spectrum cephalosporins necessary.
In what concerns multidrug resistance suggested hospital infected, a review of bacteriological and clinical records of patients with a history of hospital exposure in Buenos Aires between January 1994 and June 1995 showed in [21] how IS9110 DNA patterns of three variants of multidrug resistant Mycobacterium tuberculosis strain was isolated from 70 HIV-infected patients and one non-HIV patient, hospitalized at Muñiz Hospital.
Regarding the aim of transmission reduction, in [22] is presented a combined analysis of three mathematical models showing how antiretroviral therapy (ART) interruptions are an increasing proportion of HIV infections and deaths.
Efficient healthcare associated infection surveillance plays an important role at national and international level in [23], in which types of nosocomial infections, nosocomial pathogens, the epidemiology and determinants of nosocomial infections, reservoirs and transmission, prevention and control of nosocomial infections and not least antimicrobial use and resistance are described. In respect to this analysis of nosocomial infection, we consider mainly the part of prevalence of infectious inpatients, recorded in RedCap database, identifying infected patients and reporting risk factor data. A similar study in [24], is concentrated in prevalence of Hospital- acquired infections and resistance rates of Serbian adult, rarely investigated, over a 2- year period, exploring patient characteristics, antimicrobial resistance patterns, and risk factors of acquisition and predictors of mortality. Considering U.S. Hospitals, in [25], changes in prevalence of healtcare-associated infections examined comparing the percentages of patients with HAIs and authors performed a log-binomial multiregression, evaluating the association of survey year with the risk of HAIs.
A post hoc analysis of patients from two prospective observational cohorts of Acinetobacter baumanii colonization or infection provided in [26] the ompA expression as an independent risk factor for pneumonia and bacteremia.
The current knowledge on the potential factors underlying the outcome of Pseudomonas aeruginosa infections in critically ill and immunocompromised patients impacting mortality through the study of prognostic pathogen, host and treatment conducted in [27]. It is fundamental to assess how reliable are the results of this case study from the statistical and clinical point of view of conducted research as it is explained in [28] for pairwise and network metaanalysis of randomized respiratory clinical trials.
A scientific study is investigating in [29,30] a reduction of HAIs by introducing certain intervention measures across factor influencing HAIs that they are divided into three major subject areas, such as: processes and systems in the clinic, staff and patients. HAIs caused by coronavirus diseases performed as a multicenter, retrospective and cross-sectional study in [31], comparing 558 ICUs in Turkey before and during COVID- 19, while in [32], a prospective cohort study analysed Post-COVID-19 condition, three months after hospitalization, in South Africa.
Research in Context
Evidence before this study
The European Centre for Disease Prevention and Control (ECDC) creates the HAI surveillance network HAI-Net by the coordination of the European IPSE (Improving Patient Safety in Europe) project, consulted at [33]. Then, ECDC developed a protocol for the point prevalence study (PPS) of healthcare-associated infections (HAIs) and antibiotic use in acute care hospitals, providing a standardized methodology for Member States and hospitals in response to Article II.8.c of Council Recommendation 2009/C 151/01 of 9 June 2009 on patient safety, including infection prevention and the control of nosocomial infections, see [34]. The protocol inserted more structures and process indicators for the prevention of HAI and antibiotic resistance in acute care hospitals, based on a systematic review of these indicators carried out at the request of the ECDC from the SIGHT project, detailed in [35]. Indicators for antimicrobial stewardship are supported by decisions made by the Transatlantic Task Force on Antibiotic Resistance (TATFAR) working group, see [36].
Added value of this study
This exploration of RedCap data would investigate and picture a point prevalence study of HAIs designing a preventive model in describing infectious patients, then preventing the repetition of such disease cases. It would be an example of statistic analysis conducted through R Studio empowering this fundamental integrated development environment, showing valuable results related to our research topic.
Implications of all the available evidence
This study provides data that can help to know some numbered data and characterization of infected population in Italy, in particular in Piedmont Region and in Turin city. These collected official data can prevent infectious cases in the future as they are analysed and described completely, guiding physicians in followups and in quality healthcare programs, to assist patients and reduce infection rate.
Materials and Methods
Sampling from Piedmont Region populations of inpatients. A population of 174 inpatients from AOU S. Luigi in Orbassano (Turin) was eligible as a first statistical surveillance review of clinical data during the study period of seven months, from November 2018 to June 2019, that it can be divided in three sub-periods of statistical studies such as onto 90 days twice and 30 days to calculate the case-finding survey of infected patients in a healthcare structure or in a hospital ward.
One population of 371 susceptible individuals from two wards of Gradenigo Hospital in Turin we consider as an unicenter cohort of intensive care units from April 2019 to March 2020 that is they had been observed for eleven months. The file “Unicenter.csv” contains those data. Two clinical cohort prospect observational onsets drawn from Orthopedics and Urology wards of Gradenigo Hospital. 24.464 patients from two prospective observational cohorts of colonized or infected extended-spectrum beta- lactamase producing (ESBL) were adherent to screening for carbapenemase- producing Enterobacteriacae (CPE) by rectal swab over a consecutive threeday period in March 2020. Screening was offered to all patients in the surgical division on Day 1, all patients in the medical division on Day 2 and all patients in the specialist and critical care divisions on Day 3 mostly. We refer to [30], for deep neural network-based methods, that they are anticipated to reduce diagnosis time for pathologists. Indeed, we report infections associated to plasmidmediated AmpC (PMAβ)-producing Enterobacteriacae isolates they are usually resistant to many other non-β-lactam antibiotics, then we retrieve microorganisms of types Ampi-R&C3-S(1), C3-R(2) and C3-R(2), Ampi-S mainly to measure the multiresistance of the overall population of clinical inpatients during the study period of three years and five months: the observables are referring with the dates from the 31/05/2018 to the 06/08/2021 for one study period of three years and two months.
During this studying observed data, it is remarkable they will produce a suitable scenario for future patients in the same conditions and future inpatients with other clinical features as prospecting an audience segmentation of more populations of individuals showing the transmissions of healthcare acute infections comparing them through several evaluating and evaluated known models. Analysing the antimicrobial susceptibility and the molecular characterization by means of bacterial isolates will help to identify Hospital areas in which inpatients are subjected to high risk or not to HAIs and several different groups of inpatients will compare from the registered, targeted and labelled population of flowing populations of individuals. 141 rows had removed from the initial dataset because they resulted incomplete. The prevalence of CPE amongst Italian healthcare structures inpatients was calculated for one hospital as a whole and for each division from the patient administration system (PAS) with 95% confidence intervals (CI) using recorded data in RedCap which they are processing by means of R Studio. History of treatment data of inpatients collects the date of birth, the division of admission, episode duration and data on the implantation of prosthetic material in the preceding 24h. If the patient moved between divisions during the permanence period and swabbed multiple times, only the last results were available for this study. Featured susceptible isolates are recording by age, sex, sampling date, infection type, isolation site referencing with the hospitalization ward, hospitalization days and in hospital death. Clinical inpatient features are designing through the estimate of tolerance limits defined for a statistical control process monitoring the infection rates in the analysed populations groups. The characterization of infected or colonized patients is implementing through unadjusted odds ratio (OR) will be calculated for each risk factor. Factors associated with increased risk of CPE colonization at P < 0.05 on univariate analysis, along with age as an a-priori confounder, were entered into a multivariate logistic regression model using a forward stepwise selection process.
Prevalence risk factors of infected inpatients. We highlight the study of the distribution of genotypes of some groups of populations evaluating hospital outbreaks among inpatients with nosocomial infectious diseases and community-acquired infections through clinical characteristics of patients with the distributions of the interactions regardless pathogens, host and treatments during hospitalizations. In the most of assisting hospital outbreaks, the resistance of CPE to the classes A, B and D of antibiotics and the carbapenemase genes in Enterobacteriaceae lead to therapeutic failure facilitating infectious breakpoints they are increased by mobile genetic elements such as plasmids or transposons during the exposition of infected inpatients to community-acquired infections.
The variables we considered in the analysis were medication and length of stay. However, none of the risk factors were independently associated with being a CPE carrier. Using logistic regression, in the following table, we deduced that the only risk factors significantly associated with being a newly identified CPE-positive patient were age and having been administrated an antibiotic on the day of the survey.
Results
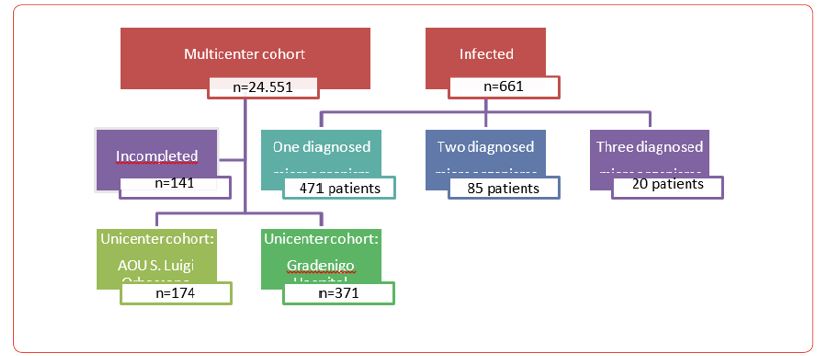
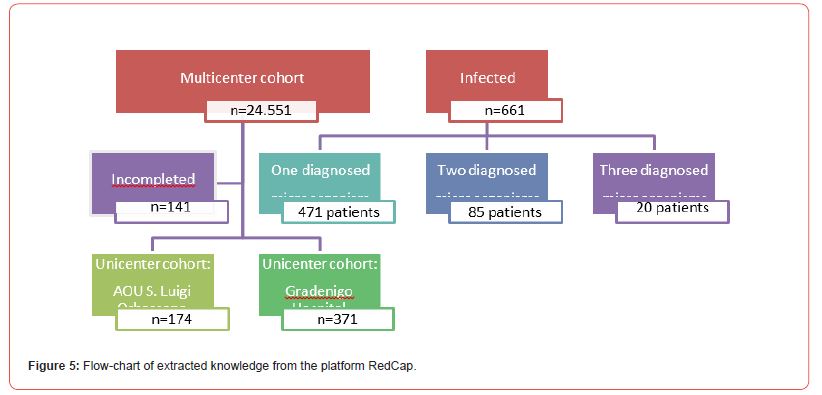
Study of the transmission of infections of clinical populations of individuals. We made a post hocanalysis of patients from whom some microorganism had been isolated from the collection of samples of the initial patient population, performed in 25 hospitals in Piedmont Region. Inpatients from two prospective observational cohorts with infectious microorganism colonization or infection were eligible. Over the study period, 24.551 inpatients are identified as unique patients and transfers among more wards of divisions had reported any.
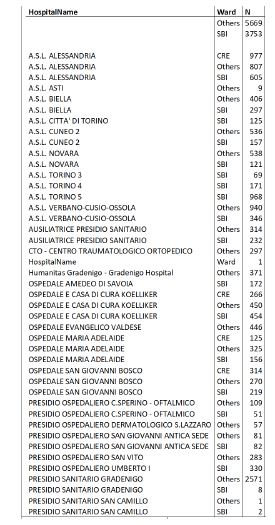
The median age of patients in the study is 74 years (quartile range 63-82 years even though the overall dataset contains inpatients age from 1 to 110 years) and the 54.1% of the sample are female. The frame table in the next figure is counting the permanence of individuals in Piedmont Region healthcare structures by Division in order to give immediately the idea of the data distributions for evaluating and proposed known models, understanding controlled nosocomial and community- acquired infections.
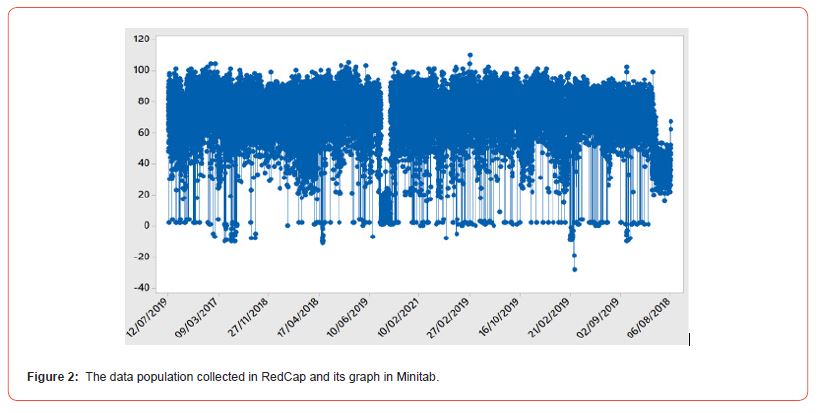
Starting with visualizing all data of all inpatients registered on RedCap database, we show in the following figure the data population divided into time and age of patients [Figure 1,2].
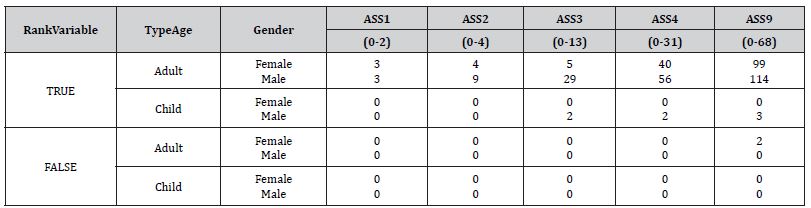
Dealing with the proportions of infections in the referring time, we observed the carriage of patients in Turin reported in Table I where the prevalence of stays compared by the qSOFA Score and the temporal duration is smaller than 15 days. The counts emerging by infected population of inpatients named “Unicenter2.csv”, colonized from the dataset “Unicenter.csv”, after the retirements of several misunderstanding of data collected in throughout one dataset cleaned by the overall localized study of infective diseases, from the two Divisions of Gradenigo Hospital in Turin they are the Orthopedics and the Urology Wards. The represented data population in the tables below are comparing with the collected data from the healthcare structures in Turin throughout the R Studio computations of confidence intervals with the information level of 95% for studying accuracy [Figure 3], [Table 1].
Table 1:Proportion of HAIs in the time to refer with respect to the data collection time.
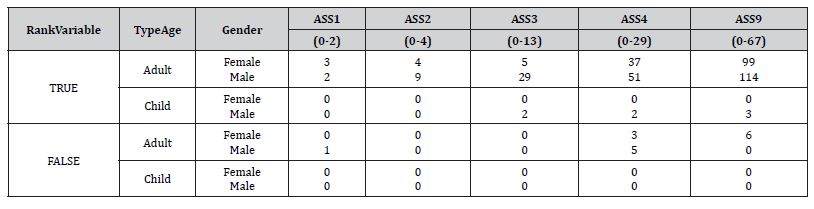
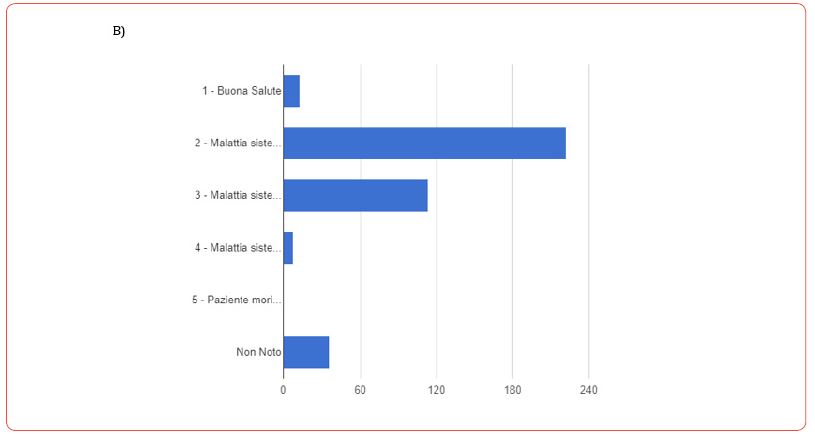
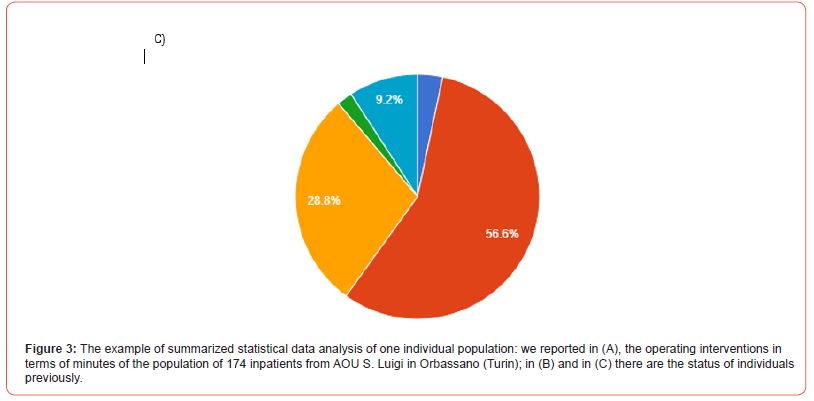
Assessment statistic variables in these tables are relative to the calculated mean interval between admission and colonization, expressed by days, to know the spatial and temporal distributions of colonized and not colonized patients characterizing the populations of patients especially by the stay wards and by those with severe brain injuries (SBI). The “FALSE” variable chose to indicate when the algorithm was failing on computing predictors whereas the ranges in the assessments due to significant confronts among marginal distributed data. Indeed, the data distribution overall was not a stochastic result for reading and they were normal distributed as one empirical distribution whom we did not require several trials to explore them firstly [Table 2].
Table 2:Proportion of Stays for the hospitalization of inpatients and the transmission of HAIs in infection care units.
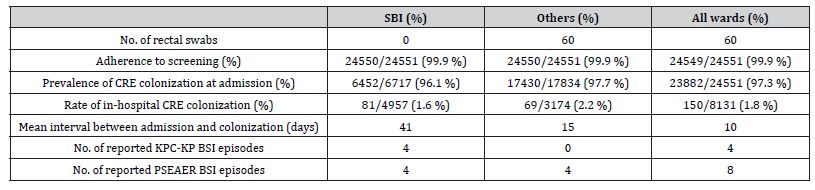
Adherence population is clearly near in respect to the expected valued random population, then some considerations from this table are fundamental for the problem objected study such as the verifying episodes of BSI are related to the presence of microorganisms ”KPC-KP” and ”PSEAER” considering the hospital divisions overall that it is deciding to evaluate when two type of HAIs developed near the BSI episodes, analyzed for the Turin City and not in Countries, turning out individual resistance to infectious populations even thought we had not list all symptoms of disease because of the infection in this time could be approved as strong or the surveillance was not subjective too. Nevertheless, cleaning the room usually aiding individual nosocomial infections limiting the action hospital operators. Furthermore, adjacency-controlled cases alert the spreading of times [Table 3].
Table 3:Overview of surveillance data relative to the referred period of observation of the aleatory phenomenon for the Turin City.
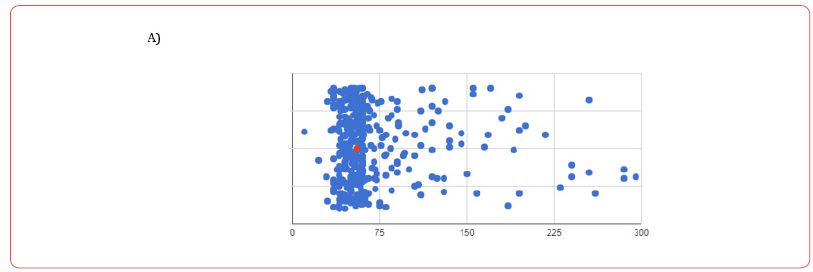
At this period, for example, we are comparing the statistic populations of Turin City are classical represented in respect to the observation time, when they fellow the target population, using variables “ASS” for Assessments, and its classical trend, during the second phase SARS-COV2-19 pandemic period, when arrival concerned by foreign Countries only, that is it is well done if it is considering again them as target population while calculations on infective individuals were the sampled distribution, made autonomously in R Studio within we retrieve it is always increasing and strongly dependent by its classes of data, they are reordered in terms of the probability density of normal sampling distribution through relative frequencies and rescaled referenced measures for the times expressed by days. Furthermore, the two statistical populations had a different nature, and they are presented as fundamental to know, equally [Figure 4].
In the study period, 302 patients were diagnosed with at least 1 HAI, an incidence rate of 1.23%, and a total of 669 HAI episodes were documented, among 24.551 registered Italian patients in Piedmont Region. A total of 302 isolates were identified, most common being Enterobacter cloacae, Staphylococcus aureus and Enterococcus faecium, see numeric details in the following table [Table 4].
After characterized patients by antibiotic use 48h upon admission, antimicrobial resistance rates were investigated for all pathogens and stratified for the three most frequent isolates, see the following tables [Table 5, 6].
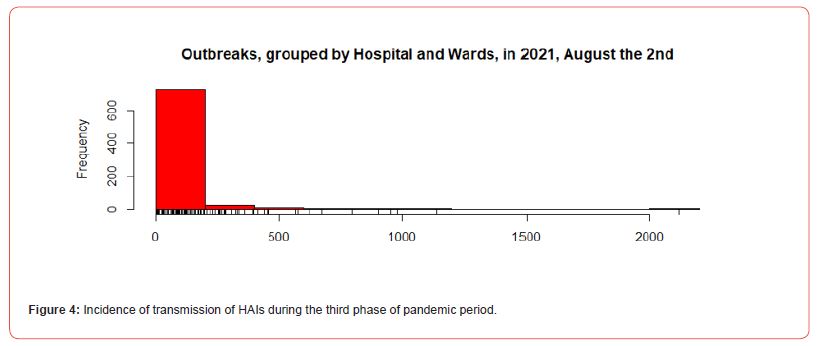
Table 4:At least one microorganism, diagnosed in registered patients.
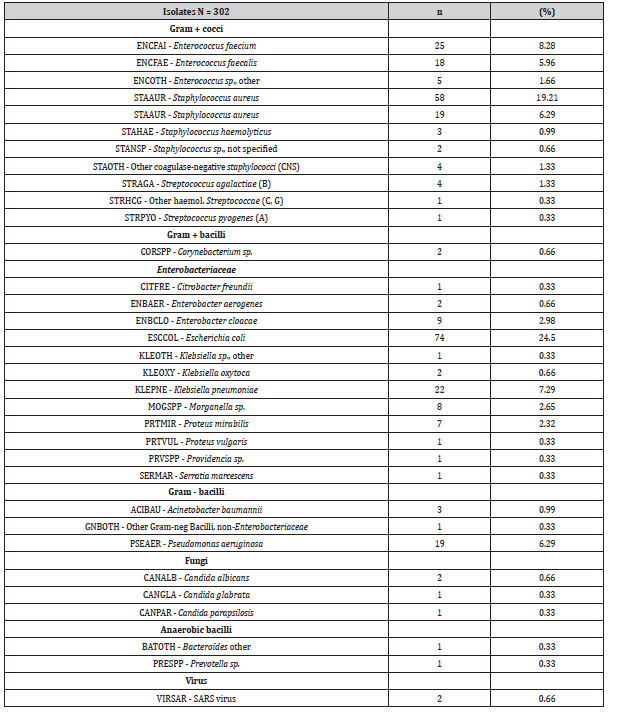
Table 5:Characteristic of patients admitted to ICUs.
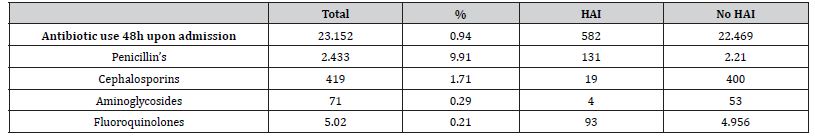
Table 6:Antimicrobial resistance patterns.
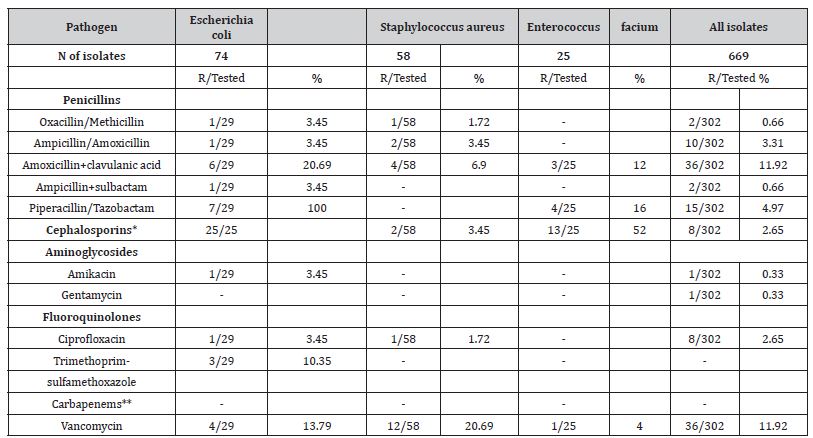
Table 7:Univariable analysis of risk factors of HAIs in the healthcare structures.
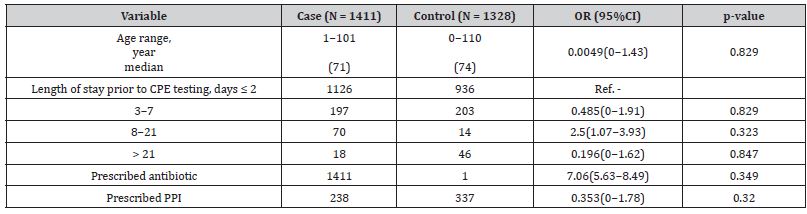
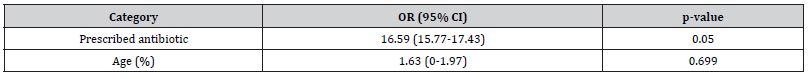
Table 8:Final multi-variable logistic regression analysis of risk factors for carriage of CPE.
The next flow chart represents data analysis method studying the topic of this research.
In the following graphs, we illustrate the absolute frequencies of patients who infected by two and three microorganisms by means of the association rules of collected and interesting data, using R-extension package arulesViz. Indeed, many organizations generate a large amount of transaction data on a daily basis. For example, Italian Entity of Data, the “Istituto Superiore della Sanità” (ISS), record everyday great numbers of infectious inpatients using check-in and check-out data. Association rule mining is one of the major techniques to detect and extract useful information from large scale transaction data. Then, association rules are rules which surpass a user- specified minimum support and minimum confidence threshold. What is doing the R algorithm is using, in a first step, minimum support to generate the set of all frequent itemsets for the data set. These frequent itemsets are itemsets which satisfy the minimum support constraint. Then, in a second step, each frequent itemsets is used to generate all possible rules from it and all rules which do not satisfy the minimum confidence constraint removed. We define dataset association rules in R Studio as follow:
library(“arulesViz”)
rules <- apriori(Multicenter23[,1:25], parameter=list(support=0.001, confiden ce=0.5))
Apriori
Parameter specification:
confidence minval smax arem aval originalSupport maxtime support minlen maxle n target ext
0.5 0.1 1 none FALSE TRUE 5 0.001 1 1
0 rules TRUE
Algorithmic control:
filter tree heap memopt load sort verbose
0.1 TRUE TRUE FALSE TRUE 2 TRUE
Absolute minimum support count: 24
set item appearances ...[0 item(s)] done [0.00s].
set transactions ...[90464 item(s), 24551 transaction(s)] done [1.11s]. sorting and recoding items ... [1355 item(s)] done [0.04s].
creating transaction tree ... done [0.04s].
checking subsets of size 1 2 3 4 5 6 7 done [9.69s]. writing ... [8762494 rule(s)] done [22.39s]. creating S4 object ... done [20.17s].
rules
set of 8762494 rules
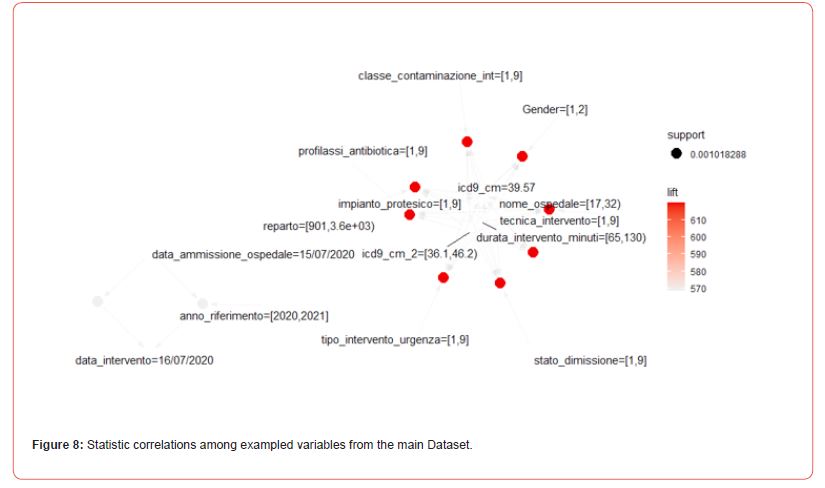
The result is a set of 5668 association rules. The top three rules with respect to the lift measure, a popular measure of rule strength, are:
inspect(head(rules, n = 3, by =”lift”))
lhs rhs support confide nce coverage lift count
[1] {nome_ospedale=[17,32), icd9_cm_2=[36.1,46.2),
impianto_protesico=[1,9],
durata_intervento_minuti=[65,130)} => {icd9_cm=39.57} 0.001018288 0.7575
758 0.001344141 619.9747 25
[2] {nome_ospedale=[17,32), reparto=[901,3.6e+03),
icd9_cm_2=[36.1,46.2), impianto_protesico=[1,9],
durata_intervento_minuti=[65,130)} => {icd9_cm=39.57} 0.001018288 0.7575
758 0.001344141 619.9747 25
[3] {nome_ospedale=[17,32), icd9_cm_2=[36.1,46.2),
impianto_protesico=[1,9],
durata_intervento_minuti=[65,130),
profilassi_antibiotica=[1,9]} => {icd9_cm=39.57} 0.001018288 0.7575
758 0.001344141 619.9747 25
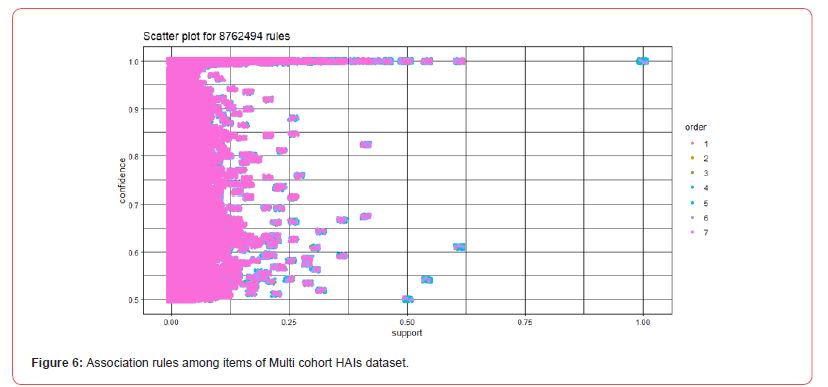
The following graph is showing a very strong inverse relationship between the order and the support, which is a known fact for association rules.
> plot(rules, method = “two-key plot”)
This plot is also available in an interactive mode, selecting a region with two clicks [Figure 6].
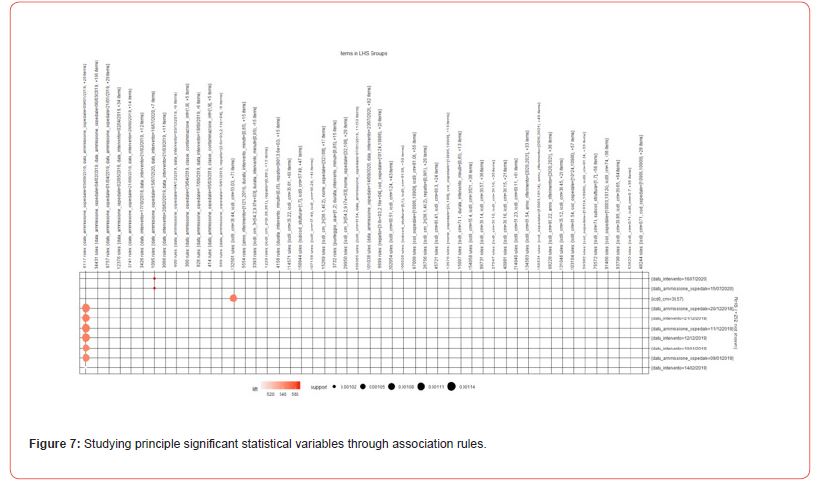
From the following graph in the next figure, it results that main featuring population of inpatients is describing by two fundamental variables they are admission date and intervention date [Figure 7].
> plot(rules, method = “grouped”, control = list(k = 50)
In the following plot, we represented items and rules as vertices connecting them with directed edges, see Figure 7. This representation focuses on how the rules are composed of individual items and shows which rules share items [Figure 8].
The next flow chart represents data analysis method studying the topic of this research.
Discussion
Comparing the two initial unicenter cohorts, extracting data from two Piedmont Hospital structures, one in Turin city and the other very near to Turin, we reported few infection cases: only one in Gradenigo Hospital due to Morganella microorganism and two in AOU S. Luigi Orbassano Hospital caused by at least one microorganism not diagnosed by medical staff. Overall, the main HAIs were urinary tract infections, skin infections, pneumonia and respiratory infections.
There were 25 known CPE-positive patients within Piedmont Region hospitals, then the prevalence was of 1.3%. Following our proposal case study, appropriate 173 additional patients were examined for isolation, likely to have prevented onward infectious transmission. The prevalence of CPE at Piedmont Region appears to be in line with all other Italian Regions. In our healthcare facilities, understanding the risk factors associated with the spread of CPE as fundamental prevention to tackle transmission, during CPE carriages, it summaries in increasing age and antibiotic administration on the day of the survey. We highlight the features collecting during this case study in which dataset information on the number, type and duration of antibiotic prescription were available and indicate the main characterization of the inpatient diseases made by physicians. Indeed, the exposure to penicillins it is well-known that it has been associated with increased risk of CPE colonization. Then, the length of stay has not been identified as the most important risk factor in this study and the transmission of HAIs may be due to the small study size [Table 7].
In addition, the following table reports the importance of the risk factor of prescribed antibiotic [Table 8].
Finally, exploring detected microorganisms among inpatient of Piedmont Region healthcare structures, the 1.3% had one and constituted the infectious population as one unicenter cohort whereas the individuals that present another microorganism after the first one, are the 0.35%, while who had three microorganisms were the 0.08% of agreeing people to registering personal data. Registered infections are then examined behind their nature, and they result of type: urinary tract infections, skin infections, pneumonia and respiratory infections, respectively.
Conclusion
The case study we described here was a small study with routine data which they were available in RedCap during the period of study and it results that the nosocomial infections are in majority in respect to the community-acquired infections, following the national trend. The study was conducted in healthcare structures of Piedmont Region and at “one point” in time and it was helpful for the hospitals to identify and describe the burden of CPE and demonstrated the feasibility of using a point prevalence study to investigate CPE epidemiology. We explored ten datasets from which we extracted relevant knowledge about featuring healthcare associated infections and characterizing populations of individuals registered as infectious cases. We visualized the variables the most significant for detecting useful exampled perspectives characterizing patients and supporting the physicians to take care of them in presence of similar pathologies. Future surveillance programs may retrieve these kinds of information about HAIs and this study wanted to be a guided example for other personalized electronic health recorded inpatients to know more about their stay in hospital, infectious disease and compare their personal health experience with other typical or atypical situations of pathologies. Fundamental were precaution measures to consider in control and prevent HAIs, reducing the risks of outbreaks.
Disclosure of Interest
The author declares there are not conflicts of interest any.
Funding
No funding was received for this research.
Acknowledgment
None
References
- Elisabeth Mathijs, Ambroos Stals, Leen Baert, Nadine Botteldoorn, Sarah Denayer, et al. (2012) A review of known and hypothetical transmission routes for noroviruses. Food Environ Virol 4(4): 131-152.
- N A Emslie, G E Greening, J P Rapana, T W Sprott, C N Thornley (2011) Recurring norovirus transmission on an airplane. Clin Infect Dis 53(6): 515-520.
- B Bottiger, A K Ersboll, T K Fischer, K T Franck, B J Holzknecht, et al. (2015) Norovirus Genotypes in Hospital Settings: Differences Between Nosocomial and Community-Acquired Infections. The Journal of Infectious Diseases, Oxford University Press 212(6): 881-888.
- C-H Chen, H-C Chen, Y-T Chen, M-F Hsieh, F-R Hsu, et al. (2012) Whole-genome sequencing and identification of Morganella morganii KT pathogenicity-related genes. BMC Genomics, BioMed Central 13(Suppl 7): S4.
- S Howick, I Megiddo, LK N Nguyen (2019) Simulation models for transmission of health care–associated infection: A systematic review. American Journal of Infection Control 48(7): 810-821.
- F Arena, F Vannetti, V Di Pilato, L Fabbri, O L Colavecchio, et al. (2018) Diversity of the epidemiology of carbapenemaseproducing Enterobacteriaceae in long-term acute care rehabilitation settings from an area of hyperendemicity, and evaluation of an intervention bundle. Journal of Hospital Infection 100(1): 29-34.
- P Nordmann, L Poirel (2013) Strategies for identification of carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother 68(3): 487-489.
- O Samuelsen, S Overballe-Petersen, J Vildershøj Bjørnholt, S Brisse, M Doumith N, et al. (2017) Molecular and epidemiological characterization of carbapenemaseproducing Enterobacteriaceae in Norway, 2007 to 2014. PLoS ONE 12(11): e0187832.
- S Eshetie, C Unakal, A Gelaw, B Ayelign, M Endris, et al. (2015) Multidrug resistant and carbapenemase producing Enterobacteriaceae among patients with urinary tract infection at referral Hospital, Northwest Ethiopia. Antimicrobial Resistance and Infection Control 4:12.
- A Adler, O Hussein, D Ben-David, S Masarwa, S Navon-Venezia, et al. (2015) Persistence of Klebsiella pneumoniae ST258 as the predominant clone of carbapenemase-producing Enterobacteriaceae in post-acute- care hospitals in Israel, 2008–13. J Antimicrob Chemother 70(1): 89-92.
- S H Jeong, H S Kim, J S Kim, D H Shin, H S Kim, et al. (2016) Prevalence and Molecular Characteristics of Carbapenemase-Producing Enterobacteriaceae From Five Hospitals in Korea. Ann Lab Med 36(6): 529-535.
- H Boutal, A Vogel, S Bernabeu, K Devilliers, E Creton, et al. (2017) A multiplex lateral flow immunoassay for the rapid identification of NDM-, KPC-, IMP- and VIM-type and OXA- 48-like carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother 73(4): 909-915.
- M Hernández-García, C Díaz-Agero, B Pérez-Viso, A M Sánchez, N López- Fresnena, et al. (2020) Implementation of contact isolation strategy for the containment of extended-spectrum β-lactamase carriers in a University Hospital positively affects the epidemiology of carbapenemase-producing Enterobacterales. Enferm Infecc Microbiol Clin S0213-005X (20)30210-X.
- Manageiro, R. Romão, I. B. Moura, D. A. Sampaio, L. Vieira, et al. (2018) Molecular Epidemiology and Risk Factors of Carbapenemase-Producing Enterobacteriaceae Isolates in Portuguese Hospitals. Front Microbiol 9:2834.
- J Robert, A Pantel, A Mérens, J P Lavigne, M H Nicolas-Chanoine, et al. (2014) Incidence rates of carbapenemase-producing Enterobacteriaceae clinical isolates in France: a prospective nationwide study in 2011-12. J Antimicrob Chemother 69(10): 2706-2712.
- M Y Lin, R D Lyles-Banks, K Lolans, D W Hines, J B Spear, et al. (2013) The Importance of Long-term Acute Care Hospitals in the Regional Epidemiology of Klebsiella pneumoniae Carbapenemase– Producing Enterobacteriaceae. Clinical Infectious Diseases 57(9): 1246-1252.
- D Caselli, S Cesaro, F Fagioli, F Carraro, O Ziino, et al. (2015) Incidence of colonization and bloodstream infection with carbapenem-resistant Enterobacteriaceae in children receiving antineoplastic chemotherapy in Italy. Infectious Diseases 48(2):152-5.
- N Djahmi, C Dunyach-Remy, A Pantel, M Dekhil, A Sotto, et al. (2014) Epidemiology of Carbapenemase-Producing Enterobacteriaceae and Acinetobacter baumannii in Mediterranean Countries. BioMed Research International 2014: 305784.
- E Taylor, S Sriskandan, N Woodford, K L Hopkins (2018) High prevalence of 16S rRNA methyltransferases among carbapenemase-producing Enterobacteriaceae in the UK and Ireland. International Journal of Antimicrobial Agents 52(2): 278-282.
- H M Abdallah, B B Wintermans, E A Reuland, A Koek, N al Naiemi, et al. (2015) Extended-Spectrum β- Lactamase- and Carbapenemase-Producing Enterobacteriaceae Isolated from Egyptian Patients with Suspected Blood Stream Infection. PLoS ONE 10(5): e0128120.
- M Ambroggi, L Barrera, A Dambrosi, N Isola, M Di Lonardo, et al. (1997) Nosocomial Spread of Human Immunodeficiency Virus– Related Multidrug-Resistant Tuberculosis in Buenos Aires. The Journal of Infectious Diseases 176(3): 637-642.
- A Bershteyn, L Jamieson, H Y Kim, I Platais, M P Milali, et al. (2022) Transmission reduction, health benefits, and upper-bound costs of interventions to improve retention on antiretroviral therapy: a combined analysis of three mathematical models. Lancet Glob Health 10(9): E1298-E1306.
- H A Khan, F K Baig, R Mehboob (2017) Nosocomial infections: Epidemiology, prevention, control and surveillance Asian Pa J Trop Biomed.
- A Despotovic, B Milosevic, I Milosevic, N Mitrovic, A Cirkovic, et al. (2020) Hospital-acquired infections in the adult intensive care unit – Epidemiology, antimicrobial resistance patterns, and risk factors for acquisition and mortality. American Journal of Infection Control 48(10): 1211-1215.
- R Alvarez-Marin, G Bou, J M Cisneros, F Fernandez-Cuenca, J Garnacho- Montero, et al. (2017) Overproduction of outer membrane protein A by Acinetobacter baumannii as a risk factor for nosocomial pneumonia, bacteremia, and mortality rate increase. The Journal of Infectious Diseases 215(6): 966-974.
- S S Magill, E O’Leary, S J Janelle, D L Thompson, G. Dumyati, et al. (2021) Changes in prevalence of health care associated infections in U. S. Hospitals. N Engl J Med 379(18): 1732-1744.
- C Juan, A Oliver, C Pea (2017) Host and Pathogen Biomarkers for Severe Pseudomonas aeruginosa Infections. The Journal of Infectious Diseases 215(suppl_1): S44-S51.
- L Calzetta, P Rogliani (2019) Critical interpretation of pairwise and network meta- analysis of randomized respiratory clinical trials. The About Open Pneumology 5: 1.
- V Kolbe, L Ewald, H Mallwitz, H Niesalla (2022) Factors influencing healthcare- associated infections. Hyg Med.
- S Sari, F Arslan, S Turan, T Mengi, H Ankarali, et al. (2023) Comparison of the healthcare- associated infections in intensive care units in Turkey before and during COVID-19. The Egyptian Journal of Internal Medicine 35(1): 30.
- M Dryden, C Mudara, C Vika, L Blumberg, N Mayet, et al. (2022) Post-COVID-19 condition 3 months after hospitalization with SARS-CoV-2 in South Africa: a prospective cohort study. Lancet Glob Health 10(9): e1247-e1256.
- V Pham, H Nguyen, B Pham, T Nguyen, H Nguyen (2022) Robust Engineering-based Unified Biomedical Imaging Framework for Liver Tumor Segmentation. Curr Med Imaging 19(1): 37-45.
- (2009) Improving Patient Safety in Europe (IPSE). The IPSE report 2005-2008. Lyon: Université Claude Bernard Lyon1.
- Council Recommendation of 9 June 2009 on patient safety, including the prevention and control of healthcare associated infections (2009/C 151/01), Council of the European Union, (2009).
- W Zingg, A Holmes, M Dettenkofer, T Goetting, F Secci, et al. (2015) Pittet; for the systematic review and evidence-based guidance on organization of hospital infection control programmes (SIGHT) study group. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis 15(2): 212-224.
- L A Pollack, D Diamantis Plachouras, H Gruhler, R Sinkowitz-Cochran (2014) DRAFT: Report on the modified Delphi process for common structure and process indicators for hospital antimicrobial stewardship programmes. Transatlantic Taskforce on Antimicrobial Resistance (TATFAR), US CDC, ECDC, (2014).
-
Cauli Alessandra*. An Empirical Evaluation on The Transmissions of Healthcare Associated Infections in Healthcare Structures in Piedmont Region. Curr Tr Clin & Med Sci. 3(5): 2024. CTCMS.MS.ID.000572.
-
epidemiology, Enterobacteriaceae, infection pneumonia, urinary tract infection
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






