 Research article
Research article
Optimized Framework for a Multidisciplinary Outpatient Clinic for Children with Elimination Disorders
Bryce A Baird1*, Haley Glasser2, Tina Solari2, Andrew A Stec2
1Department of Urology, Mayo Clinic Florida-Jacksonville, USA
2Division of Urology, Nemours Children’s Health-Jacksonville, USA
Bryce A Baird, Department of Urology, Mayo Clinic Florida 4500 San Pablo Rd Jacksonville, FL 32224, USA.
Received Date: August 09, 2022; Published Date: September 15, 2022
Abstract
Introduction: Children who have bladder and bowel elimination disorders are often treated in an inconsistent fashion by primary care providers, urologists, and gastroenterologists. Varied programs exist to treat patients with incontinence, but comprehensive care of the incontinence patient is paramount. The structure and support of the clinic allows for the treatments of pediatric patients with voiding dysfunction, urinary incontinence, fecal incontinence, failure to toilet train, chronic constipation, frequency, and urgency, recurring and persistent urinary tract infections. This project describes an optimized outpatient system that has evolved over time and currently facilitates high-level, coordinated care of pediatric patients with elimination disorders.
Materials & Methods: The described continence clinic was initiated originally with a goal to be a nurse practitioner run program to provide a dedicated place and formal process to care for pediatric patients with urinary and fecal incontinence. Over time, the structure of the program has been enhanced with additional support, providing highly efficient, comprehensive, compassionate care in this at-risk patient population. This manuscript examines the current clinical, philosophical, and administrative aspects of the continence clinic’s framework for delivering care.
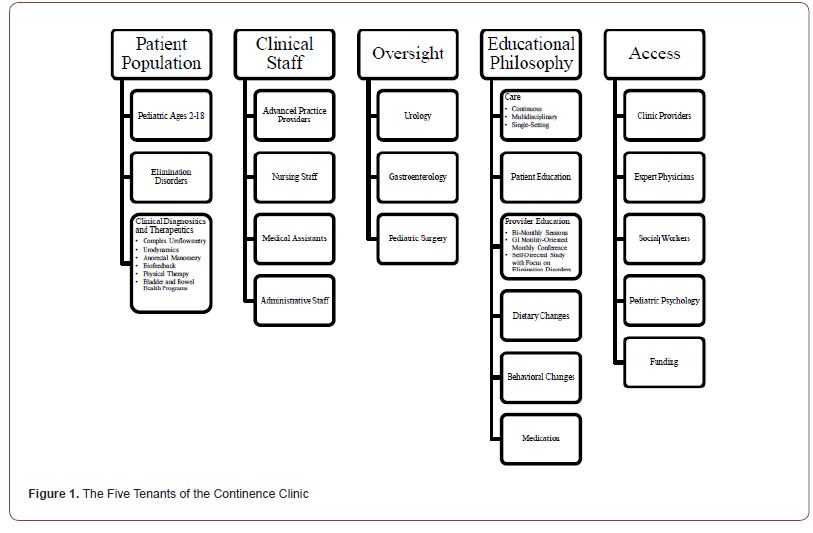
Result: The initial implementation of the continence clinic was an advance practice provider-driven (APP) response to provide thorough care for the pediatric population who dealt with incontinence. The structure of the continence clinic has evolved from this starting point and now focuses on five major elements in the delivery of this care: 1) Treat a well-defined, at-risk patient population who need educational, behavioral, dietary, and medical care to treat their bowel and bladder disorders, 2) Employ a group of dedicated advance practice providers, nurses and medical assistants for a teamwork-based approach to care, 3) Engage subject matter experts in urology, GI, and surgery to provide active support and involvement for complex cases, 4) Emphasize a continuous, educational philosophy to enhance provider knowledge base and maintain subject interest, 5) Provide accessible social workers, pediatric psychology, programmatic funding, and administration to support the clinical infrastructure.
Conclusion: A multi-disciplinary approach to bowel and bladder health is important in all patients, particularly in the pediatric-aged group. We present an advanced framework for program that optimizes the delivery of care for patients with bowel and bladder elimination disorders focusing on more than just the delivery of clinical incontinence care. Optimizing clinical operations by employing dedicated providers, team-based approaches, expert support, educational endeavors, and programmatic support elevate the continence clinic to a division level status. This framework can serve as an example for other institutions and multi-specialty practices to model care delivery in pediatric patients with dysfunctional elimination.
Keywords: Incontinence; Clinic; Bowel; Bladder; Pediatric
Introduction
Children who have bladder and bowel elimination issues are often treated in an inconsistent fashion by primary care providers, urologists, gastroenterologists, and psychologists/psychiatrists [1]. This variable approach presents a challenge to diagnosing patients and enforcing and maintaining healthy bowel and bladder habits in the pediatric population; often, a specific diagnosis is needed to ensure a solid treatment approach [2]. An organized, multidisciplinary approach is often helpful for this population, particularly due to the complex relationship between bowel and bladder habits as well as factors such as behavior [3-5].
For patients with cancer, multidisciplinary team management has been shown to reduce off-label treatments and standardize approaches; benign diagnoses such as hypertension have also shown benefit from this approach [6-8]. There is a lack of data available supporting or even outlining the ability and framework behind a multidisciplinary approach to dysfunctional elimination. In the pediatric population, 25% of patients with voiding dysfunction have been diagnosed with a neuropsychiatric disorder and more than 50% of the patients have been diagnosed with at least one negative psychosocial factor [9]. This points to a need for psychological treatment as well as social work involvement in this patient population. Additionally, the complex relationship between bowel and bladder function has been established for some time [4,10]. Available literature certainly points to the complex relationship between bowel, bladder, and behavioral function, but there is not a well-organized multidisciplinary approach to this pathology published at this time.
Many institutions and multi-specialty practices have identified a need for an incontinence clinic to treat pediatric patients with voiding dysfunction, urinary incontinence, fecal incontinence, failure to toilet train, chronic constipation, frequency, urgency, recurring and persistent urinary tract infections. Many of these clinics are primarily advance practice provider (APP) run practices acting in an adjunct fashion to a urology or GI clinic. The described continence clinic herein started similarly. Over time it has evolved to a self-supported division-level clinical program within a multispecialty practice delivering excellent care to pediatric patients with bowel and bladder disorders. This manuscript aims to describe the philosophic and structural framework of the outpatient system that makes it unique amongst continence programs.
Materials & Methods
The described continence clinic was initiated originally as an APP run program to provide a dedicated place and formal process to care for pediatric patients with urinary and fecal incontinence. Over time, the structure of the program has been enhanced with the goal of providing efficient comprehensive compassionate care in this at-risk patient population. This manuscript examines the current clinical, philosophical, and administrative aspects of the continence clinic’s framework for delivering care.
Five areas of clinical structure are (Figure 1):1) the patient population treated in the clinic and the programmatic tools used in their care; 2) the personnel who primarily comprise the clinical team and the philosophy used for care delivery; 3) subject matter experts in urology, GI and surgery to provide active support and involvement for complex cases; 4) continuous educational endeavors to enhance provider knowledge base and maintain subject interest; 5) provide accessible social workers, psychology, programmatic funding and administration to support the clinical infrastructure in a division-type style (Figure 1).
The continence clinic is comprised of APPs, nursing staff, physicians, and other clinical staff. The clinic is open 5 days per week and provides services to patients aged 2-18 years. The clinic was developed using staff and tools which were readily available. It was organized into a more official clinic and developed into a fulltime clinic. The resources and staff utilized are financially feasible and operates through existing facilities and support.
Result
The primary cornerstone that is kept at the forefront of the clinical structure is the patient population that is served. The continence clinic cares for pediatric patients ages 2-18 who have issues with bladder dysfunction, bowel dysfunction, incontinence and a myriad of other specific diagnoses that fall under these categories. Patients are often diagnosed with an elimination problem by a pediatrician, pediatric gastroenterologist or pediatric urologist and then referred to the continence clinic. The patients have frequently failed basic maneuvers to try and cure these conditions, and they need intensive patient and caregiver education, behavioral modifications, dietary modifications, and the use of medications and physical therapies in the treatment plan.
Within the framework of the clinical structure, the continence clinic also employs therapies and testing housed within the clinical structure to help patients. Complex uroflowmetry, urodynamics, anorectal manometry, biofeedback and physical therapy, and nurse run intensive healthy bladder and healthy bowel programs are employed.
Additionally, the clinic houses other subspecialty clinics within its framework. Most notably, the continence clinic is the site of a monthly multidisciplinary spinal defect clinic. Patients with spinal defects often have a range of bladder and bowel dysfunction. Thus, the continence clinic is set up to accommodate this patient population as well.
The makeup of the clinic is currently with 3 full-time advance practice providers in clinic five days a week. Five full days of telehealth care is provided concomitantly to in clinic, in person care. Two dedicated registered nurses and two dedicated medical assistants round out the primary clinical team. The primary tool employed in treatment is a multi-level approach to patient and caregiver education. Every employed clinical member of the continence team is involved in the care plan and provides continuous education opportunities during the clinical encounters, from check in, through rooming, testing, the clinical encounter, and checkout. Involving every team member at every level is instrumental at immersing the patient and family in the needed knowledge to obtain the desired therapeutic outcomes.
The primary philosophical goals of the clinic revolve around being the principal caregiver for the pediatric population dealing with bowel and or bladder dysfunction. In a single setting, multidisciplinary care is provided to pediatric bowel and bladder pathologies while employing advanced diagnostic and therapeutic tools. The clinic aims to improve both the patient and parent quality of life while providing continuity of care and follow-up for all patients seen in the clinic.
The continence clinic is supported by subject matter experts, while also maintaining the APP-driven clinical structure. A pediatric urologist with an interest in continence issues, a GI physician with expertise in motility disorders and a pediatric surgeon with surgical expertise in the treatment of anorectal malformation and constipation all support the clinic. This support is provided by several strategies including, clinical advice, patient co-management and a free flow of patients between specialty clinics when needed. The emphasis of this subspecialty physician involvement is that to provide active support while allowing the clinic to be APP driven.
Education is also actively encouraged. Bi-monthly dedicated education sessions with additional monthly GI motility-oriented conference are provided and run by the supporting physicians. These education sessions vary from topic-based presentations, difficult case discussions, literature review, and self-directed learning. This enhances provider knowledge base and maintains subject level interest.
Finally, the clinic is treated as a division-level program within the multi-specialty clinic. Operations are overseen by a physician chief, lead administrator and a nurse manager. It is a budgeted unit that maintains fiscal profitability. The continence clinic has standalone dedicated space for its clinical operations and receives the same institutional support as a small division. Additional support occurs for patient care with the involvement of social work as well as psychology and physical therapy.
Discussion
This model for the delivery of care to an at-risk model is a highly successful and reproducible clinical care pathway. The population is one of need as it consists of pediatric patients, patients with incontinence, patients needing increased time and education, and patients who have multi-factorial reasons for their disorders. Not only using a primarily APP-run clinic, but also employing nurses and medical assistants to care for the patient provides multi-layered care. At the same time, it is important for adequate physician support to maintain education of patients and support staff, be a resource for complex patients, and maintain clinic efficiency. Administrative and nursing supervisor support maintain resources and budgetary effectiveness. Overall, treating the continence clinic as a small division as opposed to a subgroup of a specialty, like urology, has led to a very successful clinical venture.
The overall success comes from the infrastructure that allows all care team members to be a part of the plan without one more important than another. By all metrics available, the continence clinic is highly successful. It is fiscally solvent and meets its budgetary obligations. Approximately 4000 patient visits, with 900 new patients were conducted this past year. Patient satisfaction metrics all sit about the 90th percentile compared to national benchmarks, and internal employee engagement results are some of the highest in our multi-specialty practice.
The people involved in this clinical endeavor are also all passionate about their clinical roles. Motivated APPs with a desire to impact a specific population are paramount. Their hard work needs adequate support. However, ownership over patient care is kept primarily at a clinic level. Engaged physicians, as subject matter experts, provide both clinical expertise and continuing education and are clearly necessary for success. Subspecialty practices do not exist in isolation, and the team is of paramount importance at every level. Currently, this clinical model is being expanded to additional remote clinical sites in our enterprise.
Voiding disorders are multifactorial in nature and require a compassionate approach to treatment. As an APP-led initiative, the standards of care for nurse practitioners (NPs) are at the forefront of the Continence Clinic’s philosophy. These tenets, as outlined by the American Association of Nurse Practitioners (AANP), include patient and family education, shared decision making, promotion of a safe environment, and interprofessional/collaborative responsibility [11]. Emphasizing these care priorities has been effective at addressing the physical, mental, and social needs of the clinic’s patient population. This NP-driven framework allows for increased accessibility to care and comprehensive visits that focus on education and health promotion. Ample time is spent with each patient to ensure the creation of sustainable and holistic treatment goals. Patients are monitored closely and are encouraged to maintain open communication with their provider in case adjustments to the treatment plan is needed.
Limitations of this specific study include a lack of clinical data; however, this study is primarily offered as a framework for other clinics. Further studies on outcomes of patients within the ‘continence clinic’ will be perused and are outside the scope of this paper’s aim. There are obvious biases involved in this clinic. By nature, our facility is set up to filter patients with elimination problems to our ‘continence clinic.’ Other facilities that do not have a clinic such as this will take time to develop a referral pattern. Additionally, providers will learn how to facilitate the treatment of the elimination disorders within the specific clinic designed for this goal.
Through the efforts of a team comprised of nurse practitioners, physician oversight, nursing, psychology, and medical assistant team, our incontinence clinic has accomplished seeing hundreds of patients with bowel and bladder emptying disorders. This multidisciplinary clinic functions to treat urinary and fecal elimination problems. It focuses on behavioral modifications, dietary modifications, and medications. A streamline treatment plan along with a well-organized treatment team benefits patients, providers and other staff involved in patient care. A system such as the one presented in this article can be utilized to make care more efficient for all parties involved. With structure in place, patients can receive a standardized approach and treatment that can be implemented in a quick, effective fashion.
Conclusion
A multi-disciplinary approach to bowel and bladder health is important in all patients, particularly in the pediatric-aged group. We present an advanced framework for a program that optimizes the delivery of care for patients with bowel and bladder elimination disorders focusing on more than just the delivery of clinical incontinence care. Optimizing clinical operations by employing dedicated providers, team-based approaches, expert support, educational endeavors, and programmatic support elevate the continence clinic to a division level status. This framework can serve as an example for other institutions and multi-specialty practices to model care delivery in pediatric patients with dysfunctional elimination.
Acknowledgement
None.
Conflicts of Interest
No conflicts of interest.
References
- Gontard AV, E Kuwertz-Broking (2019) The Diagnosis and Treatment of Enuresis and Functional Daytime Urinary Incontinence. Dtsch Arztebl Int 116(16): P 279-285.
- Santos JD, RILopes, MA Koyle (2017) Bladder and bowel dysfunction in children: An update on the diagnosis and treatment of a common, but underdiagnosed pediatric problem. Can Urol Assoc J 11(1-2Suppl1): PS64-S72.
- Halachmi S, WA Farhat (2008) Interactions of constipation, dysfunctional elimination syndrome, and vesicoureteral reflux. Adv Urol 2008: 828275.
- Kaplan SA, R Dmochowski, B D Cash, Z S Kopp, S J Berriman, et al. (2013) Systematic review of the relationship between bladder and bowel function: implications for patient management. Int J Clin Pract 67(3): 205-216.
- Jarczyk KS, Pam Pieper, Lori Brodie, Kelly Ezzell, Tina D'Alessandro (2018) An Integrated Nurse Practitioner-Run Subspecialty Referral Program for Incontinent Children. J Pediatr Health Care 32(2): 184-194.
- Sim TA, Joyner, (2002) A multidisciplinary team approach to reducing medication variance. Jt Comm J Qual Improv 28(7): 403-409.
- Adorian D (1990) Group discussions with the health care team-a method of improving care of hypertension in general practice. J Hum Hypertens 4(3): 265-268.
- Stephens MR, W G Lewis, A E Brewster, I Lord, G R J C Blackshaw, et al. (2006) Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus 19(3): 164-171.
- Logan BA, Katiuscia Correia, Jenna Mc Carthy, Mary Jo Slatterye (2014) Voiding dysfunction related to adverse childhood experiences and neuropsychiatric disorders. J Pediatr Urol 10(4): 634-638.
- Grundy L , SM (2018) Brierley Cross-organ sensitization between the colon and bladder: to pee or not to pee? Am J Physiol Gastrointest Liver Physiol 314(3): G301-G308.
- Practicioners, AAoN Standards of practice for nurse practioners. 2019 2022]; Available from: www.aanp.org/advocacy/advocacy-resource/position-statements/standards-of-practice-for-nurse-practitioners.
-
Bryce A Baird*, Haley Glasser, Tina Solari and Andrew A Stec. Optimized Framework for a Multidisciplinary Outpatient Clinic for Children with Elimination Disorders. Annal Urol & Nephrol. 3(1): 2022. AUN.MS.ID.000559.
-
Incontinence, Clinic, Bowel, Bladder, Pediatric
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






