 Research Article
Research Article
Exstrophy Epispadias Complex: Outcome Analysis of Repair Performed at A Single Centre
Mukesh Chandra Arya1, Vivek Vasudeo2*, Yogendra Shyoran2, Abhiyutthan Singh Jadaon2, Manoj Kumar Garg3, Ankur Singhal2 and Ajay Gandhi2
1Professor and head, Department of urology, Sardar Patel Medical college, Bikaner, Rajasthan, India
2Department of urology, Sardar Patel Medical College, Bikaner, Rajasthan, India
3Consultant plastic surgeon, Ganganagar, Rajasthan, India
Vivek Vasudeo, Department of urology, Sardar Patel Medical College, Bikaner, Rajasthan, 334001, India.
Received Date: February 11, 2021; Published Date: March 24, 2021
Abstract
Objective: The exstrophy-epispadias complex (EEC) is a rare developmental defect which affects multiple systems including the genitourinary system. We share our outcome analysis of 34 surgeries performed on 27 EEC cases at our institution.
Material and Methods: This is a retrospective analysis of the outcome and follow up of patients operated for EEC. A total of 27 cases including 15 bladder exstrophy (11 Males, 4 Females) and 19 epispadias (14 Males, 5 Females) were treated from September 2014 to November 2019. Total 34 surgeries were performed on 27 patients which included 7 male cases of closed exstrophy who underwent subsequent epidpadias repair. These included two interesting exstrophy cases also. One of them was a female bladder exstrophy reared as male up to 19 years and another a 31 years male with skin covered exstrophy, diphallia and total urinary incontinence since birth. Epispadias group also included two adult males.
Result: Thirteen pediatric patients underwent primary bladder and abdominal closure. Bladder reclosure rate was 14.2%. One adult male underwent Mitrofanoff diversion. The other adult- 19 year female had bladder closure, followed by bladder augmentation and rectus flap interposition. Male epispadias repair was performed in 14 patients (7 post closed exstrophy and 7 epispadias). Fistula rate after male epispadias repair was 15.3%. Five females underwent repair for epispadias. Bladder neck reconstruction (BNR) was carried out in 6 patients. Continence rates post BNR was 83% (including social continence).
Conclusion: This congenital anomaly requires accomplishment of meticulous repair in staged manner. These cases need follow up from birth to adulthood. Presentation at adult age is extremely rare and related to social stigma, illiteracy and poor access to health care system.
Keywords:Bladder exstrophy; Epispadias; Bladder neck reconstruction; Urinary incontinence; Genitoplasty
Abbreviations: EEC: Exstrophy- epispadias complex; BNR: Bladder neck reconstruction; IPGAM: Incorporated Glanuloplasty and advancement meatal; CBE: Classical bladder exstrophy; CPRE: Complete primary repair of exstrophy; MSRE: Modern staged repair of exstrophy; VUR: Vesicoureteric reflux; SPCL: Suprapubic Cystoloithotomy; CIC: Clean intermittent catheterisation; IVU: Intravenous Urography; BSRI: Bem sex role inventory; SP: Suprapubic; GIDYQ-AA: Gender Identity/ Gender dysphoria questionnaire for adolescent and adults
Introduction
The exstrophy-epispadias complex (EEC) is a rare congenital disorder involving multiple systems. It includes a spectrum from epispadias, classical bladder exstrophy (CBE) to cloacal exstrophy with ascending complexity. CBE is the most common type, with incidence of one per 10,000 to 50,000 births and twice more prevalent in males [1,2]. Risk factors for CBE include Caucasian race, young maternal age, multiparity and children born after in vitro fertilization [3,4]. The purpose of this paper is to analyse our clinical data and results of 27 exstrophy epispadias males and females, with wide variety, presenting at different ages including four adults. CBE can be repaired by either the modern staged repair of exstrophy (MSRE) or complete primary repair of exstrophy (CPRE) in a single stage. The first step of repair (in MSRE) is closure of the bladder and abdominal wall, effectively converting CBE into complete epispadias with incontinence. Malleability of pelvic bones aids in sound abdominal wall repair if carried out within 72 hours of birth. This repair with balanced posterior outlet resistance is very crucial for decreased inflammation, fibrosis, improved bladder growth and decreased need for urinary diversion [5]. Tension free closure and pelvic immobilisation are vital for success [6]. Genitoplasty and urethroplasty are accomplished in females in the first stage. The second stage in males is closure of epispadias with a modified Cantwell-Ransley repair at 6 to 12 months of age. This procedure promotes bladder growth and capacity, critical for continence. Cantwell et al first described the technique of ventral urethral transposition for epispadias in 1895 in two cases [7]. Modified Cantwell technique was originally described by Ransley et al to attain good functional and cosmetic outcome [8]. It consists of partial disassembly of corporal bodies, urethroplasty and Ransley incision and suturing corpora in midline resulting in medial rolling of corporeal bodies [9]. Incorporated Glanuloplasty and advancement meatal (IPGAM) technique helps to attain orthotopic meatal position [10]. Female epispadias repair incorporates urethroplasty, genitoplasty (monsplasty and clitoroplasty) and bladder neck repair performed in one or two stages [11]. In the third stage, Young-Dees-Leadbetter bladder neck reconstruction (BNR) is performed to achieve continence provided patient achieves adequate bladder capacity (usually at the age of 5-9 years). This stage is combined with bilateral ureteral reimplantation to correct vesicoureteric reflux (VUR).
Materials and Methods
Ethical approval for the study was obtained from the Institutional Ethical Committee. Informed consent was obtained from all individual participants or parents for whom identifying information was included in this article. We retrospectively reviewed the data of EEC cases managed at our institution from September 2014 to November 2019. Age, sex, surgical procedures at different stages, complications and follow up were recorded from a prospectively maintained EEC registry. A total of 27 cases were managed including 15 bladder exstrophy and 19 epispadias. None of these had a prenatal diagnosis or born after invitro fertilisation. Associated anomalies in pediatric CBE patients included inguinal hernia in three (bilateral in one), rectal prolapse in two and right undescended testis in one. All surgeries were performed by a single surgeon MC Arya. All patients underwent routine blood biochemistry and ultrasound KUB. All bladder exstrophy cases were neonates or infants except two interesting cases. First was a female who was reared as male up to 19 years and another a 31 years male with skin covered exstrophy, diphallia and total incontinence. Our approach to all exstrophy patients was MSRE except in the two adult cases. Out of 19 epispadias cases 14 were males and 5 females. Female epispadias cases were classified according to Davis classification[12].
Surgical techniques
Exstrophy closure
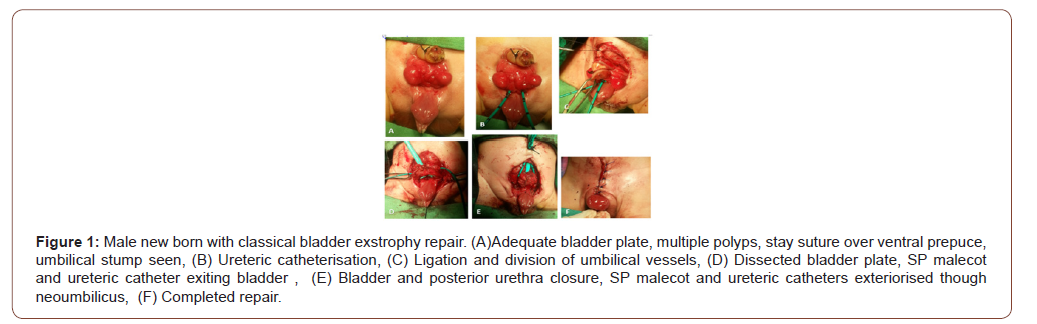
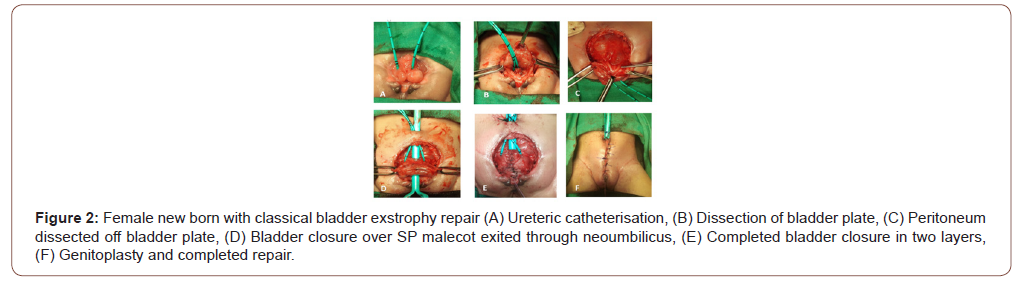
Bladder, posterior urethra and abdominal wall closure were done in first stage at presentation as the bladder plate was adequate and there was no hydronephrosis. Key steps in this repair were bilateral ureteral cannulation, adequate mobilisation of bladder template by sharp dissection, division of urogenital diaphragm and approximation in midline, creation of neoumbilicus, approximation of symphysis pubis and application of Bryant’s traction postoperatively (Figure 1). Female exstrophy closure also included genitoplasty (Figure 2).
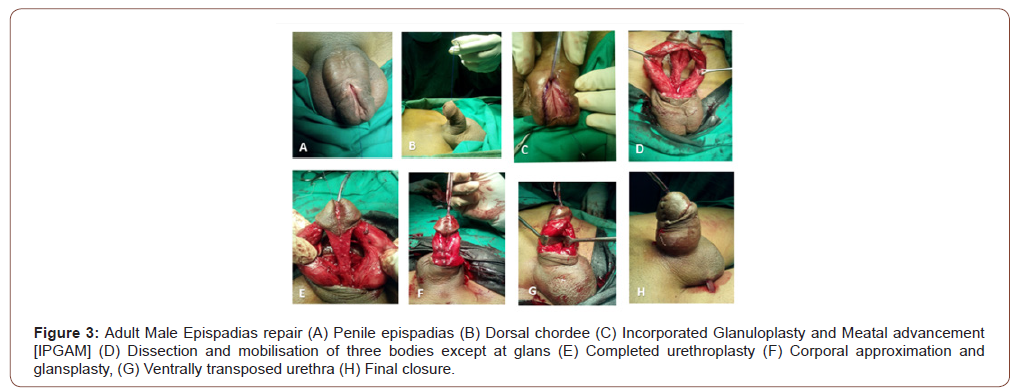
Male epispadias repair
This was done in second stage at 6 months to 1 year. The procedure adopted was slightly different from modified Cantwell Ransley procedure in the way that the urethral plate was mobilised off the corpora except at the glans. This facilitated transposition of urethra ventrally and closure of urethral plate in two layers thereby reducing fistula incidence (Figure 3). Further this allowed better medial rotation of corpora after Ransley incision to correct chordee. Partial disassembly also avoids hypospadiac meatus, a common complication of complete dissesembly (Mitchell). Glansplasty was followed by dorsal transposition of ventral prepuce by Byar’s flap. In all cases, the neurovascular bundles were identified, isolated and preserved to prevent glans necrosis.
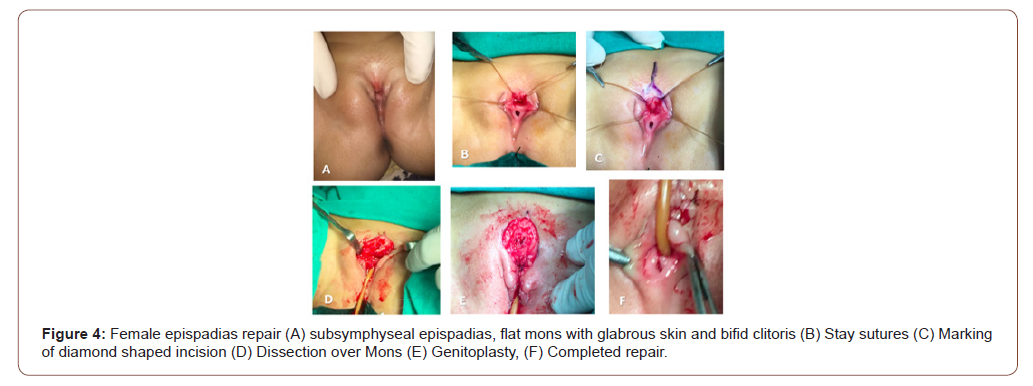
Female epispadias repair
Flat mons, bifid clitoris and patulous or dorsally split urethra are the hallmarks of female epispadias. Glabrous skin of mons pubis was excised, subcutaneous fat was mobilised from both sides and brought in midline. After applying stay sutures, dorsally a wedge of redundant tissue was excised to narrow urethra. Urethra was reconstructed over 10 F Foley catheter using 6-0 polydioxanone. Medial side of clitoris and labia minora were denuded and closed over neourethra (Figure 4).
Bladder neck reconstruction (BNR)
It was done only after attainment of good bladder capacity judged by cystogram. Bladder was opened vertically with distal transverse extensions. Modified Cohen’s ureteric reimplantation was undertaken. Posterior urethral strip (30*15 mm) was marked before tubularisation over 8 Fr infant feeding tube followed by double breasting of detrusor over it. After this, the bladder neck repair was suspended to rectus fascia. Suprapubic catheter and infant feeding tube were kept for 3 weeks. Inguinal hernia was repaired after one month of first stage. Rectal prolapse was dealt with sclerosant injection by pediatric surgeon. Orchiopexy for undescended testis was performed around one year of age. Some cases didn’t turn up after first /second stage repair, possibly went elsewhere and lost to follow up.
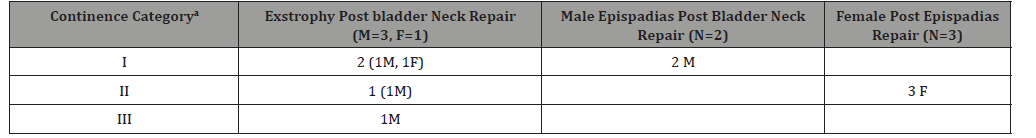
Continence was a continuous evaluation at follow ups as it improves with time. The status at last follow up was mentioned in the results. We used the criteria laid by Baird et al to measure our continence outcome. Baird et al divided their BNR results in three groups. First group being voiding per urethra with dry periods greater than 3 h with controlled spontaneous voiding during the daytime, and dry at night without bladder augmentation or intermittent catheterization. The second and third groups were patients with social continence (defined as dry for periods of 3 h during the day but damp at night) and wet group (dry interval < 3hrs) respectively [13]. The same categories are used in Table 4.
Result
Table 1:Exstrophy Epispadias Complex spectrum.
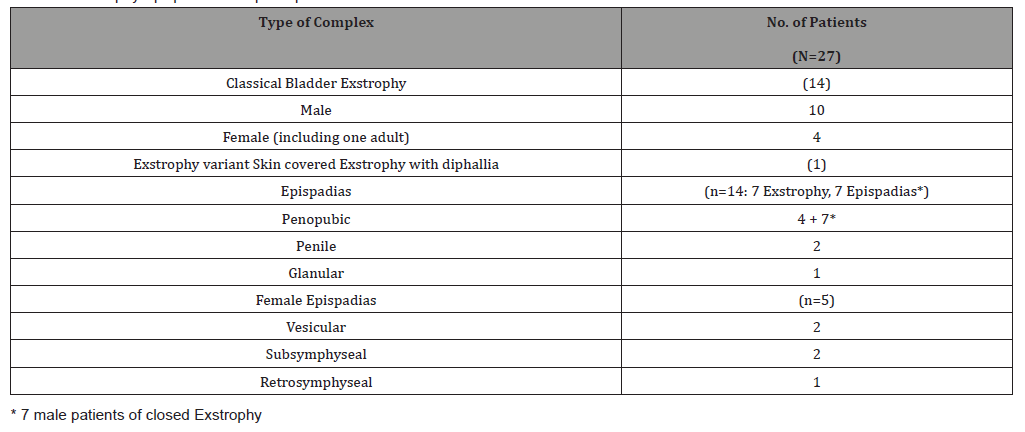
Table 2:Surgeries performed and associated complications.
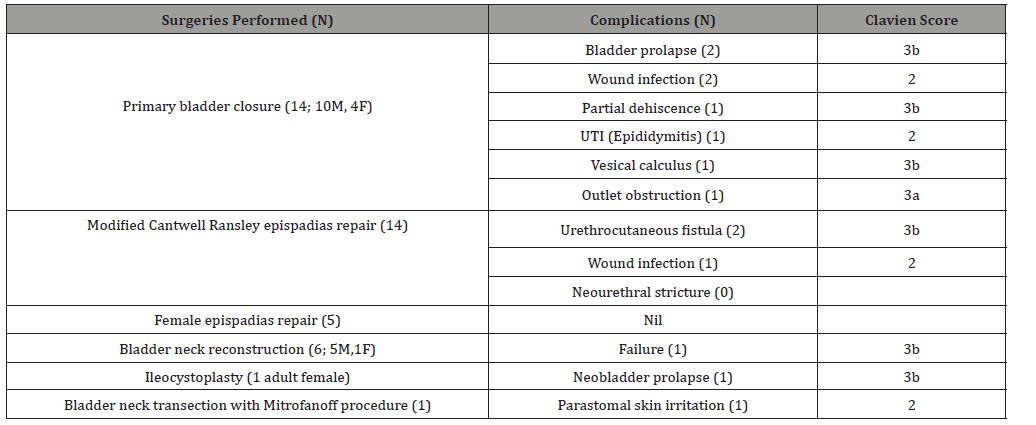
Table 3:Ages at different repairs and follow up.
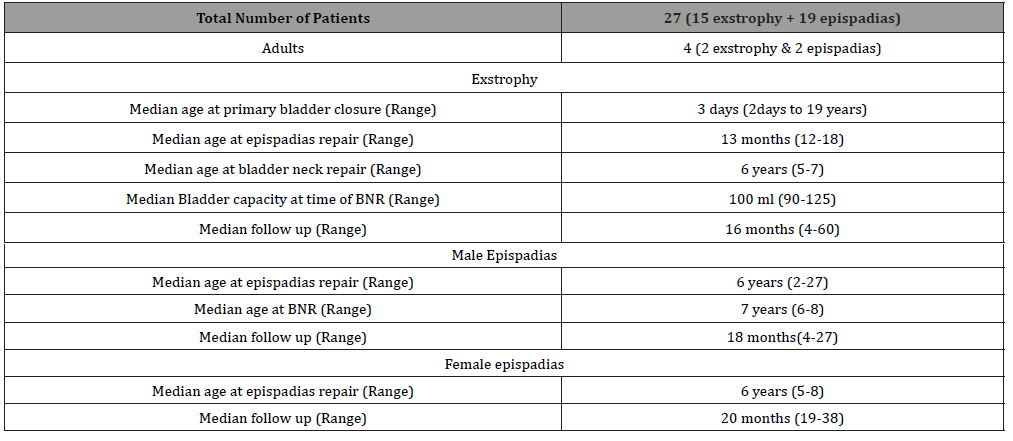
Table 4:Continence results at last follow up.
A total of 15 exstrophy and 19 epispadias surgeries were performed (Table 1). Two of the exstrophy patients were adults (one 19 years female CBE reared as male and another 31 years male exstrophy variant with true diphallia). Two of the epispadias patients also were adults (A 23 years penile and 27 years Penopubic male epispadias). Details of the procedures with associated complications is provided in Table 2. Ages at different procedures and follow ups are given in Table 3. Bladder reclosure rate was 14.2%. Male epispadias repair was performed in 14 patients (7 closed exstrophy and 7 epispadias). Fistula rate after male epispadias repair was 15.3%.
Adverse events
Additional procedures were required in four cases after 1st stage closure in CBE group. Two redo bladder closures for bladder prolapse in male exstrophy group and meatal dilatation in one female, who was continent following first stage closure with bladder outlet obstruction and bilateral hydroureteronephrosis. One child required Suprapubic Cystolithotomy (SPCL) for two cm vesical calculus. None developed vesicocutaneous fistula. We did not encounter any complication related to major soft tissue loss. All patients on follow up had stable renal function. In male epispadias group, two urethrocutaneous fistulae healed after closure. Cosmetic outcome of phallus and voiding function after epispadias repair was satisfactory. Sexual and ejaculatory functions in two adult epispadias cases were satisfactory. Rest of the patients have not attained sufficient maturity for evaluation of these functions. We evaluated continence by criteria suggested by Baird et al. Continence outcomes at last follow up are depicted in Table 4. Bladder neck repair was performed in six patients (4 exstrophy and 2 male epispadias patients). Two males and one female exstrophy cases were continent immediately after BNR. Rest of the cases are having better continence with passage of time except one who failed to improve. Three female epispadias cases were socially continent after epispadias repair only. Three male glanular/penile epispadias, 2 female vesicular epispadias were already continent. Remaining patients are awaiting bladder growth for a continence procedure to be undertaken. None of the cases had VUR after ureteric reimplantation.
Two cases in our study deserve special mention
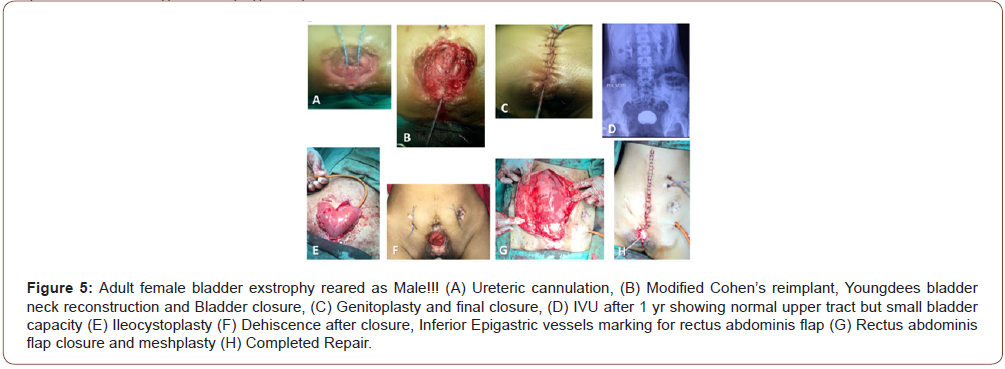
Adult female exstrophy reared as male!!!
There are very few reports of adult exstrophy mostly from third world [14-16] Incidence of female exstrophy is one in two lacs live births. Such a case reared as male up to 19 years of age has not been reported earlier to the best of our knowledge. A person was admitted in male ward with urinary incontinence since birth. Examination revealed female CBE with good bladder plate. She had female internal genitalia and karyotype 46XX. Parents were counselled and they agreed to rear her as female. Multiple bladder biopsies were done to rule out malignancy. Single stage closure of CBE with modified Cohen’s ureteric reimplant, Youngdees bladder neck reconstruction and genitoplasty were done. Intravenous urogram after one year had normal upper tracts, well-formed bladder neck with 100 cc bladder capacity. Ileocystoplasty was done. Dehiscence of neobladder required rectus abdominis flap and meshplasty (Figure 5). Multiple psychology sessions and support of elder sister helped her to attain female attire, gesture and mannerism. On her insistence she got married and is sexually cohabitating well. Finally she is continent and dry with >300 ml capacity of bladder, normal upper tract and on clean intermittent catheterisation (CIC) every 3-4 hours. She applied for change of sex in ration card, aadhar card and passport. She is being followed up with yearly cystoscopies.
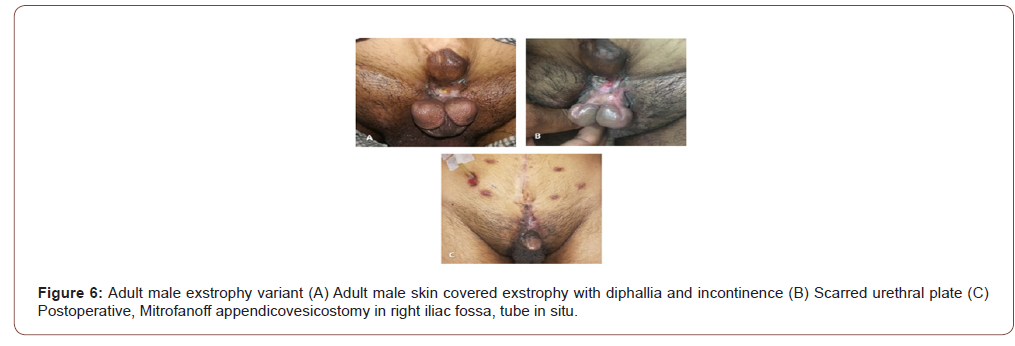
Adult male exstrophy variant with true diphallia!!!
A 31 years male presented with incontinence since birth. Examination revealed skin covered exstrophy, penopubic epispadiac meatus, partial diphallia in sagittal plane, dorsal chordee and no defined urethral plate. Diphallia itself is a rare condition incidence being 1 in 5 million births and is associated with multisystem
anomalies [17,18]. He had normal testes with well-developed secondary sexual characters. Owing to absent urethral plate, urethral reconstruction in one stage was not possible. On table cystoscopy demonstrated 400 cc bladder capacity, normal ureteric orifices and external meatus opening at bladder neck. He accepted the option of excision of one phallus with closure of bladder neck, Mitrofanoff diversion, and lifelong need for CIC. He was happy with perfect continence, cosmetically acceptable phallus and erections despite the need of regular CIC (Figure 6).
Discussion
The goals of treatment of CBE and epispadias are preservation of renal function, continence, cosmetically acceptable genitalia and ability to sexually cohabitate and reproduce. It requires multidisciplinary approach including pediatric urologist, neonatologist, plastic surgeon, pediatric surgeon, and psychologist. In a large series of 210 CBE patients, 187 underwent bladder reconstruction. Bladder dehiscence rate was 10.5%. This cohort included first stage repair without osteotomy as well as referred cases of failed closure despite osteotomy in some cases. [19] In our series, reclosure rate was 14.2%. Most of our neonates were operated around 72 hours, therefore, Pelvic osteotomy was not warranted. Good symphysial approximation and Bryant traction helped to attain sound closure. The Bryant traction additionally prevents fecal contamination of stitch line. In adult cases, the limited available literature doesn’t advocate osteotomy [14]. We did not face any complication of major soft tissue loss of glans, corpora and urethral plate. Such complications are described with more CPRE [20]. Kelly described a radical soft-tissue mobilization procedure in various stages achieving tension free closure without the need of osteotomies. At birth, bladder closure in first stage was followed by proximal urethral reconstruction and creation of penoscrotal meatus at 3-6 months. In this stage, pelvic floor muscles were radically mobilised to wrap around proximal urethra to impart continence. Penoscrotal hypospadias was repaired at the age of three years contrasting from disassembly techniques [21]. Mitchell combined bladder closure with epispadias repair in one stage. Now it is a part of the complete primary repair of exstrophy (CPRE) for primary closure in the new born. He repaired epispadias by penile disassembly where penis was dissected into three corporal bodies completely. Bladder neck tailoring was done to increase outlet resistance in the same stage. Ureteric reimplantation was done in second stage. However, this technique was not reproducible and Borer et al., 2017 and Kasprenski et al., 2018 reported major soft tissue losses .This surgical techique also resulted into hypospadiac meatus in more than fifty percent cases. There are more endorsers of similar but partial disassembly in modified Cantwell-Ransley repair on the strength of ease without hypospadias [22,23]. Rectus abdominis flap is a very handy, locally available and gives a robust abdominal wall closure. This virtually obviates the need of pelvic osteotomy and pubis closure in adults and redo cases as well [16]. This flap combined with peritoneum can be used for bladder augmentation as well. Some workers have advocated routine use of this flap in single stage CPRE [24].
The incidence of bladder calculi in closed exstrophy is reported to be 15%. The possible causes are use of nonabsorbable sutures (for bladder closure or approximation of symphysis) and stasis with infection following BNR or bladder augmentation [25]. Rate of urethrocutaneous fistula after modified Cantwell Ransley epispadias repair ranges from 13% to 33% with rates being higher in secondary repair as compared to primary repair [9]. In all our primary cases fistula rate was 15.3%. Continence results are difficult to compare as there is no single standard criteria to define it and it continues to improve after surgery. Schaeffer and colleagues used very simple criteria and divided outcomes in three groups, the three groups being continent, continent during the day and have nocturnal incontinence, and continuously incontinent. [20]. Baird et al in a series of 67 males with CBE, reported continence in 70% of cases, social continence in 10.6% cases. Failed BNR was faced in 19.4% [13].Mean age at BNR was 5.8 years. Final achievement of the continence depends on two most important factors, primary bladder closure at birth and bladder capacity at time of BNR. A successful primary bladder closure is an important factor for getting a larger bladder, getting it more quickly and for achieving a high continence rate [5]. Multiple reclosures markedly diminishes the chances of eventual continence [6]. Apart from providing a better chance of achieving continence successful primary closure also decreases overall cost [26]. Continence rate in our series after bladder neck repair was 83.4%. Gearhart and coworkers presented their results of 11 complete female epispadias repairs. They either performed a staged repair, urethroplasty and genitoplasty being done in 1st stage and BNR in 2nd stage or a combined urethral, genital or bladder neck repairs in one stage. Eight patients underwent BNR and mean interval to maximum continence was 18 months. Overall continence rates were 87% [11]. In our study two female epispadias patients were not incontinent. And three were partly continent at last follow up and will be considered for bladder neck procedure if needed. Pediatric Urology Midwest Alliance shared a 36 years long, multi institutional retrospective cohort experience and proposed a probability of bladder augmentation, diversion and need of CIC in bladder exstrophy patients. In their cohort of 216 patients with median 14.4 years follow up, the probability of bladder augmentation/diversion was 14.9% by age 5 years, 50.7% by 10 years and 70.1% by 18 years. Among the entire group, 67.4% performed clean intermittent catheterization at last follow up, obviously more in augmentation/diversion group and less in native bladder group [27]. In our series two patients required augmentation/diversion both of which presented in adulthood.
Satisfactory cosmesis is always a concern in males as they have short penis, dorsal chordee and require multiple genital surgeries. Ansari and colleagues in a review of EEC patients on issue of sexuality, sexual function and fertility concluded that heterosexuality is expressed in both sexes and most of them have adequate sexual function. Regarding fertility, most female patients had normal fertility but males had significantly low fertility [28]. Pubic diastasis facilitates vaginal delivery. Taskinen et al studied gender identity and sex role in exstrophy epispadias population and compared it with normal control. Gender Identity/ gender dysphoria questionnaire for adolescents and adults (GIDYQAA) and Bem sex role inventory (BSRI) were obtained from 33 exstrophy epispadias patients and 99 gender matched control. They found that male patients had lower gender identity score than controls. Female patients had better female sex role index [29]. Further follow up into adolescence and adulthood would unfold several other issues related to gender identity, sex role and sexual function in our series. The limitation of our study is small number of patients and intermediate term follow up. But strength of this study is variety of cases of wide spectrum of EEC including both sexes. Only those with good volume of cases, reconstructive skills and adequate experience should attempt repair of such cases. Any futile attempt may lead to irreparable loss of tissues such as glans, corpora or urethral plate.
Conclusion
EEC is a condition that needs continued care right from birth till attainment of sexuality and reproduction. Patient and parental counselling are of paramount importance in this regard. Achievement of perfect continence with preservation of upper tracts is the ultimate goal. Presentation in adulthood is extremely rare. These cases need bladder augmentation, use of robust flap interposition to achieve good bladder capacity and sound abdominal wall closure in one stage. In spite of, acceptable continence after BNR, many will need CIC. Presentation of female CBE at 19 years (reared as male) is unique and was not cited in the available literature.
Fundamentals
The surgeon should be well versed with multiple repair techniques to prevent irreparable tissue loss. EEC needs continued care right from birth till attainment of sexuality and reproduction. Preservation of upper tracts with achievement of continence is the ultimate goal. Need for CIC / Diversion in future should always be explained. Adult exstrophy repair should be done in a single stage with bladder augmentation and use of flap for abdominal wall closure. Bladder preservation is possible in adult exstrophy also.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Lattimer JK, Vernon Smith MJ (1966) Exstrophy Closure: a Follow up on 70 Cases. J Urol. 95: 356–359.
- Gambhir L, Höller T, Müller M, Schott G, Vogt H, et al. (2008) Epidemiological Survey of 214 Families with Bladder Exstrophy-Epispadias Complex. J Urol 179(4): 1539–1543.
- Nelson CP, Dunn RL, Wei JT (2005) Contemporary Epidemiology of Bladder Exstrophy in the United States. J Urol 173(5): 1728–1731.
- Wood HM, Babineau D, Gearhart JP (2007) In vitro fertilization and the cloacal/bladder exstrophy–epispadias complex: A continuing association. J Pediatr Urol 3: 305–310.
- Oesterling JE, Jeffs RD (1987) The Importance of a Successful Initial Bladder Closure in the Surgical Management of Classical Bladder Exstrophy: Analysis of 144 Patients Treated at the Johns Hopkins Hospital Between 1975 and 1985. J Urol 137(2): 258–262.
- Gearhart JE, Ben-Chaim J, Sciortino C, Sponseller aul D, Jeffs RD (1996) The multiple reoperative bladder exstrophy closure: What affects the potential of the bladder? Urology 47: 240–243.
- Cantwell FV (1895) I. Operative Treatment of Epispadias by Transplantation of the Urethra. Ann Surg. 22(6):689–694.
- Ransley PG, Duffy PG, Wollin M (1989) Bladder exstrophy closure and epispadias repair. In: Operative Surgery- Pediatric Surgery. London: Butterworths p.620.
- Baird AD, Gearhart JP, Mathews RI (2005) Applications of the modified Cantwell–Ransley epispadias repair in the exstrophy–epispadias complex. J Pediatr Urol 1(5): 331–336.
- Gearhart JP, Mathews R (2000) Penile reconstruction combined with bladder closure in the management of classic bladder exstrophy: illustration of technique. Urology 55(5): 764–770.
- Gearhart JP, Peppas DS, Jeffs RD (1993) Complete Genitourinary Reconstruction in Female Epispadias. J Urol 149(5): 1110–1113.
- Davis DM (1928) Epispadias in females and its surgical treatment. Surg Gynec & Obst 47: 680.
- Baird AD, Nelson CP, Gearhart JP (2007) Modern staged repair of bladder exstrophy: A contemporary series. J Pediatr Urol 3(4): 311–315.
- Mansour AM, Sarhan OM, Helmy TE, Awad B, Dawaba MS, et al. (2010) Management of bladder exstrophy epispadias complex in adults: is abdominal closure possible without osteotomy? World J Urol 28(2): 199–204.
- Hosseini SMV, Zarenezhad M, Sabet B (2011) Abdominal wall closure in bladder exstrophy complex repair by rectus flap. Ann Afr Med 10(3): 243-245.
- Agarwal P (2011) Closure and augmentation of bladder exstrophy using rectus abdominis musculo-peritoneal flap. Indian J Plast Surg 44(3): 444-447.
- Gyftopoulos K, Wolffenbuttel KP, Nijman RJM (2002) Clinical and embryologic aspects of penile duplication and associated anomalies. Urology 60(4): 675–679.
- Frolov A, Tan Y, Rana MWUZ, Martin JR (2018) A Rare Case of Human Diphallia Associated with Hypospadias. Case Rep Urol 13: 1–6.
- Bhatnagar V (2011) Bladder exstrophy: An overview of the surgical management. J Indian Assoc Pediatr Surg 16(3): 81-87.
- Schaeffer AJ, Stec AA, Purves JT, Cervellione RM, Nelson CP, et al. (2011) Complete Primary Repair of Bladder Exstrophy: A Single Institution Referral Experience. J Urol 186(3): 1041–1047.
- Kelly JH (1995) Vesical exstrophy: repair using radical mobilisation of soft tissues. Pediatr Surg Int 10: 298–304.
- Borer JG, Vasquez E, Canning DA, Kryger JV, Bellows A, et al. (2017) Short-term outcomes of the multi-institutional bladder exstrophy consortium: Successes and complications in the first two years of collaboration. J Pediatr Urol 13(3): 275.e1-275.e6.
- Kasprenski M, Maruf M, Davis R, Jayman J, Benz K, et al. (2020) Penile Disassembly in Complete Primary Repair of Bladder Exstrophy: Time for Re-evaluation? Urology 137: 146–151.
- Giron AM, Mello MF, Carvalho PA, Moscardi PRM, Lopes RI, et al. (2017) One - staged reconstruction of bladder exstrophy in male patients: long - term follow-up outcomes. Int Braz J Urol 43(1): 155–162.
- Silver RI, Gros DA, Jeffs RD, Gearhart JP (1997) Urolithiasis in the Exstrophy-Epispadias Complex. Urol. 158(3 pt 2): 1322-1326.
- Nelson CP, North AC, Ward MK, Gearhart JP (2008) Economic Impact of Failed or Delayed Primary Repair of Bladder Exstrophy: Differences in Cost of Hospitalization. J Urol 179(2): 680–683.
- Szymanski KM, Fuchs M, Mcleod D, Rosoklija I, Strine AC, et al. (2019) Probability of Bladder Augmentation, Diversion and Clean Intermittent Catheterization in Classic Bladder Exstrophy: A 36-Year, Multi-Institutional, Retrospective Cohort Study. J Urol 202(6): 1256–1262.
- Ansari M, Cervellione R, Cervellione J (2010) Sexual function and fertility issues in cases of exstrophy epispadias complex. Indian J Urol 26(4): 595-597.
- Taskinen S, Suominen JS, Mattila AK (2016) Gender Identity and Sex Role of Patients Operated on for Bladder Exstrophy-Epispadias. J Urol 196(2): 531–535.
-
Mukesh Chandra Arya, Vivek Vasudeo, Yogendra Shyoran, Abhiyutthan Singh Jadaon, Manoj Kumar Garg, Ankur Singhal, Ajay Gandhi. Exstrophy Epispadias Complex: Outcome Analysis of Repair Performed at A Single Centre. Annal Urol & Nephrol. 2(4): 2021. AUN.MS.ID.000545.
-
Exstrophy-epispadias complex, Genitourinary system, Retrospective analysis, Bladder exstrophy, Epispadias, Genitoplasty, Mitrofanoff diversion
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






