Case Report
Case Report
Extra Scrotal Spermatocele – A Unique Case Presentation & Brief Review of literature
Iqbal Singh1*, Aravind TK2, Dibya Priyadarsini Behera 3, Deep Patel4 and Natasha Panesar5
1M. Ch (Urology), DNB, MS, Professor (CAS), Department of Surgery (Urology), University College of Medical Sciences (University of Delhi) & GTB Hospital, ORCID ID: https://orcid.org/0000-0001-8743-3404
2MBBS, Post Graduate Junior Resident, Department of Surgery, University College of Medical Sciences (University of Delhi) & GTB Hospital, ORCID ID: https://orcid.org/0000-0002-6501-5014
3MBBS, Post Graduate Junior Resident, Department of Surgery, University College of Medical Sciences (University of Delhi) & GTB Hospital, ORCID ID: https://orcid.org/0000-0001-7672-904X
4MBBS, Post Graduate Junior Resident, Department of Surgery, University College of Medical Sciences (University of Delhi) & GTB Hospital
5MBBS, Hamdard Institute of Medical Sciences & Research (HIMSR), ORCID ID: https://orcid.org/0000-0002-8630-4544
Iqbal Singh, M. Ch (Urology), D.N.B (GUSurg), MS, DNB (Surg) Fellowship (Robotics & Minimally Invasive Urology), WFUMS, NC, USA. Professor& Senior Consultant Urologist, Department of Surgery, University College of Medical Sciences, (University of Delhi).F-14 NDSE-2, New Delhi-110049. India.
Received Date: October 04, 2020; Published Date: November 12, 2020
Abstract
Background: Spermatoceles are extra testicular lesions caused by cystic dilation of the efferent ductules filled with clear/milky fluid containing spermatozoa usually diagnosed incidentally either as a scrotal swelling or by ultrasonography. Suspecting and diagnosing spermatoceles presenting at extra scrotal positions is extremely rare and very few cases have been described in literature thus far. This article attempts to depict a patient presenting with one such spermatocele at an unusual location which adds to the scarce literature on the subject.
Case Presentation: A 60-year-old male presented with complaints of a gradually progressing left inguinal swelling for past 3 months with prior trivial scrotal trauma. Clinical evaluation and investigations revealed a 5 × 3 cm inguinal swelling extending up to the superior aspect of the left hemiscrotum that was confirmed as a spermatocele on pathological analysis at an unusual extra scrotal location.
Conclusion: Spermatoceles presenting at extra scrotal locations are extremely rare occurrences as is evident by the scant available published literature. This report adds to the scarce literature and also alerts the practicing urologist/surgeon towards insisting on a complete physical examination including simple but effective examination techniques like the transillumination technique as an aid to diagnosis of spermatoceles that may present uniquely at uncommon (extrascrotal) locations as in the present case.
Keywords: Extrascrotal; Inguinal; Spermatocele; case report
Abbreviations: FNAC: Fine Needle Aspiration Cytology; OPD: Outpatient Department
Introduction
Spermatoceles are usually asymptomatic and rarely cause clinical problems like disturbing pain and infertility. Self -examination and physical examination are the most common ways spermatoceles are detected. They are frequently seen on scrotal ultrasound as an incidental finding usually being located within scrotum cephalic and occasionally posterior to the testis [1]. Case reports of spermatoceles presenting at unusual locations are extremely rare with an extensive literature search revealing only 3 such cases which are depicted in Table 1 [2-4]. This case hence adds to the scarce literature on spermatocele with unusual presentations (Table 1).
Table 1:Reported Cases of Spermatoceles Presenting at Unusual Locations.

Case Presentation
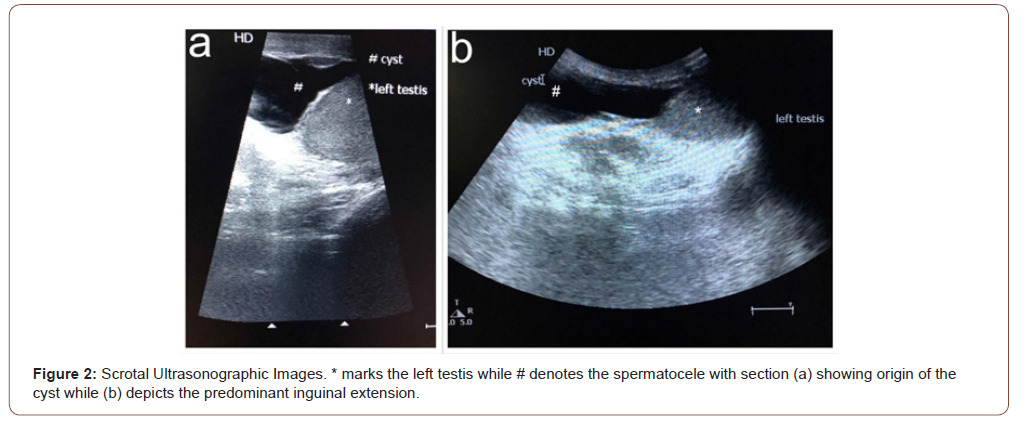
60-year-old male presented to surgical OPD with complaints of a gradually progressing painless left inguinal swelling for 3 months following history of trivial blunt scrotal trauma without any urinary/ sexual complaints. The patient was initially managed as a case of chronic epididymitis by a private practitioner with medications and reported to our clinic due to lack of improvement from the prior treatment. Physical examination revealed approximately 5 × 3 cm inguinal swelling extending up to the superior aspect of the left hemiscrotum (Figure 1). Bilateral testicular, scrotal, and abdominal examination was unremarkable. Ultrasonography suggested a hypoechoic lesion with low-level echogenicity and irregular walls abutting the left testis with superior extension into the inguinal region (Figure 2). FNAC of the cystic lesion revealed clear fluid with mature spermatozoa that confirmed the diagnosis of a spermatocele with predominant extra scrotal location (Figures 1,2).

Discussion
Spermatoceles are extra testicular lesions caused by cystic dilation of the efferent ductules filled with clear/milky fluid containing spermatozoa. They are generally found incidentally as single, unilateral, and mostly asymptomatic swellings [5]. The exact aetiology of spermatocele still remains obscure with the proposed hypothesis being shedding of senile seminiferous cells leading to obstruction and dilatation of the efferent ducts [6]. Spermatoceles are well characterized on ultrasonography, appearing as hypoechoic lesions with posterior acoustic enhancement and confirmed by Fine needle cytology which reveals cyst fluid-filled with mature spermatozoa [7]. Most spermatoceles are managed conservatively unless they are persistently symptomatic or when they trigger doubts of malignancy in which case they are managed by spermatocelectomy. Sclerotherapy using ethanolamine oleate forms another effective and safe therapeutic alternative to surgery with minimal side effects and low recurrence. Sclerotherapy in younger men is avoided owing to the danger of epididymitis and resulting infertility [8]. The patient was managed conservatively owing to a lack of distressing symptoms with FNAC proving partially therapeutic causing more than 50% reduction in swelling size and is currently on periodic clinical follow-ups.
Conclusion
Spermatoceles occurring at extra scrotal locations are extremely rare occurrences as is evident by the scant published literature. This report adds to the scarce literature and serves to alert the practicing urologist-surgeon to maintain a vigilant eye for abnormal presentations of a common disease by persistent usage of simple but effective physical examination techniques like the transillumination technique and scrotal ultrasonography which must be considered in the examination of all inguinal/ inguinoscrotal swellings keeping extra scrotal spermatoceles in the list of differential diagnosis.
Acknowledgement
None.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this case report.
References
- Rioja J, Sánchez-Margallo FM, Usón J, Rioja LA (2011) Adult hydrocele and spermatocele. BJU Int 107(11): 1852-1864.
- Ansari S, Shaikh TP, Thahir VU, Mandhane N, Deolekar S, et al. (2015) A rare extra scrotal spermatocele: a rare case presentation. Int J Res Med Sci 3(8): 2141-2142.
- Davis RS (1998) Intratesticular spermatocele. Urology 51(5A Suppl): 167-169.
- Dollard DJ, Fobia JB (2011) Extra scrotal spermatocele causing lower abdominal pain: a first case report. Am J Emerg Med 29(3): 358.e7-357.e9.
- Clarke BG, Bamford SB, Gherardi GJ (1963) Spermatocele: pathologic and surgical anatomy. Arch Surg 86: 351-355.
- Itoh M, Li XQ, Miyamoto K, Takeuchi Y (1999) Degeneration of the seminiferous epithelium with ageing is a cause of spermatoceles. Int J Androl 22(2): 91-96.
- Rifkin MD, Kurtz AB, Goldberg BB (1984) Epididymis examined by ultrasound. Correlation with pathology. Radiology 151(1): 187-190.
- Tammela TL, Hellström PA, Mattila SI, Ottelin PJ, Malinen LJ, et al. (1992) Ethanolamine oleate sclerotherapy for hydroceles and spermatoceles: a survey of 158 patients with ultrasound followup. J Urol 147(6): 1551-1553.
-
Iqbal Singh, Aravind TK, Dibya Priyadarsini Behera, Deep Patel. Extra Scrotal Spermatocele – A Unique Case Presentation & Brief Review of literature. Annal Urol & Nephrol. 2(2): 2020. AUN.MS.ID.000535.
-
Extrascrotal, Inguinal, Spermatocele, case report, Scrotum cephalic, Occasionally posterior, Left hemiscrotum, Low-level echogenicity, Hypoechoic lesion
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.