 Case Report
Case Report
Combination of Sac packing and liquid embolization using Double Microcatheter Technique for Renal Artery Aneurysm: A Case Report
Zhilong Chen1, Haifei Wang1 and Hao Xu2*
1Department of vascular surgery, Affiliated Hospital of North Sichuan Medical College, China
2Department of Interventional Radiology, Affiliated Hospital of North Sichuan Medical College; Sichuan Key Laboratory of Medical Imaging, North Sichuan Medical College, China
Dr. Hao Xu, Department of Interventional Radiology, Affiliated Hospital of North Sichuan Medical College; Sichuan Key Laboratory of Medical Imaging, North Sichuan Medical College, China.
Received Date:January 21, 2022; Published Date: February 16, 2022
Abstract
Renal artery aneurysm (RAA) is one of the rare visceral aneurysms and has an estimated incidence of 0.1% in the general population. When the aneurysmal sac is irregular and larger than 2cm in diameter, treatment is needed for preventing its rupture. There are many methods for the treatment of RAA. Here we report the treatment of a RAA patient with a double microcatheter technique (DMT) to embolize renal hilar region aneurysm using coils and glue. Further, we also review the literature and propose that DMT is an effective and optional treatment for RAA.
Keywords: Renal Artery Aneurysm; Therapeutic Embolization; Endovascular Procedures
Introduction
Renal Artery Aneurysm, a type of aneurysms of the visceral arteries, is rare but clinically crucial vascular conditions. Most of the true visceral artery aneurysms are inherently degenerative or atherosclerotic, with histologic specimens demonstrating smooth muscle loss, elastic fibers disruption, and the arterial media’s deficiency. Visceral aneurysms mostly remain asymptomatic and are diagnosed incidentally. Visceral artery aneurysms are routinely diagnosed with ultrasound, computed tomography angiography (CTA), magnetic resonance angiography (MRA), and invasive catheter digital subtraction angiography (DSA). In this case report, we report the treatment of an RAA patient with a double microcatheter technique (DMT) to embolize renal hilar region aneurysm using coils and glue. This report also reviews the literature to elaborate on this case.
Case report
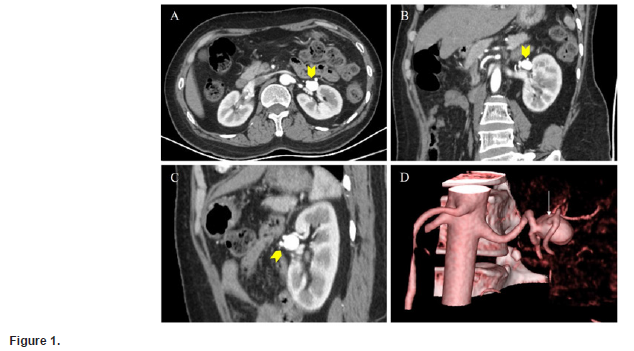
A 54-year-old woman was presented to the department of Interventional radiology for a renal artery aneurysm. She had been suffering from functional constipation and gastric polyps for the last 8 years. A month ago, she went to the outpatient clinic for help with abdominal pain. An enhanced CT scan was performed for assessing suspected intestinal obstruction. A left hilum RAA measuring 23mm × 22mm in size was diagnosed incidentally. She had no history of microbial infections such as specific viruses. CTA examination suggested a regular and round saccular aneurysm with a narrow neck and a small branch on the sac (Figure 1). The abdominal pain significantly improved after symptomatic treatment. A month later, she was presented to the department of interventional radiology for a renal artery aneurysm. Although the abdominal pain was not evidently related to the aneurysm and that there was no possibility of aneurysm rupture. However, the patient was under considerable psychological pressure and was worried about the aneurysm rupture therefore, demanded further treatment. The patient was subjected to, endovascular embolization after the multidisciplinary discussion and assessment (Figure 2).
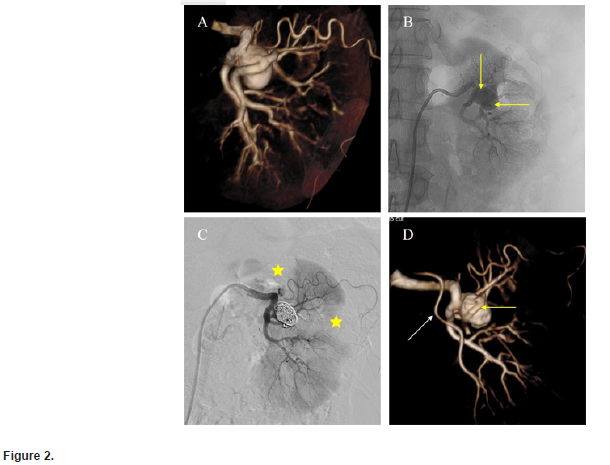
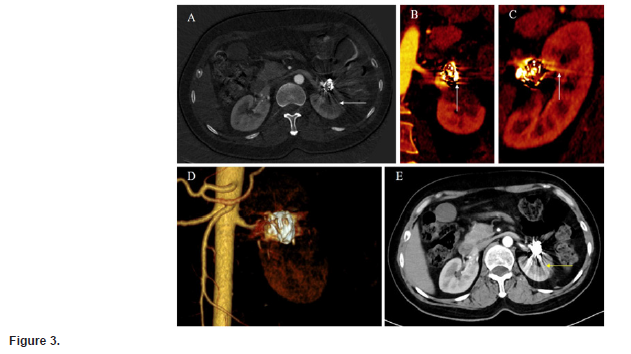
Given the small branch of the aneurysm, occlusion of the branch was not expected to cause massive infarction of the renal cortex as seen later on the follow-up of 3 months after CT (Figure 3) and serologic renal function index (Table 1). The double microcatheter technique was used for endovascular embolization after obtaining the written informed consent.
RDC (Cordis VISTA BRITE TIP) guiding catheter was placed in the main left renal artery for conventional DSA and 3D-DSA. Volume Render (VR) was then performed to formulate the protocol for the next treatment. Two microcatheters, one placed at 10 o’clock and the other at 5 o’clock, were then implanted within the aneurysmal sac using the coaxial catheter technique. First, embolization was performed simultaneously with the sac packing technique through the double microcatheter using two detachable coil embolization systems (Interlock Fibered IDC occlusion system; 0.018 inches; Boston Scientific). After releasing the coils, a mixture of iodized oil (Lipiodol; Guerbet, Roissy, France) and n-butyl-2 cyanoacrylate (Glubran 2®, GEM, Viareggio, Italy) in a 3:1 ratio (33% concentration) was embolized via the 5 o’clock microcatheter. After satisfactory embolization and filling the sac with liquid embolization agent, the glue injection was stopped and the microcatheter at 5 o’clock was pulled out. This was followed by slowly injecting an emulsion of glue and iodized oil through the microcatheter at 10 o’clock. When the liquid embolization material was filled near the sac neck, the injection was stopped and the microcatheter was pulled out 50 seconds later. Immediate angiography was performed to confirm aneurysmal sac occlusion. 3D-DSA was taken to assess the renal cortex’s infarct volume. Eventually, the residual renal preservation volume was about 90% (Figure2). There were no significant fluctuations in eGFR, Serum urea, Serum creatinine, and 99mTc-DMSA before the operation, and 1 month, and 3 months after operation (Table1).
Table 1:Pre- and post-procedural eGFR, serum parameters and 99mTc-DMSA.
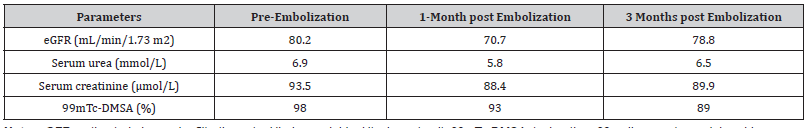
Note: eGFR: estimated glomerular filtration rate; Hb: hemoglobin; Htc: hematocrit; 99mTc-DMSA: technetium-99m dimercaptosuccinic acid.
Discussion
In clinical practice and autopsies, less than 0.1% of patients with ruptured or unruptured renal aneurysms are admitted [1], however, this can be an underestimated number. The number of such patients has recently increased owing to the use of more effective diagnostic tools such as CTA and angiography [1-3]. Though CTA and enhanced CTA have been highly sensitive, specific, and accurate in the diagnosis of vascular disease [4,5], however they do not provide a complete blood supply to the renal parenchyma of the small efferent branch of the sac. DSA, especially 3D-DSA, can provide more anatomical information for further evaluation during endovascular treatment [6]. In our center, 3D-DSA is often used as the auxiliary diagnostic tool [7].
Although renal artery aneurysm is rare, it can be life-threatening if not treated properly or intervened. The indications of RAA are still controversial [8,9]. Studies have shown that a RAA with a diameter of larger than 2cm is the critical value for intervention [8]. The detection of its size or whether there is a rupture trend seems to be a time-consuming process. Aneurysm morphology is an essential factor for immediate intervention, but the patient’s age, blood pressure, blood glucose, and childbearing age still need to be considered comprehensively [1,9-12]. RAA-related mortality may be low in the general population, however, it can be higher in emergencies, such as a sudden increase in abdominal pressure [10]. Furthermore, renal aneurysms with functional renal artery stenosis may be at higher risk [1,3,13]. However, aneurysms of any size can be treated therapeutically in cases the patients know about aneurysm in the body and they are under apsychological burden [14,15].
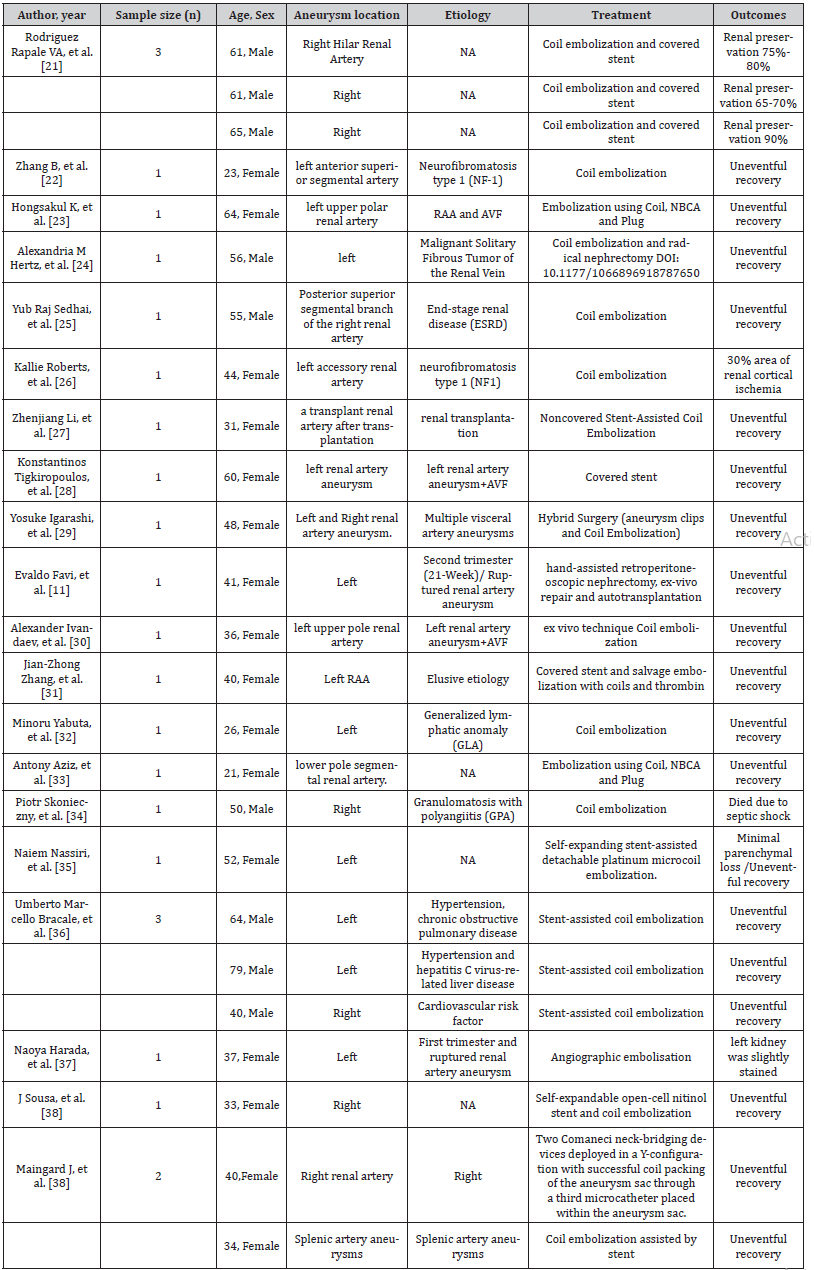
Various treatment modalities are currently employed for aneurysms. Aneurysm clipping, aneurysmal parent artery resection, angioplasty, and bypass grafting are the most classical treatment modalities with high success rates and low complications [16-20]. A review of the literature over the last 4 years shows that renal aneurysms are increasingly treated with endovascular techniques [11,21-39] (Table 2). The techniques used in endovascular therapy are varied, including endovascular coiling, remodeling techniques (such as balloon- and stent-assisted coiling), covered stent implantation, and flow diverter [8, 21,40-45]. This patient had a tortuous course of the aneurysm parent artery, and peritoneal stenting was difficult and more costly. The aneurysmal neck was narrow and the branch of the aneurysmal sac was delicate, making it unsuitable to use remodeling techniques and flow diverter. Thus, Sac packing was the best treatment option for this patient.
Table 2: Literature review of Renal Artery Aneurysm.
Nevertheless, for bi - / trifurcation aneurysms, coil embolization alone can neither achieve dense embolization nor protect small branches [45,46]. The use of microcoils and liquid embolic agent can achieve complete occlusion and aneurysm isolation. The double microcatheter technique [47], which was first applied for the treatment of intracranial aneurysms, is less risky than surgical management in treating visceral aneurysms. Further, it is cost-effective for patients who refuse open operation and are not candidates for other endovascular techniques [48]. However, extensive experience in embolizing liquid embolic materials is required to avoid reflux misembolism [49-51]. Successful cases of percutaneous direct intra-aneurysmal injection of glue or thrombin have been reported, however, they are more appropriate for superficial aneurysms and pseudoaneurysms [52-54]. Visceral aneurysms are located deeply and are difficult and risky for percutaneous thrombin and glue injection under the influence of respiration and other factors.
Imaging plays a pivotal role in detection, follow-up of RAA, but in conventional CT, the effects of beam hardening, and photon starvation make noticeable banding artifacts around the microcoils, thus seriously affecting the observation of peri-aneurysm structures and the assessment of postoperative efficacy [55,56]. The metal artifact reduction (MAR) technique can significantly reduce the metal artifact on CTA images and accurately assess the effect of intracavitary embolization of visceral aneurysms. Therefore, MAR has a high clinical application value for postoperative follow-up [57,58]. We adopted the MAR technique for follow-up observations for 3 months, and no signs of aneurysm remnants or recurrence were observed. Technetium Tc 99m dimercaptosuccinic acid (99mTc-DMSA) is a commonly used radiopharmaceutical and is equally reliable in calculating relative renal function [59]. The value of 99mTc-DMSA in this patient did not fluctuate significantly, indicating that our treatment strategy was effective and safe.
Conclusion
In conclusion, simultaneous embolization with coil and liquid embolic material via a double microcatheter is technically safe, and effective for the treatment of RAA, however, it should be carefully selected after a thorough evaluation.
Ethics
This study was approved by the Ethics Committee of the Affiliated Hospital of North Sichuan Medical College (Nanchong, China).
Consent for Publication
Written informed consent for publication of anonymized case details, which included accompanying images, was obtained from the patient.
Disclosure
The authors report no conflicts of interest in this work.
References
- Coleman DM and Stanley JC (015) Renal artery aneurysms. J Vasc Surg 62: 779-785.
- Zhang LJ, Yang GF, Qi J, Shen W (2007) Renal artery aneurysm: diagnosis and surveillance with multidetector-row computed tomography. Acta Radiol 48: 274-279.
- Gonzalez J, Esteban M, Andres G, Linares E, Martinez-Salamanca JI (2014) Renal artery aneurysms. Curr Urol Rep 15: 376.
- Albert TS, Akahane M, Parienty I (2015) An international multicenter comparison of time-SLIP unenhanced MR angiography and contrast-enhanced CT angiography for assessing renal artery stenosis: the renal artery contrast-free trial. AJR Am J Roentgenol 204: 182-188.
- Xu H, Jing C, Zhou J (2020) Application of interventional embolization in the treatment of iatrogenic pseudoaneurysms. Exp Ther Med 20: 248.
- Uricchio M, Gupta S, Jakowenko N (2019) Computed Tomography Angiography Versus Digital Subtraction Angiography for Postclipping Aneurysm Obliteration Detection. Stroke 50: 381-388.
- Liao X, Xu H, Liu F (2020) Value of Angioembolization in the Treatment of Iatrogenic Renal Vascular Injury Assisted by 3-Dimensional Digital Subtraction Angiography. Med Sci Monit 26: e927208.
- Chaer RA, Abularrage CJ, Coleman DM (2020) The Society for Vascular Surgery clinical practice guidelines on the management of visceral aneurysms. J Vasc Surg 72: 3S-39S.
- Pfister K, Kasprzak P, Oikonomou K (2018) [Management of Visceral Artery Aneurysms with Preservation of Organ Perfusion: More Than Twenty Years’ Experience]. Zentralbl Chir 143: 516-525.
- Li G, Sun Y, Song H and Wang Y (2015) Embolization of ruptured renal artery aneurysms. Clin Exp Nephrol 19: 901-908.
- Favi E, Cacciola R, Muthuppalaniappan VM, Thuraisingham R, Ferraresso M, et al. (2018) Multidisciplinary management of complicated bilateral renal artery aneurysm in a woman of childbearing age. J Surg Case Rep 2018: rjy147.
- Wang TKM, Desai MY (2020) Optimal surveillance and treatment of renal and splenic artery aneurysms. Cleve Clin J Med 87: 755-758.
- Hellmund A, Meyer C, Fingerhut D, Muller SC, Merz WM, et al. (2016) Rupture of renal artery aneurysm during late pregnancy: clinical features and diagnosis. Arch Gynecol Obstet 293(3): 505-508.
- DeFrank JT, Barclay C, Sheridan S (2015) The psychological harms of screening: the evidence we have versus the evidence we need. J Gen Intern Med 30: 242-248.
- Gillani RL, Podraza KM, Luthra N, Origitano TC, Schneck MJ (2016) Factors Influencing the Management of Unruptured Intracranial Aneurysms. Cureus 8: e601.
- Augustin G, Kulis T, Kello N, Ivkovic V (2019) Ruptured renal artery aneurysm in pregnancy and puerperium: literature review of 53 cases. Arch Gynecol Obstet 299: 923-931.
- Shirodkar SP, Bird V, Velazquez O, Ciancio G (2010) Novel management of complicated renal artery aneurysm: laparoscopic nephrectomy and ex-vivo repair with heterotopic autotransplant. J Endourol 24: 35-39.
- Abreu AL, Medina LG, Chopra S (2020) Robotic Renal Artery Aneurysm Repair. Eur Urol 78: 87-96.
- Silva NA, Shao B, Sylvester MJ, Eloy JA, Gandhi CD (2018) Unruptured aneurysms in the elderly: perioperative outcomes and cost analysis of endovascular coiling and surgical clipping. Neurosurg Focus 44: E4.
- Laser A, Flinn WR, Benjamin ME (2015) Ex vivo repair of renal artery aneurysms. J Vasc Surg 62: 606-609.
- Rodriguez Rapale VA, Martinez Trabal JL (2019) Hilar Renal Artery Aneurysm Repair Using Coil Embolization and Covered Stent. Vasc Endovascular Surg 53: 82-85.
- Zhang B, Zou Y, Yang M, Niu G (2017) Endovascular management of renal artery aneurysms induced by neurofibromatosis type 1: A case report. Medicine (Baltimore) 96: e8858.
- Hongsakul K, Bannangkoon K, Boonsrirat U, Kritpracha B (2018) Transarterial Embolization of a Renal Artery Aneurysm Concomitant with Renal Arteriovenous Fistula. Vasc Endovascular Surg 52: 61-65.
- Hertz AM, Childers CK, Wingate JT (2019) Malignant Solitary Fibrous Tumor of the Renal Vein Presenting as a Giant Renal Artery Aneurysm: A Case Report and Review of Literature. Int J Surg Pathol 27: 72-76.
- Sedhai YR, Basnyat S, Dar T, Acharya D (2019) Endovascular Treatment of Ruptured Renal Artery Aneurysm: A Case-Based Literature Review. Case Rep Med 2019: 3738910.
- Roberts K, Fan B, Brightwell R (2019) Spontaneous Accessory Renal Artery Aneurysm Rupture in a Patient With Neurofibromatosis Type 1: A Case Report. Vasc Endovascular Surg 53: 150-153.
- Li Z, Li Y, Jing Z, Feng R (2018) Endovascular Treatment for a True Aneurysm of the Transplant Renal Artery using Noncovered Stent-Assisted Coil Embolization. Ann Vasc Surg 51: 325 e325-325 e328.
- Tigkiropoulos K, Karamanos D, Stavridis K (2019) Endovascular Stent-graft Repair of Combined Renal Artery Aneurysm and Arteriovenous Fistula. Ann Vasc Surg 55: 310 e319-310 e313.
- Igarashi Y, Ohki T, Maeda K, Kanaoka Y, Chono Y (2019) Hybrid Surgery for Multiple Visceral Artery Aneurysms: A Case Report. Ann Vasc Surg 60: 478 e419-478 e424.
- Ivandaev A, Askerova A, Zotikov A, Kozhanova A, Schima W, et al. (2018) Successful surgical treatment with ex vivo technique in a patient with renal artery aneurysm rupture and bilateral arteriovenous fistula. J Vasc Surg Cases Innov Tech 4: 232-236.
- Zhang JZ, Zhang P, Wu LY (2019) Think twice before stent insertion for renal artery aneurysm with elusive etiology: a case report. BMC Surg 19(1): 154.
- Yabuta M, Nozaki T, Fukuda T, Suzuki K, Kurihara Y, et al. (2018) Generalized Lymphatic Anomaly Associated with Multiple Paraspinal Arteriovenous Malformations and Renal Artery Aneurysms. Journal of Vascular and Interventional Radiology 29: 1633-1635.e1631.
- Aziz A, Ham S (2018) Coil Embolization of a Renal Aneurysm Using a Minimally Invasive Endovascular Robotic System. Vasc Endovascular Surg 52: 207-211.
- Skonieczny P, Heleniak Z, Liberek T, Bullo Piontecka B, Bascik B, et al. (2019) Life-threatening bleeding from an aneurysm in the arcuate artery of the kidney as a rare complication of granulomatosis with polyangiitis. Pol Arch Intern Med 129: 930-931.
- Nassiri N, Huntress LA (2017) Stent-Assisted Coil Embolization of a Symptomatic Renal Artery Aneurysm at a Bifurcation Point. Ann Vasc Surg 42: 299 e211-299 e214.
- Bracale UM, Narese D, Ficarelli I (2017) Stent-assisted detachable coil embolization of wide-necked renal artery aneurysms. Diagn Interv Radiol 23: 77-80.
- Harada N, Hashimoto A, Okajima E (2017) Angiographic embolisation of a ruptured renal artery aneurysm in a primigravida during the first trimester. J Obstet Gynaecol 37: 254-256.
- Sousa J, Mansilha A (2017) Endovascular Treatment of Symptomatic Renal Artery Aneurysm with Hostile Anatomy. Eur J Vasc Endovasc Surg 53: 843.
- Maingard J, Kok HK, Phelan E (2017) Endovascular Treatment of Wide-Necked Visceral Artery Aneurysms Using the Neurovascular Comaneci Neck-Bridging Device: A Technical Report. Cardiovasc Intervent Radiol 40: 1784-1791.
- Eldem G, Erdogan E, Peynircioglu B, Arat A, Balkanci F (2019) Endovascular treatment of true renal artery aneurysms: a single center experience. Diagn Interv Radiol 25: 62-70.
- Meyer C, Verrel F, Weyer G, Wilhelm K (2011) Endovascular management of complex renal artery aneurysms using the multilayer stent. Cardiovasc Intervent Radiol 34: 637-641.
- Ginat DT, Saad WE, Turba UC (2009) Transcatheter renal artery embolization: clinical applications and techniques. Tech Vasc Interv Radiol 12: 224-239.
- Clark TW, Sankin A, Becske T, Nelson PK, Fox M (2007) Stent-assisted Gugliemi detachable coil repair of wide-necked renal artery aneurysm using 3-D angiography. Vasc Endovascular Surg 41: 528-532.
- Rezq A, Piti A, Martelli E, De Luca F, Sangiorgi G (2019) Renal artery side branches patency protection during endovascular exclusion of giant renal artery aneurysm with covered stent: Well done is better than well said. J Cardiol Cases 20: 11-13.
- Tang H, Tang X, Fu W (2018) Coil embolization of renal artery bifurcation and branch aneurysms with flow preservation. J Vasc Surg 68(2): 451-458 e452.
- Dorigo W, Pulli R, Azas L (2016) Early and Intermediate Results of Elective Endovascular Treatment of True Visceral Artery Aneurysms. Ann Vasc Surg 30: 211-218.
- Zhang Y, Gao G, Chao Y (2017) Endovascular treatment of irregular and complicated intracranial aneurysms with coils using double microcatheter technique. Exp Ther Med 13: 75-78.
- Lee BC, Kim JK, Yim NY, Kang YJ, Kim HO, et al. (2020) Endovascular treatment of wide-necked aneurysms of the visceral and renal arteries using the double microcatheter technique via a single access route. Diagn Interv Radiol 26(5): 476-481.
- Abath C, Andrade G, Cavalcanti D, Brito N, Marques R (2007) Complex renal artery aneurysms: liquids or coils? Tech Vasc Interv Radiol 10(4): 299-307.
- Elaassar O, Auriol J, Marquez R, Tall P, Rousseau H, et al. (2011) Endovascular techniques for the treatment of renal artery aneurysms. Cardiovasc Intervent Radiol 34(5): 926-935.
- Gorsi U, Chaluvashetty S, Kalra N (2020) Percutaneous glue embolization as a primary treatment for visceral pseudoaneurysms. Minim Invasive Ther Allied Technol 29(3): 170-176.
- Stolt M, Braun Dullaeus R, Herold J (2018) Do not underestimate the femoral pseudoaneurysm. Vasa 47(3): 177-185.
- Kurzawski J, Janion Sadowska A, Sadowski M (2018) A novel minimally invasive method of successful tissue glue injection in patients with iatrogenic pseudoaneurysm. Br J Radiol 91: 20170538.
- Sharma M, Somani P, Sunkara T, Prajapati R, Talele R (2019) Endoscopic ultrasound-guided coil embolization and thrombin injection of a bleeding gastroduodenal artery pseudoaneurysm. Endoscopy 51(2): E36-E37.
- Katsura M, Sato J, Akahane M (2018) Single-energy metal artifact reduction technique for reducing metallic coil artifacts on post-interventional cerebral CT and CT angiography. Neuroradiology 60(11): 1141-1150.
- Wellenberg RHH, Hakvoort ET, Slump CH, Boomsma MF, Maas M, et al. (2018) Metal artifact reduction techniques in musculoskeletal CT-imaging. Eur J Radiol 107: 60-69.
- Bier G, Bongers MN, Hempel JM (2017) Follow-up CT and CT angiography after intracranial aneurysm clipping and coiling-improved image quality by iterative metal artifact reduction. Neuroradiology 59(7): 649-654.
- Sonoda A, Nitta N, Ushio N (2015) Evaluation of the quality of CT images acquired with the single energy metal artifact reduction (SEMAR) algorithm in patients with hip and dental prostheses and aneurysm embolization coils. Jpn J Radiol 33(11): 710-716.
- Domingues FC, Fujikawa GY, Decker H, Alonso G, Pereira JC, et al. (2006) Comparison of relative renal function measured with either 99mTc-DTPA or 99mTc-EC dynamic scintigraphies with that measured with 99mTc-DMSA static scintigraphy. Int Braz J Urol 32: 405-409.
-
Zhilong Chen, Haifei Wang, Hao Xu. Combination of Sac packing and liquid embolization using Double Microcatheter Technique for Renal Artery Aneurysm: A Case Report. Curr Tr Clin & Med Sci. 3(1): 2022. CTCMS.MS.ID.000554.
-
Renal Artery Aneurysm, Interventional radiology, Saccular aneurysm, Psychological pressure, Treatment, Endovascular embolization
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






