 Case Report
Case Report
Acute Appendicitis Post Ureteroneocystostomy for Uretero-Vaginal Fistula Causing Diagnostic Dilemma: A Rare Case Report
Abubakar Sadiq Muhammad1*, Abubakar Ibrahim Umar2, Olusegun Goerge Obadele1, Abdullahi Umar Adoke3, Abdullahi Khalid1 and Umar Amina Gambo3
1Institute of Urology and Nephrology of Urology , Usmanu Danfodiyo University, Teaching Hospital, Nigeria
2Department of Surgery, Usmanu Danfodiyo University, Nigeria
3Urologynaecology, Department of Obstetrics and Gynaecology, Nigeria
Abubakar Sadiq Muhammad, Institute of Urology and Nephrology, Usmanu Danfodiyo University, Sokoto, Nigeria.
Received Date: June 23, 2022; Published Date: July 26, 2022
Abstract
Background: Acute appendicitis is a differential diagnosis of acute abdomen. It poses diagnostic challenge more especially when it occurs postoperatively in women. Postoperative acute appendicitis had been reported following surgical and gynecological interventions. There is no report following urological intervention.
The objective of this paper is to report a case of acute appendicitis post ureteroneocystostomy causing diagnostic dilemma.
Case report: We report a 39-year-old woman who developed intermittent colicky right flank pain 3 days after ureteroneocystostomy for ureterovaginal fistula. She had hysterectomy due to abnormal uterine bleeding which was complicated by ureteric injury. There was generalized abdominal tenderness and guarding. She had abdominal reexploration, appendectomy and drainage of abscess due to the findings of acute appendicitis and pelvic abscess. The post-operative period was uneventful, and she was discharged home 10 days postoperatively.
Conclusion: Acute appendicitis may occur postoperatively after urological intervention. A high index of suspicion is required for diagnosis. Incidental appendicectomy following abdominopelvic exploration in the presence of peritonitis and or suppuration may be helpful.
Keywords: Acute abdomen; Appendicitis, Diagnostic dilemma; Post-operative appendicitis; Uretero-neocystostomy; Uretero-vaginal fistula
Abbreviations: PUD: Peptic ulcer disease; Post op: Post operative; CTU: Computerized tomographic scan urography; MRI: Magnetic resonance imaging
Introduction
Acute appendicitis is a common cause of acute abdomen worldwide [1]. Diagnosis of Acute appendicitis in women even with classical symptoms poses diagnostic challenge as it mimics some gynecological conditions such as pelvic inflammatory disease, twisted ovarian cyst and ectopic pregnancy [2]. Therefore, thorough evaluation is required to elucidate the actual cause of acute abdomen which may be only possible intraoperatively.
Postoperative acute appendicitis had been reported following colonoscopy [3], cholecystectomy, choledocholithotomy, hip fracture management, laparoscopic hysterectomy, sigmoid and abdominoperineal resections [4]. It was also reported in pregnant women [5]. Classical features of acute appendicitis with Alvarado score of 7 was reported in a patient being treated for acute pyelonephritis which the features were not present at the point of diagnosis [6].
The causes of postoperative appendicitis are luminal obstruction, bacterial infection, ischemic changes and thrombosis [2,4,7]. Due to the fact that post operative appendicitis is not preventable [3,7] high index of suspicion is required for early diagnosis and prompt intervention.
Although cases of post operative appendicitis have been reported in other disciplines, that have not been reported following urological intervention. The objective of this paper is to report acute appendicitis following ureteroneocystostomy for ureterovaginal fistula constituting a diagnostic dilemma.
Case Summary
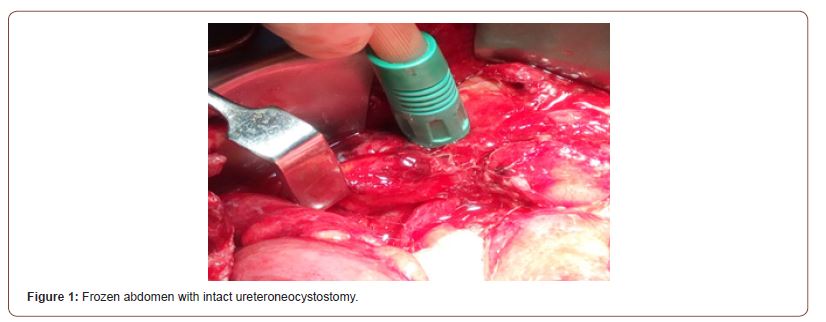
We report a 39-year-old woman who developed intermittent colicky right flank pain 3 days after ureteroneocystostomy for ureterovaginal fistula. She had abdominal hysterectomy due to severe menorrhagia from fibroids 2 weeks prior to presentation. The obstetric history was not contributory. She is a known peptic ulcer disease patient. There was no other comorbidity. She was acutely ill looking, afebrile, not dehydrated and not cyanosed. There was generalized abdominal tenderness and guarding which was more in the lower quadrants. The results of full blood count, urea and electrolyte were within normal limits. Abdominopelvic ultrasound scan and x ray were not remarkable. A diagnosis of generalized peritonitis secondary to adhesive intestinal obstruction was made. She had abdominal reexploration, appendectomy, drainage of pelvic abscess, adhesiolysis and omental wrapping of the bowel. Intraoperative findings were frozen abdomen (Figure 1), pelvic abscess, inflamed appendix with edematous tip and friable base (Figures 2&3). There was oedema of the surrounding caecum and moderate intestinal adhesions. The post-operative period was uneventful, and she was discharged home 10 days postoperatively.


Discussion
Acute appendicitis is a common cause of acute abdomen. It however poses diagnostic difficulty when it occurs postoperatively as it mimics most common postoperative complications [4]. It is also difficult to diagnose in females, as it mimics tubo-ovarian diseases, some of which require medical intervention [6].
Postoperative appendicitis had been reported after colonoscopy, laparoscopic hysterectomy, cholecystectomy, choledocholithotomy, sigmoid and abdominoperineal resection [2,7]. It was however not reported following urological surgeries.
The index patient was a 39-year-old woman who developed features of peritonitis 3 days postoperatively as reported by Almassinokiani F et. al [8], whose patient developed overt symptoms of acute abdomen 3 days post laparoscopic hysterectomy. Similarly, they also offered the patient laparotomy and appendicectomy due to her refusal for laparoscopic appendicectomy. In the index case there was delay in the diagnosis of acute abdomen and intervention as she was thought to have exacerbation of PUD and later urinary leak from the ureteroneocystostomy repair. The age of the patient in the previous report was 42 years which is slightly higher than the age of the index case.
A high index of suspicion is required to diagnose postoperative appendicitis. This is important as it will facilitate prompt diagnosis and intervention with subsequent reduction in morbidity and mortality [3].
The causes of postoperative acute appendicitis are obstruction, bacterial infection, ischemia, and thrombosis [6,7]. Luminal obstruction, thrombosis and bacterial infection are possible in our patient as she developed ureteral injury with infected urinoma and ureterovaginal fistula following hysterectomy for symptomatic fibroid. The ureteroneocystostomy for uretero-vaginal fistula seems to be early at 5-6 weeks post hysterectomy. This may not be adequate for sufficient healing of tissues in the retroperitoneum as a result of urinoma and subsequent peritonitis.
Computerized tomographic scan with urography (CTU) could have given clue about the diagnosis as it was done in a previous study. Because of the presence of peritonitis, clear indication for laparotomy we did not further evaluate the patient with the CTU or magnetic resonance imaging (MRI). This is justifiable as the patient had positive laparotomy.
To the best of our knowledge, there is no report of postoperative acute appendicitis following urological intervention. This will bring to light the possibility of this complication following urological intervention.
We advocate incidental appendicectomy in patients with peritonitis that undergo laparotomy in order to avoid postoperative appendicitis.
Conclusion
Postoperative acute appendicitis may complicate urological interventions. A high index of suspicion is required for early diagnosis and prompt intervention. Routine exploration of appendix in pelvic surgeries associated with peritonitis with or without suppuration may mitigate missing.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Patterson JW, Kashyap S, Dominique E (2022) Acute Abdomen. StatPearls. Treasure Island (FL): StatPearls Publishing.
- Gennaro P (2021) Acute Abdomen in Woman of Childbearing Age: Appendicitis or Pelvic Inflammatory Disease? A Systematic Review. Biomed J Sci Tech Res 35(4): 27900-27906.
- Al Hillan A, Mohamed M, Chien D, Alshami A, Arif F (2020) Postcolonoscopy Appendicitis: A Delayed Complication. Cureus. 12(4):
- Arnbjörnsson E (1984) Postoperative acute appendicitis. Ann Chir Gynaecol 73(5): 277-280.
- Akın T, Birben B, Akkurt G, Karaca O, Dönmez M, et al (2021). Acute Appendicitis During Pregnancy: A Case Series of 42 Pregnant Women. Cureus. 13(8): e17627.
- Ozkan B, Ustun C, Coskuner ER (2021) Acute appendicitis coexisting with acute pyelonephritis causing diagnostic dilemma: a case report. Afr J Urol 27, 71.
- Hirata K, Noguchi J, Yoshikawa I, Tabaru A Nagata N et al, (1996) Acute appendicitis immediately after colonoscopy. Am J Gastroenterol 9(10): 2239-2240.
- Almassinokiani F, Ghoraian M, Akbari H, Almasi A, Pazooki A, et al (2012) Acute Appendicitis Following Laparoscopic Hysterectomy. J Minim Invasive Surg Sci 1(2): 74-76.
-
Bryce A Baird*, Haley Glasser, Tina Solari and Andrew A Stec. Optimized Framework for a Multidisciplinary Outpatient Clinic for Children with Elimination Disorders. Annal Urol & Nephrol. 3(1): 2022. AUN.MS.ID.000558.
-
Acute abdomen, Appendicitis, Diagnostic dilemma, Post-operative appendicitis, Uretero-neocystostomy, Uretero-vaginal fistula
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






