 Research Article
Research Article
Acute Kidney Injury in Adult Patients: Experience of a Single Center During a 5-Year Period
Rebic D*, Hamzic Mehmedbasic A, Dautbegovic E, Hasanspahic S, Herenda V, RibicMrkonja A, Odobasic M
Nephrology Clinic, Clinical Center University of Sarajevo, Bosnia and Herzegovina
Damir Rebic, Nephrology Clinic, Clinical Center University of Sarajevo, Bosnia and Herzegovina.
Received Date: December 29, 2022; Published Date: January 12, 2023
Abstract
Introduction: Acute kidney injury (AKI) is an under-recognized disorder, which is associated with a high risk for mortality, and the development of chronic kidney disease (CKD).The aim of this study was to determine the etiology and severity of AKI among hospitalized patients at our clinic in the five-year follow-up period according to the contemporary classifications (RIFLE, AKIN, and KDIGO).
Methods: We analyzed a clinical database of 312 adult patients who were consecutively admitted to hospitals in Clinic for nephrology in the previous 5 years. AKI was defined by the RIFLE, AKIN, and KDIGO criteria. Receiver operating curves were used to compare the predictive ability for mortality, and regression analysis was used for the calculation of odds ratios and 95% confidence intervals.
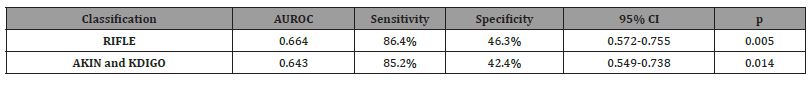
Results: The incidence rates of AKI based on the RIFLE, AKIN, and KDIGO criteria were 13,1%, and 12,4%, respectively. However, the predictive ability of all three classifications for renal function recovery was poor (AUROC: RIFLE 0.664, AKIN and KDIGO 0.643). According to the RIFLE and AKIN criteria, in-hospital was statistically significantly higher in stage F/3, compared to stages R/1 and I/2. Only the RIFLE classification showed a statistically significant difference in in-hospital mortality incidence rate between the stages: in-hospital mortality was more frequent in stage F than in stages R and I. According to the RIFLE criteria, patients in stage F of AKI had a relative risk of 4.95, which means they had a 5 times higher possibility of in-hospital mortality than patients categorized as stage I and II of AKI.
Conclusions: The incidence of AKI in ill patients varied according to the criteria used. The RIFLE criteria identified more patients as AKI than KDIGO and AKIN did. Compared with the KDIGO criteria, RIFLE was more predictive for in-hospital mortality, but there was no significant difference between AKIN and KDIGO.
Keywords: Acute kidney injury; Causes; Outcome; Adults
Abbreviations: AKI: Acute kidney injuri; CKD: Chronic kidney disease; ESRD: End-stage renal disease; ICU: Intensive care unit, KDIGO: The Kidney Disease Improving Global Outcome; RIFLE: Risk Injury Failure Loss of Kidney Function, AKIN: Acute Kidney Injury Network; eGFR: The estimated glomerular filtration rate; MDRD: Modification of Diet in Renal Disease Study
Introduction
Acute kidney injury (AKI) is a complex syndrome with wide variation in etiologies that makes its outcome difficult to predict. It is associated with various etiologies and pathophysiological mechanisms and manifested by increased serum creatinine (Scr) or re duction in urine output [1]. Acute kidney injury is a common complication in patients admitted to hospital (10-15%), with increasing incidence in recent years, especially in the intensive care unit (ICU), where it can sometimes exceed 50% [2]. It is associated with ad verse short- and long-term outcomes and increased mortality, placing a high cost to patients, as well as healthcare systems[1]. Due to its prognostic impact and frequent development as part of other syndromes such as heart failure, liver failure, and sepsis, early and rapid diagnosis of AKI is crucial in all adult and pediatric patients.
There are significant variations in the reported incidence of AKI, which can be explained by population differences, differences between high-income and low-to-middle-income countries, and most importantly by the inconsistent use of diagnostic criteria for AKI. Additionally, there is a lack of studies comparing critically ill and non-critical patients, which makes it difficult to reach accurate conclusions on the epidemiology of AKI [3]. Considering the prognostic impact and outcomes of AKI, substantial research has focused on assessment and comparison of diagnostic criteria, as well as prevention and treatment strategies, which necessitate uniform epidemiological data. Over the last few decades, the definition and classifications of AKI have been modified and improved significantly, starting with the Risk, Injury, Failure, Loss of Kidney Function, End-Stage Kidney Disease (RIFLE) classification in 2004, Acute Kidney Injury Network (AKIN) classification in 2007, until the recently developed Kidney Disease Improving Global Outcomes (KDIGO) classification, which had the aim of unifying the definition of AKI. Since then, many studied have compared the three classifications in their reported incidence of AKI, as well as sensitivity, accuracy, and predictive ability for various short- and long-term outcomes [4,5,6].
AKI is not a single disease but, rather, a loose collection of conditions that share common diagnostic features. The causes of AKI have traditionally been divided into three broad categories, according to the semi-anatomical divisions of the urinary tract: prerenal azotemia, intrinsic renal parenchymal disease, and postrenal obstruction. Identification of prognostic factors of AKI provides the information necessary to make important medical decisions. The presence of AKI is usually determined by an elevation in the serum creatinine concentration, however, it might be challenging to diagnose AKI if a patient’s baseline renal function is not well documented, so it must be inferred using medical history.
The aim of this study was to determine the etiology and severity of AKI among hospitalized patients at our clinic in the five-year follow-up period according to the contemporary classifications (RIFLE, AKIN, and KDIGO) and compare the incidence of stages of AKI using different classification systems
Material and Methods
This study was retrospective analysis of prospectively collected data. It was performed during period 2016-2020 at Clinic for Nephrology in University Clinical Centre of Sarajevo. Three hundred and twelve patients with presence of AKI according to the RIFLE (Risk, Injury, Failure, Loss, and End-stage kidney disease) who gave their informed consent were enrolled in the study. Patients included in this study were adults (age ≥18 years) with hospital stay ≥24 hours. Patients with preexisting end-stage renal disease on chronic dialysis or with prior kidney transplant were excluded. AKI was defined and categorized according to RIFLE classification, based on creatinine criteria [4]. Class Risk was considered if there was an increase of baseline serum creatinine x1.5; Class Injury was considered if there was an increase of baseline serum creatinine ×2; and Class Failure was considered if there was an increase of baseline serum creatinine ×3, or if there was an acute rise in serum creatinine of at least 44 μmol/L in patients with baseline serum creatinine >354 μmol/L. When pre-admission serum creatinine was unavailable, it was estimated by the Modification of Diet in Renal Disease (MDRD) equation, as recommended by the Acute Dialysis Quality Initiative (ADQI) Working Group [5].
Septic origin of AKI was diagnosed in those patients who had recognized source of infection, regardless of whether the blood culture was positive or not, and if they had verified increased blood urea nitrogen and serum creatinine. Criteria for the diagnosis of sepsis and septic shock were defined according to consensus American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (ACCP/SCCM) [5] Patients were followed-up until hospital discharge or death. Outcome of AKI was defined according to the values of creatinine clearance as recovered (creatinine clearance >60 mL/min) and unrecovered (creatinine clearance <60 mL/min) with impaired renal function.
Statistical Analysis
Statistical analysis was realized using SPSS software (version 21.0). Chi-square, fisher mood’s median test were used to compare variables. Regression statistical model was used to test for significance of association between the independent and dependent variables. Values were considered significant at p < 0.05.
Results
A total of 312 patients participated in the study, of which 154 were men and 158 were women. The median age of patients was 72 (62-80), while the median age of men was 69 (60.75-79.25) years, and the median age of women was 73 (65-80) (Figure 1). (Table 1) shows the distribution of patients according to classification stages. According to the RIFLE classification, a slightly smaller number of subjects were classified in the first (R) and second (I) stages of acute kidney injury. The distribution of subjects according to AKIN and KDIGO classification was almost identical. The study showed that a total of 42.04% of patients had prerenal, 49.04% had renal, while 8.92% had postrenal acute kidney injury (Figure 2). (Table 2) shows the frequency and percentage of patients according to the causes of AKI. Of the total number of patients, 28% had hypovolemia with kidney hypoperfusion as the cause of AKI, while AKI was caused by an infectious syndrome in 19.8% of cases. (Table 3) shows that 88.4% of patients had a satisfactory treatment outcome, 32.6% were cured while 55.8% recovered. Of the total number of patients, 2.9% had a verified worsening of renal function during hospitalization, while mortality was recorded in 8.7% of patients.
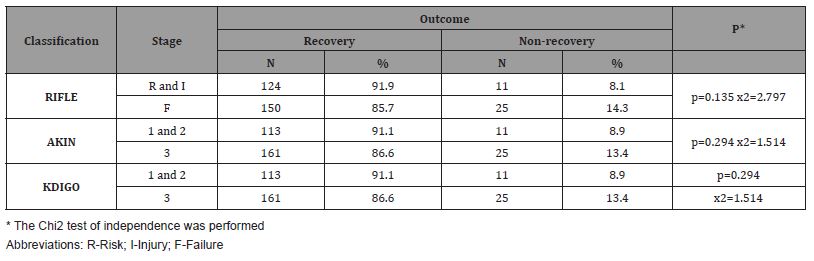
Comparison of renal function recovery based on the stages of RIFLE, AKIN and KDIGO criteria is shown in Table 4. Based on all three classifications, patients in stage 1/R and stage 2/I of AKI had a significantly higher percentage of renal function recovery than patients in stage 3/F of AKI.
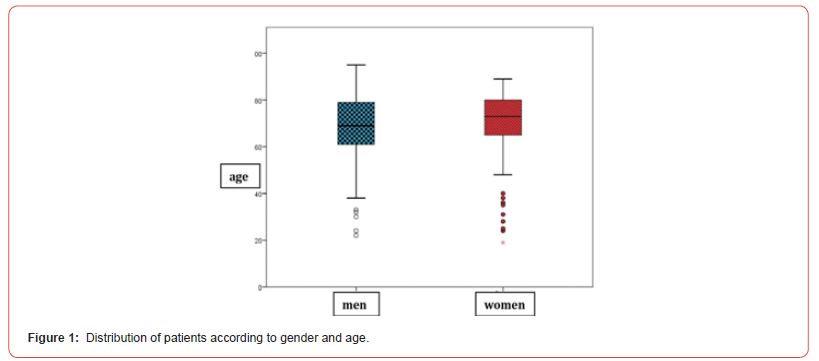
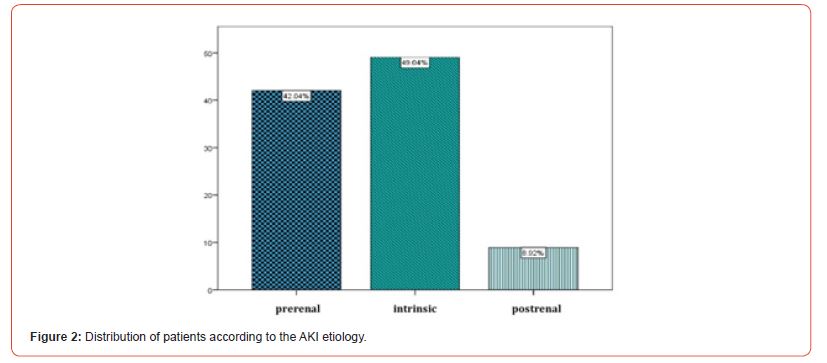
Table 1:Distribution of patients according to the AKI stages.
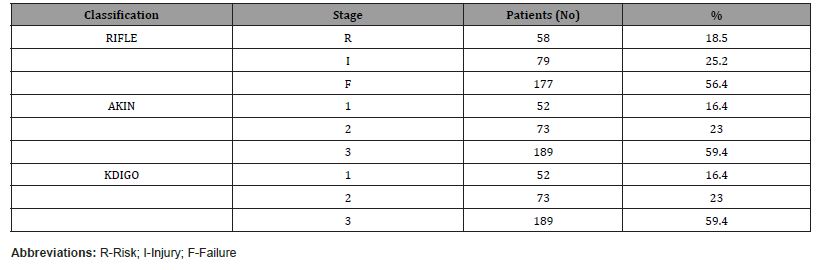
Table 2:Causes of AKI.
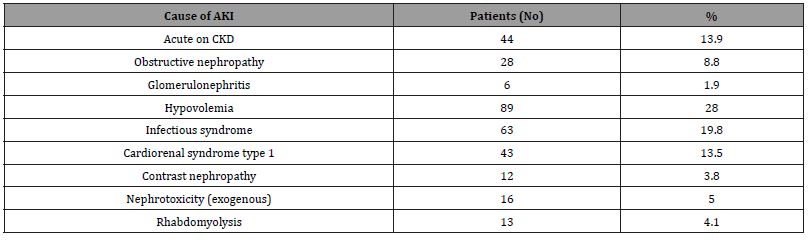
Table 3:Outcome of AKI.
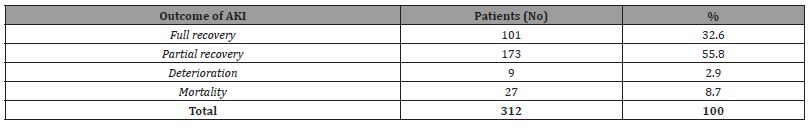
Table 4:Comparison of the outcome of patient according to the stages of AKI based on KDIGO, RIFLE and AKIN classification.
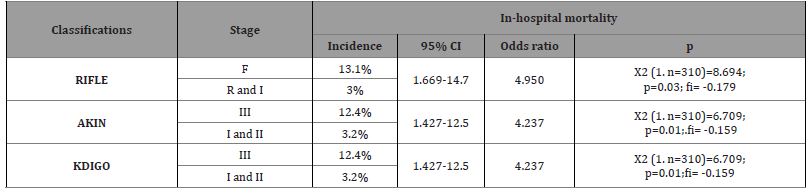
Comparison of incidence rate of in-hospital mortality in stage 3 of each classification with stages 1 and 2 is shown in (Table 5). Only the RIFLE classification showed a statistically significant difference in in-hospital mortality incidence rate between the stages: in-hospital mortality was more frequent in stage F than in stages R and I. According to the RIFLE criteria, patients in stage F of AKI had relative risk of 4.95, which means they had 5 times higher possibility of in-hospital mortality than patients categorized as stage I and II of AKI. AKIN and KDIGO classifications were statistically significantly associated with increased relative risk of in-hospital mortality.
Table 5:In-hospital mortality incidence rate and relative risk.
Area under the ROC curves for RIFLE, AKIN, and KDIGO classifications and their predictive abilities for renal function outcome are shown in (Figure 3) and (Table 6). Using the three AKI classifications (RIFLE, AKIN and KDIGO) as a predictive test for renal function recovery showed that: RIFLE classification had AUROC=0.664, p=0.005- suggesting it has failed as a predictive test. KDIGO and AKIN classification had identical results AUROC=0.643, p=0.014 - suggesting that they can be used as one of the predictive tests, but with “poor” accuracy. They have a relatively high sensitivity (85.2%) with a specificity of 42.4%.
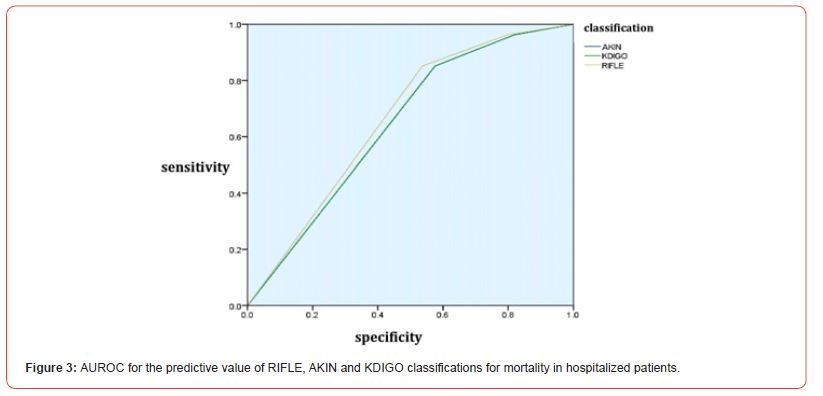
Table 6:ROC analysis of RIFLE, AKIN and KDIGO classifications for mortality in hospitalized AKI patients.
Discussion
Numerous studies have compared the RIFLE and AKIN criteria for AKI [7,8]. However, the incidence of AKI still varied. Based on these two criteria, the KDIGO criteria were proposed in order to unify the definition of AKI. To date, only a few previous studies have compared the incidence and mortality of AKI in critically ill patients according to these three definitions in a period of several years. Identification of prognostic factors of acute kidney injury is very important for proper clinical treatment, quality control and management of health resources. Earlier epidemiological studies have demonstrated a great diversity in the etiology and prognostic factors of acute kidney injury, and pointed to a common consequent development of chronic kidney disease [2,7].
Our data showed that AKI remains a common clinical condition in adults in urban or semi-urban areas. Patient presented with the severe form of AKI but more in the semi-urban area. Pre renal AKI was more prevalent and the main aetiologies were sepsis and volume depletion Of the 312 patients files assessed in both hospitals, 55.58% were female, resulting in an F: M ratio of 1.25:1. The median age (IQR) was 59 (19-93) years, this distribution is quite similar to previous studies in other developing countries showing a female gender preponderance with those in mid-age being more affected [9-11]. The disparities in age between developing and developed countries lies in the difference in life span of the general population (generally more longer in developed countries) and in the differences of risk factors of AKI (infectious causes versus non communicable diseases).
Although many studies have reported an increased incidence of AKI, there is notable variability in the reported incidence, which could be contributed to different causes of AKI and diagnostic criteria used, as well as differences in the characteristics of the populations studied [4]. In the present study, the incidence of AKI defined by the RIFLE, AKIN and KDIGO classifications varied between 3.2 and 13.1% depending on the classification used. The incidence of AKI defined by the RIFLE classification (F) was slightly higher (13.1%) than that defined by KDIGO and AKIN classifications, but there were no significant variations between the three classifications.
Furthermore, a clinical trial conducted by colleagues reported identical incidence of AKI according to the AKIN and KDIGO classification (25.9%) [12]. An increased incidence of AKI according to the KDIGO criteria compared to the AKIN criteria could be explained by the fact that for AKI diagnosed (with an increase in creatinine 1.5 x relative to the baseline values) according to KDIGO criteria, a longer timeframe of 7 days is allowed, compared to the timeframe of only 48 hours used to diagnose AKI according to AKIN criteria. Furthermore, diagnosing AKI based on the RIFLE criteria can be difficult due to the occasional lack of baseline creatinine values, which then requires the use of MDRD formulas to calculate the value. Variability in the reported incidence of AKI is further attributable to different clinical settings. There are important differences in the reported incidence among ambulatory patients, patients hospitalized in different clinical departments and critically ill patients [13]. In the present study, AKI was diagnosed based on the RIFLE classification the highest percentage was represented in the Failure stage. Using the AKIN and KDIGO classification (stage III), AKI was diagnosed in the same number of patients and was often represented on stage. Accordingly, the highest number of patients was categorized as stage 3 of each classification. When comparing the severity of AKI, there was no statistically significant difference between stages of AKI based on the three classifications (RIFLE, AKIN and KDIGO). These results are supported by the results of other studies, such as the one conducted by Bastin and colleagues, which concluded that the staging of AKI based on the KDIGO criteria was identical to the AKIN criteria[12]. In the present study, prerenal type of AKI was diagnosed in 42.04% of patients, intrinsic type in 49.04%, and postrenal type in 8.92% of patients. The most frequent causes of AKI were hypovolemia and infectious syndrome. These results are supported by the results of a study conducted by Thongprayoon and al., where prerenal and intrinsic type of AKI were most frequently diagnosed [14]. Poston and al. also reported prerenal cause as the most frequent contributor to AKI in 49.1% of patients [15]. Furthermore, Wilson and al. found that the most frequent cause of AKI was prerenal , followed by sepsis-associated AKI and ischemic acute tubular necrosis [16].
Among 312 patients with AKI in the present study, 88.4% had a full and partially recovered renal function, while 2.9% had deterioration renal function. Using the three AKI classifications (RIFLE, AKIN and KDIGO) as a predictive test for renal function recovery showed the following: RIFLE classification had AUC=0,664 (0,005) - suggesting it has failed as a predictive test. KDIGO classification had AUC=0.643 (0,014) - suggesting that it could be used as one of the predictive tests but with “poor” accuracy. AKIN had same results AUC.
According to all three classifications (RIFLE, AKIN and KDIGO), in-hospital mortality increased in accordance with staging of AKI. Comparing stage 3 with stages 1 and 2 jointly, both AKIN and RIFLE classification showed statistically significant difference between the stages: in-hospital mortality was more frequent in 3/F than in 1/R and 2/I. Based on all three classifications, there was a weak, but significant correlation with in-hospital mortality; stage of AKI had a significant influence on in-hospital mortality (RIFLE incidence 13.1%, AKIN and KDIGO 12.4%). These results, although not as compelling as the results of other studies, do show that higher degrees of AKI severity are associated with increased risk of in-hospital mortality. One such study was published, where the in-hospital mortality rate was 2.2% and varied significantly depending on the severity of AKI [17]. Our results confirm that all three classifications have similar but poor predictive ability for in-hospital mortality. These results are similar to the results of a study about improve outcomes in acute kidney injury, where they investigated septic patients and found that all three classifications have similar prognostic abilities and there were no statistically significant differences between them [4,5,12, 18-21].
However, the results of the present study differ from the results of many previous studies that have found better predictive ability of some criteria for in-hospital mortality, compared to others. For example, a study by Pan and al. showed that the KDIGO criteria had greater predictive ability compared with the RIFLE criteria, according to the AUC curve for in-hospital mortality (AUROC: RIFLE 0.738, AKIN 0.746, KDIGO 0.757). There was no significant difference between AKIN and KDIGO in their predictive ability for in-hospital mortality (0.757 versus 0.746, p=0.12) [7]. Bastin and al. found that in patients after cardiac surgery, the AKIN classification correlated better with in-hospital mortality than the RIFLE criteria (AUROC: AKIN 0.86 RIFLE 0.78) [12]. It has been confirmed in some studies that RIFLE and KDIGO criteria had similar and sufficient prognostic ability for in-hospital mortality and performed better than the AKIN criteria (AUROC: RIFLE 0.77, AKIN 0.69, KDIGO 0.78) [22]. On the other hand, one study claimed that in patients with type 1 cardiorenal syndrome, the KDIGO criteria are superior in their outcome prediction, compared to RIFLE and AKIN (AUROC: RIFLE 2.56, AKIN 2.68, KDIGO 4.00) [23]. Also, a study that was done before the COVID-19 pandemic investigated patients on extracorporeal membrane oxygenation (ECMO) support and showed that all three classifications had excellent predictive ability, although the KDIGO classification performed better than RIFLE and AKIN (AUROC: RIFLE 0.826, AKIN 0.836, KDIGO 0.840) [24]. These discrepancies in the results of the present study and most others could be explained by a small sample size in the present study, and rather low in-hospital mortality rate.
The main limitation of the present study is that it was a single- center study, with a relatively small cohort of patients. As a retrospective study, quality of data was dependent on the accuracy of health provider to keep his archives. Over 20% of files were not reviewed because of either missing or incomplete clinical information. The definition of renal recovery limited to short term (at discharged), the absence of baseline serum creatinine availability may have. Bias in the analysis of the outcome related to these parameters. Furthermore, pre-admission serum creatinine level was unknown in some cases, necessitating the application of the MDRD equation to calculate an estimated baseline value.
Although these classifications are exceedingly important in the diagnosis of AKI, the fact that they rely on markers which are insensitive and unspecific for AKI demands caution. It is becoming increasingly apparent that novel biomarkers must be researched, and diagnostic measures, as well as treatments could still be improved [25]. This study could be expanded to better understand the role of the three classifications (RIFLE, AKIN, and KDIGO) for AKI. For example, patients could be monitored for a longer period after discharge from the hospital, to determine whether CKD has developed, and whether the classifications have any predictive ability for the development of certain stages of CKD. This would require monitoring the patients’ renal function 3 months after discharge of the patient, at the earliest. Furthermore, we believe that future studies should include ICU patients in several clinical centers, to diagnose AKI on time and take appropriate measures to prevent it in the future.
Conclusion
There were no significant variations in incidence of AKI in patients hospitalized at the Nephrology Department according to the RIFLE, AKIN, and KDIGO criteria. When comparing the severity of AKI, there was no statistically significant difference between stages of AKI based on the three classifications. Based on the RIFLE and AKIN criteria, the number of in-hospital mortalities was significantly higher in stage F/3, compared to stages R/1 and I/2. However, ROC analysis showed that all three classifications showed similar, but poor predictive ability for renal function outcome and in-hospital mortality. Compared with the KDIGO criteria, RIFLE was more predictive for in-hospital mortality, but there was no significant difference between AKIN and KDIGO. The integration of the new biomarkers of AKI into the clinical classification could increase the sensitivity and specificity of AKI diagnosis, overwhelming some of the limitations of the traditional markers of kidney function, such as creatinine and urine output. The high prevalence of AKI, even in the post-COVID era, indicates that there is a need to raise awareness about AKI as well as better preventive protection of patients in primary health care and overall care.
Acknowledgements
None.
Conflict of interest
The authors report no conflicts of interest in this work.
References
- Georges TD, Marie Patrice H, Ingrid TS, Mbua RG, Hermine FM, et al. (2022) Causes and outcome of acute kidney injury amongst adults patients in two hospitals of different category in Cameroon; a 5 year retrospective comparative study. BMC Nephrol 14; 23(1): 364.
- Luo X, Jiang L, Du B, Wen Y, Wang M, et al. Beijing Acute Kidney Injury Trial (BAKIT) workgroup (2014) A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care 8;18(4): R144.
- Georges TD, Marie Patrice H, Ingrid TS, Mbua RG, Hermine FM, et al. (2022) Causes and outcome of acute kidney injury amongst adults patients in two hospitals of different category in Cameroon; a 5 year retrospective comparative study. BMC Nephrol 23(1): 364.
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Care 8(4): R204-212.
- Mehta RL, Kellum JA, Shah S V, Molitoris BA, Ronco C, et al. (2007) Acute kidney injury network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care 11(2); 31.
- Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, et al. (2012) Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int 1: 138.
- Pan HC, Yang SY, Chiou TT, Shiao CC, Wu CH, et al. (2022) Comparative accuracy of biomarkers for the prediction of hospital-acquired acute kidney injury: a systematic review and meta-analysis. Critical care (London, England)26(1): 349.
- Ostermann M, Bellomo R, Burdmann EA, Doi K, Endre ZH, et al. Conference Participants (2020) Controversies in acute kidney injury: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Conference. Kidney international98(2); 294-309.
- Asraf OO, Sameeha AA, Suleiman MM, Shaher MS, Basheer YK, et al. (2020) Incidence, risk factors, and outcome of acute kidney injury in the intensive care unit: a single-Centre study from Jordan. Critical Care Research and Practice 7(30): 8753764.
- Mohamed EE, Osman MI, Tasneem I (2010) Causes and outcome of acute kidney injury: GEZIRA experience. Sudan JMS 5(3).
- Gordon JP, Wendy M, Jyoti B, Izhar HK, Keith S, et al. (2007) A prospective national study of acute renal failure treated with RRT: incidence, aetiology and outcomes. Nephrol Dial Transplant 22(9): 2513-2519.
- Bastin AJ, Ostermann M, Slack AJ, Diller GP, Finney SJ, et al. (2013) Acute kidney injury after cardiac surgery according to Risk/Injury/Failure/Loss/End-stage, Acute Kidney Injury Network, and Kidney Disease: Improving Global Outcomes classifications. J Cri Care 28 (4): 389-3965.
- Gameiro J, Agapito Fonseca J, Jorge S, Lopes J (2018) Acute Kidney Injury Definition and Diagnosis: A Narrative Review J Clin Med 7(10): 307.
- Thongprayoon C, Hansrivijit P, Kovvuru K, Kanduri SR, Torres Ortiz A, et al. (2020) Diagnostics, Risk Factors, Treatment and Outcomes of Acute Kidney Injury in a New Paradigm. J Clin Med 9(4): 1104.
- Poston J T & Koyner J L (2019) Sepsis associated acute kidney injury. BMJ 9: 364, k4891.
- Wilson FP, Martin M, Yamamoto Y, Partridge C, Moreira E, Arora T, et al. (2021) Electronic health record alerts for acute kidney injury: multicenter, randomized clinical trial. BMJ 372: m4786.
- Sawhney S, Fraser SD (2017) Epidemiology of AKI: Utilizing Large Databases to Determine the Burden of AKI. Advances in chronic kidney disease, 24(4): 194-204.
- Pereira M, Rodrigues N, Godinho I, Gameiro J, Neves M, et al. (2017) Acute kidney injury in patients with severe sepsis or septic shock: a comparison between the ‘Risk, Injury, Failure, Loss of kidney function, End-stage kidney disease’ (RIFLE), Acute Kidney Injury Network (AKIN) and Kidney Disease: Improving Global Outcomes (KDIGO) Classifications. Clin Kidney J 10(3): 332-340.
- Poukkanen M, Vaara ST, Pettilä V, Kaukonen KM, Korhonen AM, et al. (2013) Acute kidney injury in patients with severe sepsis in finnish intensive care units. Acta Anaesthesiol Scand 57(7): 863-872.
- Gameiro J, Agapito Fonseca J, Jorge S, Lopes J (2018) Acute Kidney Injury Definition and Diagnosis: A Narrative Review J Clin Med 7(10): 307.
- Luo X, Jiang L, Du B, Wen Y, Wang M (2014) A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care 8; 18(4): R144.
- Fujii T, Uchino S, Takinami M, Bellomo R (2014) Validation of the kidney disease improving global outcomes criteria for AKI and comparison of three criteria in hospitalized patients. Clin J Am Soc Nephrol 9(5): 848-854.
- Li Z, Cai L, Liang X, Du Z, Chen Y, et al. (2014) Identification and predicting short-term prognosis of early cardiorenal syndrome type 1: KDIGO is superior to RIFLE or AKIN. PLoS One 9(12): 114369.
- Tsai TY, Chien H, Tsai FC, Pan HC, Yang HY, et al. (2017) Comparison of RIFLE, AKIN, and KDIGO classifications for assessing prognosis of patients on extracorporeal membrane oxygenation. J Formos Med Assoc 116(11): 844-851.
- Husain Syed F, Reis T, Kashani K, Ronco C, (2022) Advances in laboratory detection of acute kidney injury. Prac lab med 2:31; e00283.
-
Rebic D*, Hamzic Mehmedbasic A, Dautbegovic E, Hasanspahic S, Herenda V, RibicMrkonja A, Odobasic M. Acute Kidney Injury in Adult Patients: Experience of a Single Center During a 5-Year Period. Annals of Urology & Nephrology. 3(3): 2023. AUN. MS.ID.000564.
-
Acute kidney injury, Causes, Outcome, Adults, prerenal azotemia, Serum creatinine
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






