 Opinion Article
Opinion Article
Health Care Utilization up to 180 Days After Initial COVID-19 Diagnosis Among a Nationwide Sample of Insured Adults Aged 18-29 Years: An Analysis of Claims Data
Glenn Melnick* and June O’Leary
Sol Price School of Public Policy, University of Southern California, USA
Glenn Melnick, Sol Price School of Public Policy, University of Southern California, USA.
Received Date: September 22, 2021; Published Date: October 06, 2021
Abstract
Objective: To describe the health care utilization patterns of a large sample of young commercially insured adults in the U.S. after an initial COVID-19 diagnosis. Methods: Analysis of claims data of adults aged 18-29 years covered by a large national insurer with at least one day of enrollment from March 1 through July 31, 2020. An initial diagnosis of COVID-19 was identified by a confirmed (ICD-10 diagnosis code U07.1) or probable COVID-19 diagnosis (ICD-10 diagnosis codes U07.2 or B97.29) in any position on the claim. Follow-up utilization is also restricted to claims coded with a confirmed or probable COVID-19 diagnosis and divided into three timeframes: a ≤30 day acute period and two post-acute periods of 31-90 days and 91-180 days. Results: During the months of March through July 2020, 42,859 patients received an initial diagnosis of COVID-19 and nearly 15% had a follow-up physician visit within the next 30 days. Of note, 2.8% or 1,211 patients sought emergency care within 30 days of their initial COVID-19 diagnosis. Almost 3% of patients had a COVID-19 related claim for a physician visit 91-180 days after their initial COVID-19 diagnosis. The most patients were diagnosed in July 2020 (N=19,106) and 18% (N=3,391) had a claim for COVID-19 related follow-up care within the next 30 days; 4% (N=742) during days 31-90, and 3% (N=591) during days 91-180. Conclusions: While the risk of hospitalization and death increases with age, young adults are not exempt from serious acute illness and/or long term COVID-19 related symptoms.
Keywords: COVID-19; Health Care Utilization; Young Adults; Claims Data
Introduction and Background
We previously reported that COVID-19 related health care utilization persists in a subset of adult patients for 180 days or more after their initial diagnosis [1]. As expected, utilization was positively associated with age [1,2]. Consistent with CDC results, recovery was not necessarily immediate or limited to self-care among young adults [3]. In this analysis, we focus on commercially insured persons aged 18-29 years who were diagnosed with COVID-19 from March 1 through July 31, 2020..
Data and Sample
We analyzed claims data of adults aged 18-29 years covered by a large national insurer with at least one day of enrollment from March 1 through July 31, 2020. As previously reported, 42,859 patients received an initial COVID-19 diagnosis out of a total of 3,791,615 members aged 18-29 years yielding a prevalence of 1.13% [1].
Study Design and Analysis
To describe utilization patterns over time, we first identified a patient’s initial health care claim coded with a confirmed (ICD- 10 diagnosis code U07.1) or probable COVID-19 diagnosis (ICD- 10 diagnosis codes U07.2 or B97.29) in any position on the claim and further categorized patients by month of initial diagnosis [4]. Follow-up utilization is also restricted to claims coded with a confirmed or probable COVID-19 diagnosis, which may miss claims related to COVID-19, but avoids including claims for completely unrelated conditions or symptoms. Follow-up was divided into three timeframes: a ≤30-day acute period and two post-acute periods of 31-90 days and 91-180 days [5]. The initial COVID-19 diagnosis date is defined as the discharge date of the initial visit/stay with a COVID-19 diagnosis; each follow-up time period does not include the initial visit/stay with a COVID-19 diagnosis. Patients can have a health care claim in each of the follow-up time periods (≤30, 31-90, and 91-180 day). Utilization that crosses time periods will only be counted in one time period (based on the start date of the visit/stay). COVID-19 diagnosis related health care related utilization is defined by an ICD-10 diagnosis code U07.1, U07.2, or B97.29 in any position on the claim.
The initial visit/stay is assigned hierarchical in the following
order: inpatient stay, emergency room (ER) visit (if occurred prior
to or on day 1 of a skilled nursing facility (SNF)/other facility visit),
other facility visit, and then physician visit. Utilization definitions
based on claims are as follows:
• If an ER visit occurs during another facility visit, then
both an ER and other facility visit are counted. ER visits are not
counted if they occur during an inpatient stay.
• Physical therapy and rehabilitation visits are counted a
maximum of 1 per 30-day period.
• Chiropractor visits are not counted towards a health care
visit.
• Any visits that were solely for the purpose of COVID-19
testing (to ensure patient no longer has COVID-19), are not
counted towards a health care visit.
• Home enteral nutrition therapy is not counted towards a
health care visit.
Results
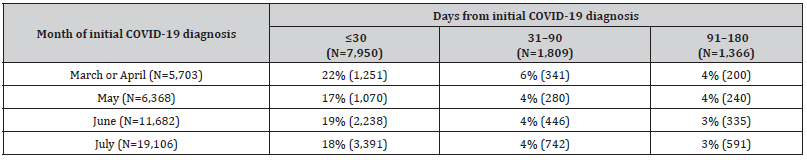
The data are broken down by month of diagnosis in Table 1 and estimates are relatively stable except for the increasing number of COVID-19 cases over time, which follows the trajectory of the pandemic in the US [6] The percentage of patients with claims for care related to their initial COVID-19 diagnosis declined in each of the three follow-up time periods from a high of 22% to a low of 3% depending on the initial month of diagnosis and length of follow-up (Table 1).
Table 1:Percent (Number) of patients with ≥1 COVID-19 diagnosis related health care claim, through 180 days: Aged 18-29 years.
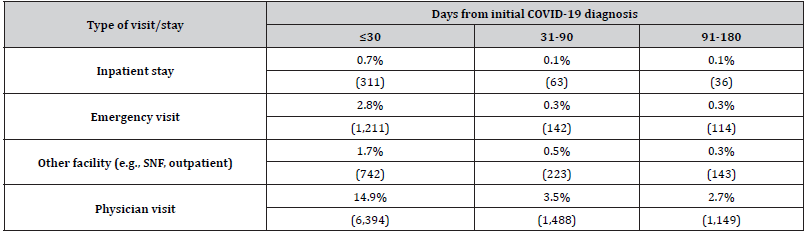
Focusing on the type of visit/stay, the majority of claims in each time frame was for a physician visit (14.9%, 3.5%, 2.7%, respectively) as shown in Table 2. Of note, 2.8% or 1,211 patients sought emergency care within 30 days of their initial COVID-19 diagnosis. Per person per month calculations reinforce that while the acute phase of illness (≤30 days) requires greater utilization of health care services (1.19 encounters per person per month), medical encounters again persist during the 31-90 day (0.62 encounters per person per month) and 91-180 day (0.39 encounters per person per month) post-acute periods.
Table 2:Percent (Number) of patients with ≥1 COVID-19 diagnosis related health care claim through 180 days by type of visit/stay for combined cohorts (March – July, N=42,859): Aged 18-29 years.
Discussion and Conclusion
While severe disease, including hospitalization and death is strongly associated with increasing Age, these data indicate that some adults aged 18-29 years’ experience symptomatic disease that may take days to weeks to months to completely recover from While severe disease, including hospitalization and death is strongly associated with increasing age, these data indicate that some adults aged 18-29 years experience symptomatic disease that may take days to weeks to months to completely recover from [2].
Acknowledgment
None.
Conflict of Interest
No conflict of Interest.
References
- Melnick G, JO Leary (2021) After their Initial Diagnosis Many Adult COVID-19 Patients Continue Seeking Medical Care up to Six Months or More. Epic Health Research Network.
- CDC (Centers for Disease Control and Prevention) (2021) Risk for COVID-19 Infection, Hospitalization, and Death by Age Group: Rate ratios compared to 18- to 29-year-olds.
- Tenforde MW (2020) Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care systems Network -United States, see also the CDC graphic “Recovery from COVID-19 can take a long time, even among young adults with no chronic conditions.” MMWR 69(30): 993-998.
- World Health Organization Emergency (2020) use ICD codes for COVID-19 disease outbreak and Centers for Medicare and Medicaid Services (CMS) New Waivers for Inpatient Prospective Payment System (IPPS) Hospitals, Long-Term Care Hospitals (LTCHs), and Inpatient Rehabilitation Facilities (IRFs) due to Provisions of Inpatient Rehabilitation Facilities (IRFs) due to Provisions of the CARES Act (https://www.cms.gov/outreach-and-educationoutreachffsprovpartprogprovider-partnership-email-archive/2020-04-15-mlnc-se).
- Datta SD, Talwar A, Lee JT (2020) A Proposed Framework and Timeline of the Spectrum of Disease Due to SARS-CoV-2 Infection: Illness Beyond Acute Infection and Public Health Implications. JAMA 324(22): 2251-2252.
-
Glenn Melnick. Health Care Utilization up to 180 Days After Initial COVID-19 Diagnosis Among a Nationwide Sample of Insured Adults Aged 18-29 Years: An Analysis of Claims Data. Cur Trends Civil & Struct Eng. 2(5): 2021. CTCMS.MS.ID.000546.
-
COVID-19, Health Care Utilization, Young Adults, Claims Data, Emergency
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






