 Opinion Article
Opinion Article
Introduction to A New Approach to Treat Insomnia by Improving Daily Movements
Shinnosuke Harada1*, Anna Ueda2 and Sumire Sato3
1Faculty of Psychology, Iryo Sosei University, Fukushima, Japan
2Community Psychology, Counseling, and Family Therapy Department, St. Cloud State University, Minnesota, USA
3Faculty of Psychology, Iryo Sosei University, Fukushima, Japan
Shinnosuke Harada, Faculty of Psychology, Iryo Sosei University, Fukushima, Japan.
Received Date: October 12, 2021; Published Date: October 22, 2021
Introduction
Insomnia is a type of sleep disorder in which patients exhibit difficulty falling asleep, difficulty staying asleep with frequent awakenings, and early-morning awakening without being able to return to sleep [1]. Although medication is the primary treatment for insomnia, due to its addictive feature and side effects, nonpharmacologic intervention have also become recommended in recent years. Two of the most well-known nonpharmacological interventions are Restriction Therapy and Stimulus Control Therapy [2]. In Sleep Restriction Therapy, patients plan to restrict their sleeping hours to enhance their sleep efficiency. In Stimulus Control Therapy, patients control the behaviors that prevent them from sleeping and enforce conditioning of lying in bed and sleeping. Both treatments are evidence-based behavioral therapies for insomnia and are practiced in numerous clinical settings.
In addition to the above behavioral therapies, relaxation interventions of patients with insomnia have been practiced. For instance, Autogenic Training, Progressive Muscle Relaxation, and Biofeedback have been practiced for patients with insomnia for many years. These interventions allow patients to relax their bodies and muscles to improve their ability to fall asleep and stay asleep [3]. Mindfulness is another intervention treatment that has attracted attention in recent years. There has been a noteworthy development of programs using mindfulness and their use in evidence-based research and clinical practice [4]. In this way, interventions to address insomnia from the perspectives of relaxation have developed from various aspects based on different methodologies, and each has shown its effectiveness.
“Dohsa Hou” or “Movement Therapy” in English is a new relaxation treatment to be used for patients with insomnia. Dohsa Hou is a psychotherapy developed in Japan to improve clients’ mental health by intervening in their movement [5]. As a note, based on a clinical psychology term, the term “client” is used instead of “patient.” Gosaku Naruse, the developer of this therapy, interpreted human movement not merely as a physical motor phenomenon but as a psychological one, and looked into the psychology behind each movement. Based on Naruse’s development and practice of Dohsa Hou, research has proven that various psychological factors influence human movements, and in turn, movement influences psychology. Therefore, improvement of movement will improve mental health. Most clients who have physical or mental disorders or inhibitions have high body tension, dull somatic sensation, and poor sensation of relaxed feeling [6]. According to the theoretical school of Dohsa Hou, these somatic problems are related to how the clients use, position, and move their bodies [5].
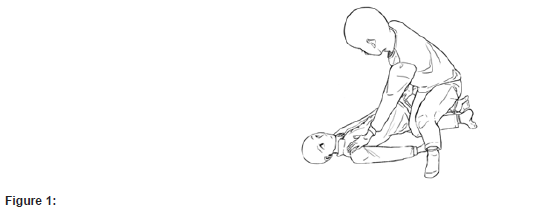
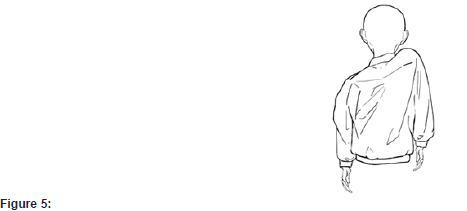
Based on these theoretical foundations, case studies were conducted by Harada et al (2018) and Harada (2020). Patients with insomnia noted improved outcomes in clinical scales in insomnia after four one-hour sessions [7,8]. Harada & Harada (2021) developed a Dohsa Hou program consisting of four sessions for insomnia patients and applied this program to clinical cases. Results showed effectiveness and improved clinical scales and actigraphy [9]. The core aim of this program is to loosen the back of the client, to help clients learn a stable sitting position, and to enhance the client’s range of motion, primarily in their arms and shoulders as shown in figures 1 through 5. Training to twist their upper body while laying on their side (Figure 1), the training to lean the upper body forward from the pelvis and then sit up while keeping the spine straight (Figure 2,3), the training to raise an arm up along the side of the body (Figure 4), and the training to move shoulders up and down (Figure 5). The explanation of the goals and functions of each training is omitted but in all of the trainings, clients are expected to be engaged in focusing on their own body and sensations. Clients focus on controlling the muscle tension that blocks movement and to adjust the level of control they exert.



When these goals are achieved, clients are able to improve their movements in daily life and increase the number of physically and mentally comfortable experiences. Eventually, their chronic anxiety and ruminations about insomnia will decrease, and their cognitive and physical hyperarousal before sleep will reduce [7,8]. In addition to the relaxation effect described above, Dohsa Hou has the added function of accumulating the experience of comfort in body and mind and improving the motivation for activity during waking hours, an important consideration for older patients with insomnia in improving their quality of life [7,8]. The above points are considered to be important in solving the problem of insomnia, as they can function to improve the balance of the client’s sleepwake rhythm.
Dohsa Hou is a very unique intervention technique as it approaches patients with insomnia from a perspective focused on the relationship between psychology and movement. It not only brings relaxing effects by reducing hyperarousal which prevents sleep but also urges clients to reflect on their daily activities through body movement and to make adjustments. Although the application is limited to a small-scale practical study in Japan, we hope to attract attention for using Dohsa Hou as a new widely accepted and practiced treatment approach for insomnia.
Acknowledgment
We wish to extend a special thanks to the managing editor of the journal for giving us the opportunity. We would also like to dedicate the article to Mr. Gosaku Naruse, the developer of Dohsa Therapy.
Conflict of Interest
The authors declare that there are no conflicts of interest.
References
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edition: Dsm-5. American Psychiatric Publishing.
- Morin CM, Harui PJ, Espie CA, Spielman AJ, Buysee DJ, et al. (1999) Nonpharmacologic Treatment of Choronic Insomnia. An American Academy of Sleep Medicine Review. Sleep 22(8): 1134-1156.
- Lichstein LK, Taylor JD, McCrae SC, Thomas JS (2011) Relaxation for Insomnia. In M Perlis, M Aloia, & B Kuhn. (Eds). Behavioral Treatments for Sleep Disorders. A Comprehensive Primer of Behavioral Sleep Medicine Interventions. Academic Press.
- Rusch LH, Rosario M, Levison ML, Olivera A, Livingston SW, et al. (2019) The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences 1445(1): 5-16.
- Imura O (2015) The Birth and Development of Dohsa-hou. Osamu Imura, & Velizara Chervenkova. (Eds). Introduction to Dohsa-hou-An Integrated Japanese Body-Mind Therapy. Graduate School of Human Sciences, Osaka University.
- Aposhyan S (2004) Body Mind Psychotherapy: Principles, Techniques, and Practical Applications. WW Norton & Company.
- Harada S, Murakami J, Miyawaki H, Hatakenaka Y, Oishi T, et al. (2008) A case indicating the effectiveness of clinical Dohsa-hou for treatment of insomnia. Psycho-clinical research 36(3): 350-356.
- Harada S (2020) An example of Dohsa-therapy intervention for a client with psychophysiological insomnia. Psycho-clinical research 38(3): 185-195.
- Harada S, Harada E (2020) Demonstrating the Effectiveness of Dohsa-Therapy Using Actigraphy in Treating Insomnia. Proceedings of the 39th Annual Meeting of the Japanese Psychological Association 178.
-
Shinnosuke Harada, Anna Ueda, Sumire Sato. Introduction to A New Approach to Treat Insomnia by Improving Daily Movements. Cur Trends Civil & Struct Eng. 2(5): 2021. CTCMS.MS.ID.000547.
-
History of medicine, Neighborhood, Mysterious sickness, Mineral, Planet, Solar system, Uranium, Potassium sulfate, Radium, Comparison, Measurements, Self-luminous, Environmental problem, Belgium
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






