 Case Report
Case Report
Spontaneous Rupture of a Central Neurological Bladder: A Personal Approach with a Brief Review of The Literature
Errabi Mohammed Nizar*, Krimou Hicham, Menfaa Mohamed, Sakit Fouad, and Choho Abdelkrim
Military Hospital Moulay, Ismail of Meknes, Morocco
Errabi Mohammed Nizar; Military Hospital Moulay Ismail of Meknes; Morocco
Received Date: February 17, 2023; Published Date: March 14, 2023
Abstract
Spontaneous rupture of the bladder is exceptional, with high morbidity and mortality, hence the major interest in establishing a positive diagnosis early, ensuring adequate and thorough medical resuscitation allowing a conservative treatment or leaning towards an invasive surgical approach. We report the case of a spontaneous bladder rupture in a paraplegic patient followed for central neurogenic bladder with notion of indwelling bladder catheterization. The radiological investigation revealed a large peritoneal effusion. Exploratory laparotomy revealed the presence of a perforation at the level of the bladder dome. The histological study returned positive and isolated E. Coli into the liquid as the pathogenic agent.
Keywords: Neurogenic bladder; Bladder rupture; Spontaneous; Urine peritonitis; Diagnosis, treatment, Systematic reviews
Introduction
Spontaneous rupture of the urinary bladder (SRUB) is often secondary to trauma (nearly 96.6%), with either a missed or delayed diagnosis [1]. We report a case of spontaneous bladder rupture in a paraplegic followed for central neurogenic bladder, which is only diagnosed and treated at the stage of neglected urinary peritonitis.
We report this case to highlight the major interest of the clinic and especially the imaging to make the diagnosis and then justify a conservative treatment or admit the patient to the theater for a minimal radical procedure.
Case Report:
26 yo male, paraplegic followed for central neurogenic bladder with notion of indwelling bladder catheterization. Admitted at the CHU fez, to the emergency room with fever and abdominal pain. On admission the Glasgow Score was 14/15, Blood Pressure at 8/4 cmhg, Heart Rate 110 beats/minute, venous glucose 0.92 g/liter. Clinical examination found a wooden abdomen with diffuse tenderness.
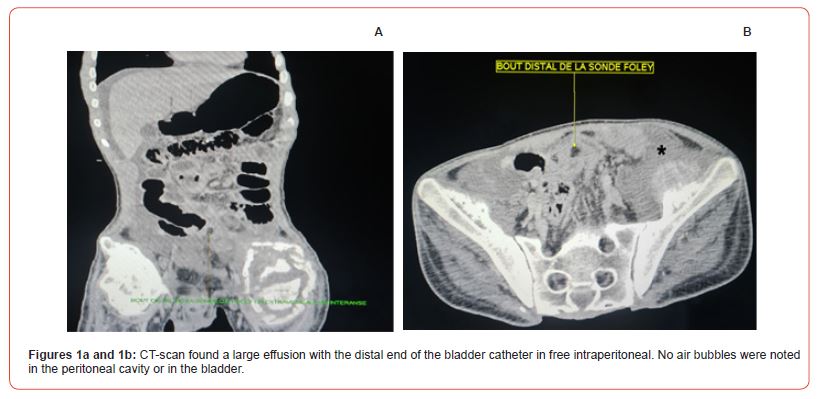
WBC at 12000 elements/mm3, C-Reactive Protein at 104, urea at 0.81 and creatinine at 12. Abdominal-pelvic Computed Tomography scan (Figures 1a-1b) found a large effusion with some slightly distended bowel (paralytic ileus), and the distal end of the bladder catheter in free intraperitoneal. No air bubbles were noted in the peritoneal cavity or in the bladder. Patient admitted to the OR for exploratory laparotomy (Figures 2a-b), who found a peritoneal cavity engorged with a fishy liquid mixed with urine, bowel distended and lined with false membranes.
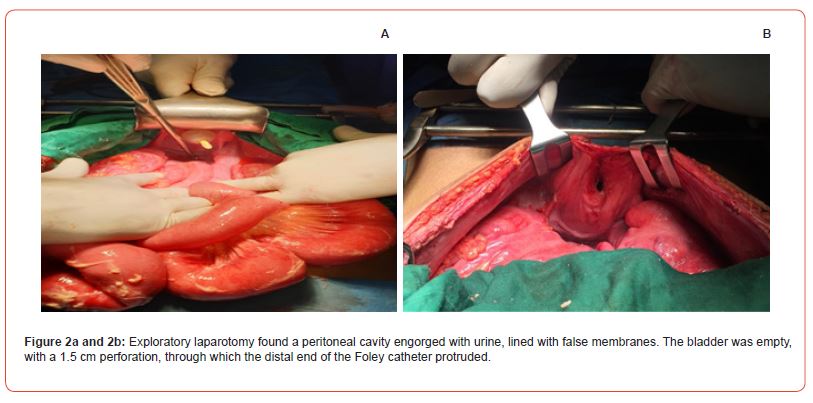
After aspiration of peritoneal fluid, the bladder was empty, with a 1.5 cm perforation, through which the Foley catheter protruded. The false membranes were resected kindly but not at all, only a peritoneal large cleaning was meticulously performed, then a flange resection was performed centered on the ostium of the bladder perforation, and finally the wall of the dome was sutured with 2/0 Vicryl in two planes without burying the sutures. The postoperative course was simple and without any particularities with recovery of transit on the third postoperative day. The histological study of the fishy liquid initially taken part; it came back positive incriminating Escherichia Coli as the pathogen in question.
Discussion
A spontaneously ruptured bladder is rare but serious with a non-negligible Morbi-mortality. Its incidence is about 1 in 126.000, less than 1% of bladder injuries [2]. Our case concerns a young adult male paraplegic followed for neurogenic bladder, admitted to the emergency room with urine peritonitis due to neglected intraperitoneal bladder rupture.
The review of the literature points out that most cases of UBRS were intraperitoneal (458 out of 713 patients), while extraperitoneal cases were less common (54 out of 713 patients), and that the majority of these patients were middle-aged men [3,5]. Most spontaneous-rupture-of-a-central-neurological-bladder spontaneous bladder rupture develops on parietal fragility following chronic and repetitive urinary retention [3,6,8]. Nevertheless, there are other predisposing factors but not commonly encountered in patients with spontaneous rupture of the urinary bladder (SRUB), including vaginal delivery, lower urinary tract obstruction, etylism, neurological, inflammatory, infectious, tumor or diverticular bladder disease [3,5,7]. In our patient, his neurogenic bladder acquired by spinal cord trauma during an Motor Vehicle Accident (MVA), alters both bladder control and bladder-sphincter coordination.
Abdominal pain is the most common sign of rupture of the urinary bladder (RUB) [4]. The same, in our case described above, where he was admitted in a state of septic shock with a wooden, contracted and painful abdomen in its entirety. Abdominal distension, urinary disorders, fever, nausea and vomiting were less frequent [3,9]. However, all of these symptoms are non-specific, making the diagnosis of RUB very delicate and delayed, even with imaging [4], which can usually only detect and quantify an intraperitoneal effusion, sometimes visualizing pneumoperitoneum or even air inside the bladder lumen. Our CT scan (Figure 1a-b) shows a very large effusion, with the distal end of the Foley catheter outside of the bladder. Once the patient was hemodynamically stabilized, he was admitted to the OR for exploratory laparotomy.
The American Urological Association (AUA) recommends urethral catheter drainage without supra-pubic cystostomy, mainly after a surgical repair of an intraperitoneal SRUB [5,9,10]. And this was the same procedure maintained for our patient. However, a recent review of the literature showed that conservative treatment could be effective in the absence of severe infection, hemorrhage or major injury [3]. Adequate urine drainage and broad antibiotic coverage are the cornerstones of conservative treatment [11,9]. The postoperative course was simple and unremarkable, with a good and normal diuresis, on its third day we noted a partial recovery of the intestinal transit. Seen again in consultation after two weeks then one month without any particularities, with a return to the previous life at the end of this last consultation [12]. Escherichia coli is the most frequently incriminated bacterium, and it is the same pathogen isolated in our patient.
Conclusion
SRUB is rare but potentially fatal, especially since its diagnosis of certainty is rather only radiological and intraoperative while the clinical-biological couple is only a potential indicator reflecting the degree of urgency and the seriousness of the disease. Thus judging the adoption of a conservative treatment or rather an imminent surgical approach. Early diagnosis and action according to the recommendations considerably reduces the morbidity and mortality rate.
Contribution of the authors
All the authors contributed to this work and read and approved the final version of the manuscript.
Acknowledgment
None
Conflict of Interest
The authors report no conflicts of interest in this work.
References
- Bacon SK (1943) Rupture of the urinary bladder: clinical analysis of 147 cases occurring over the past ten years. J Urol 49: 432-435.
- CP Peters (1989) Intraperitoneal rupture of the bladder. Urol Clin North America 16 (2): 279-282.
- Y Zhang, S Yuan, RWA Alshayyah, W Liu, Y Yu, et al. (2021) Spontaneous rupture of the urinary bladder: two case reports and review of the literature. Front Surg 2(8): 721-705.
- S Celotti, L Benuzzi, C Ceriani, P D Amore, D Foschi, et al. (2021) Laparoscopic Management for Spontaneous Bladder Rupture: A Case Report, J Surg Case Rep (1) 18;1(1): rjaa 570.
- DJ Bryk, LC Zhao, (2016) Guideline of guidelines: A Review of Urological Trauma Guidelines. BJU Int 117 (2): 226-234.
- Duenas Garcia, H Rico, V Gorbea Sanchez, T Herrerias Canedo, (2008) Bladder rupture caused by postpartum urinary retention. Obstet Gynecol112: 481-482.
- R Crawford, Oliver TRW, H Abboudi, S Shah, (2017) Spontaneous rupture of bladder during vomiting. BMJ Case Report 2016-217914.
- S Golbidi, I Laher, (2010) Bladder dysfunction in diabetes mellitus. Front Pharmacol 16(1): 136.
- RA Santucci, JM Bartley, (2010) Urologic Trauma Guidelines: A 21st Century Update. Nat Rev Urol 7(9): 510-519.
- AF Morey, JA Broghammer, CMP Hollowell, MJ McKibben, L Souter (2021) Urotrauma Guideline 2020: AUA guideline. J Urol 205 (1): 30-35.
- SB Ah, JH Ahn, (2020) Successful conservative management of spontaneous intraperitoneal rupture of the bladder diverticulum in a critical patient: about a case. An article consistent with CARE, Medicine (Baltimore) 99 (7): e19262.
- Richardson JR, Guy W, Leadbetter JR (1975) Non-operative treatment of ruptured bladder. J Urol 114 2 (2): 213-216.
-
Errabi Mohammed Nizar*, Krimou Hicham, Menfaa Mohamed, Sakit Fouad, and Choho Abdelkrim. Spontaneous Rupture of a Central Neurological Bladder: A Personal Approach with a Brief Review of The Literature. Annals of Urology & Nephrology. 3(3): 2023. AUN.MS.ID.000565.
-
Neurogenic bladder; Bladder rupture; Spontaneous; Urine peritonitis; Diagnosis, treatment, Systematic reviews
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






