 Research Article
Research Article
Percutaneous Nephrolithotomy or Retrograde Intrarenal Surgery with Flexible Ureteroscopes? A Systematic Review and Meta-Analysis of The Management of Renal Stones Larger Than 2 cm
Tianmin Li1, Chengjie Zhong2, Luofu Wang3*
1Department of Urology, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou, Jiangsu Province, China
2The Second Clinical Medical College, Chongqing Medical University, Chongqing, China
3Department of Urology, Daping Hospital, Army Medical University, Chongqing, China
Luofu Wang, Professor, Department of Urology, Daping Hospital, Army Medical University, China Tianmin Li and Chengjie Zhong contributed equally to this work.
Received Date:March 06, 2024; Published Date:March 14, 2024
Abstract
Objective: The purpose of this study was to review systematically the efficacy and safety of percutaneous nephrolithotomy (PCNL) and
retrograde intrarenal surgery (RIRS) for the treatment of renal stones larger than 2 cm.
Methods: Electronic databases such as the Cochrane Library, PubMed, Embase, and Wanfang Data were searched for studies that compared
PCNL versus RIRS for treating renal stones larger than 2 cm from January 1, 2010, to December 1, 2022. Using inclusion and exclusion criteria,
relevant literature was strictly screened. RevMan 5.4 software was used to perform a meta-analysis of the data.
Results: A total of 4 randomized controlled studies and 17 nonrandomized controlled studies, with a total of 3231 patients (1839 in the PCNL
group and 1392 in the RIRS group) were included in this study. The initial stone clearance rate (odds ratio (OR) = 0.31; 95% CI [0.20, 0.47]; P <
0.00001) and final stone clearance rate (OR = 0.32; 95% CI [0.26, 0.41]; P < 0.00001) were significantly better in the PCNL group than in the RIRS
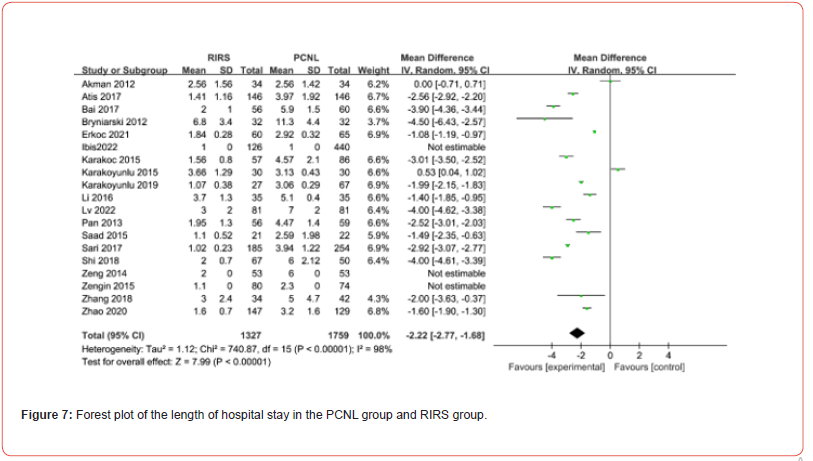
group. Hemoglobin drop (WMD = -0.78; 95% CI [-1.03, -0.53]; P < 0.00001) and length of hospital stay (WMD = -2.22; 95% CI [-2.77], -1.68]; P <
0.00001) were significantly better in the RIRS group than in the PCNL group. The incidence of postoperative complications in both groups (OR=0.91;
95%CI [0.75, 1.11]; P =0.35) had no statistical significance.
Conclusion: PCNL and RIRS are both safe and effective surgical methods for the treatment of renal stones larger than 2 cm. PCNL is superior
to RIRS in stone clearance rate, which supports PCNL as the preferred treatment. RIRS has fewer severe complications and faster postoperative
recovery. RIRS can also achieve satisfactory stone clearance rate through auxiliary or staged procedure. Therefore, RIRS can be used as an alternative
treatment for PCNL.
Keywords: Percutaneous nephrolithotomy; retrograde intrarenal surgery; flexible ureteroscopy; renal stones; meta-analysis; systematic review
Introduction
Renal stones are common diseases of the urinary system, with an annual incidence of approximately 8 in 1,000 [1]. The European Association of Urology (EAU) and American Urological Association (AUA) recommend PCNL as the preferred method for the treatment of renal stones larger than 2 cm, and RIRS using a flexible ureteroscope (FURS) is recommended as a second-line treatment after PCNL [2,3]. Although the success rate of PCNL exceeds 95%, it is an invasive approach, and there are obvious complications, including urinary extravasation (7.2%), bleeding requiring blood transfusion (11.2-17.5%), postoperative fever (21-32.1%), sepsis (0.3-4.7%), colon injury (0.2-0.8%) and pleural injury (0.0-3.1%), etc.
Due to advances in the design and fabrication of modern flexible ureteroscopes, for example, reduced diameter, increased resolution, improved light diffusion, and expanded field of view, RIRS has been widely considered a promising alternative to PCNL for larger renal stones [4-7]. Therefore, the efficacy and safety of PCNL and RIRS for the treatment of larger renal stones (>2 cm) are important issues that need to be evaluated and discussed. The purpose of this study was to conduct a meta-analysis of relevant published articles, update the efficacy and safety of PCNL and RIRS for the treatment of renal stones larger than 2 cm, and compare and analyze the respective advantages of the 2 treatment methods to provide more objective evidence for clinical treatment.
Materials and Methods
Search Strategy
For this meta-analysis, electronic databases such as the Cochrane Library, PubMed, Embase, Springer, CNKI, and Wanfang Data were searched. The retrieval and publication period were from January 1, 2010, to December 1, 2022. The Chinese key words for the searches were “percutaneous nephrolithotomy”, “flexible ureteroscopy”, “upper urinary tract calculi”, “nephrolithiasis,” etc., and the English key words for the searches were “percutaneous nephrolithotomy”, “PCNL”, “flexible ureteroscopy”, “FURS”, “retrograde intrarenal surgery”, “RIRS”, “renal”, “pelvis”, “upper ureter”, “kidney”, “calculus”, “stone” and related synonyms and variants.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows:
a) Research subjects – patients diagnosed with upper
urinary tract calculi (kidney, renal pelvis and calyces, and upper
ureter) by imaging examinations such as ultrasound, kidneys,
ureters, and bladder (KUB), intravenous pyelography (IVP),
computed tomography (CT), with the diameter of the calculi > 2
cm.
b) Study type – randomized controlled trials (RCTs) and
nonrandomized controlled studies (case-control studies,
cohort studies) of RIRS and PCNL for the treatment of renal
stones larger than 2 cm.
c) Outcome indicators – final stone clearance rate (SFR),
complication rate, operation time, hemoglobin decline, length
of hospital stay, etc.
The exclusion criteria were as follows:
a) Studies not belonging to controlled clinical trials.
b) Conference abstracts, reviews, case reports and metaanalyses.
c) Incomplete or vague literature data and unextractable
corresponding data and results.
d) Studies related to stones < 2cm.
e) Research subjects/object are pregnant women, horseshoe
kidney, patients with severe cardiopulmonary Insufficiency or
with contraindications to surgery, etc.
f) Language other than Chinese or English.
g) Original text could not be obtained.
Research Methods
Two authors independently read and organized the literature, screened eligible literature using the inclusion and exclusion criteria, and conducted full-text readings, quality risk assessments and data extraction of the included literature. In case of inconsistent results after cross-referencing, agreement was reached through third-party discussions. The following data were extracted in this study: name of the first author, publication time, type of study design, number of enrolled subjects, intervention measures, outcome indicators, and literature quality scores.
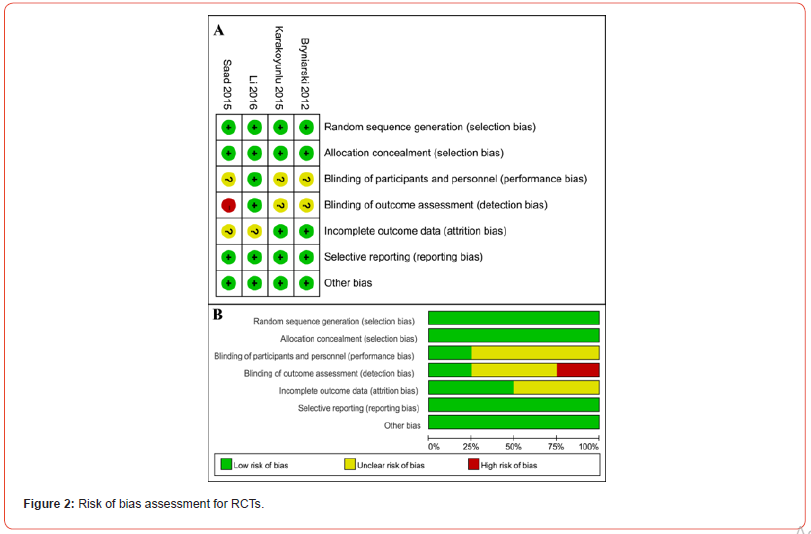
Quality Evaluation and Bias Analysis
This study divided the included literature into 2 categories: experimental research and observational research. The level of evidence of each included study was rated using the Oxford Centre for Evidence-Based Medicine criteria [8]. For experimental studies (RCTs), the Cochrane collaboration’s tool for assessing risk of bias was used. The results of the literature evaluation were divided into 3 types: “high risk of bias,” “low risk of bias” and “uncertain risk of bias.” The quality of the literature was assessed using the modified Jadad scale [9,10], with a total score of 7 points; 4-7 points were considered high-quality experiments. For observational studies (such as case-ontrol studies), the Newcastle-Ottawa Scale (NOS) was used [11]; the total evaluation score was 9 points, with 5-9 points indicating higher quality experiments.
Statistical Methods
RevMan 5.4 software was used for the meta-analysis. A heterogeneity test was carried out for each study statistic. The test level was set to P ≥ 0.1, and when I2 < 50% (there was homogeneity among studies), a fixed effect model was used to calculate the combined statistic; otherwise, a random effect model was used. The odds ratio (OR) and weighted mean (WMD) were used to calculate summary statistics for dichotomous variables and continuous variables, respectively, and 95% confidence intervals (CIs) are reported for ORs and WMDs. The probability P value of the pooled effect statistic was determined using the Z test, and statistical significance was defined as P < 0.05. A funnel plot was used to detect potential publication bias.
Results
Basic Characteristics and Quality Evaluation of The Literature Included in The Analyses
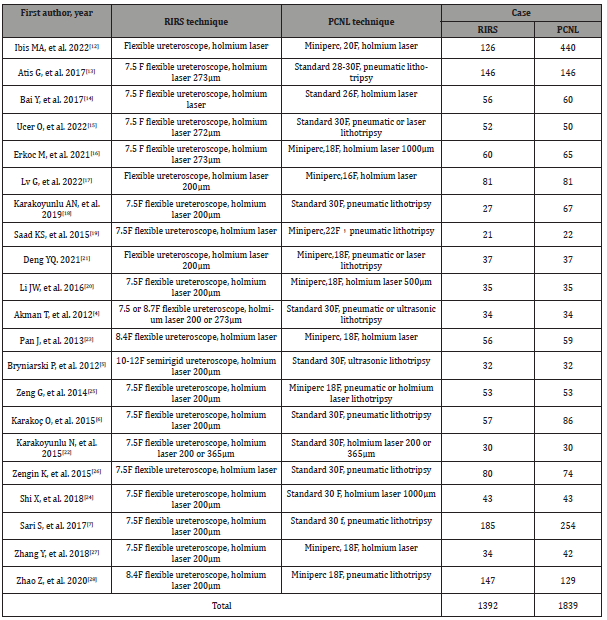
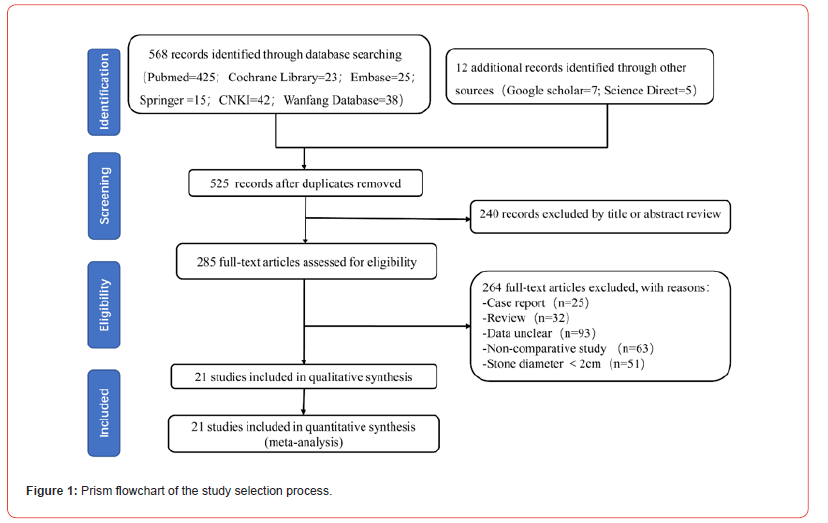
A total of 580 documents were retrieved from the relevant databases using the described search strategy, and 55 duplicate documents were excluded. After reading the titles and abstracts, 457 documents that did not meet the inclusion criteria were excluded. After reading the full text of the remaining 68 papers, some papers were excluded using the exclusion criteria, e.g., incomplete literature data, index that could not be included or wrong data, leaving 21 eligible papers [12-28] (Table 1, Figure 1). Four were RCTs with a level of evidence of 2b. The risk of bias was assessed for each RCT using the Cochrane risk of bias. The risk assessments included “high risk,” “unclear” and “low risk” (Figure 2). The quality of the literature was scored using the modified Jadad scale (4-6 points). The 17 other publications were observational studies (case-control studies and cohort studies), and the level of evidence was 3b. The NOS score for literature quality was 5-8 points (Table 1). In the included studies, there were 1839 patients in the PCNL group and 1392 in the RIRS group (Table 2).
Table 1:General characteristics of the included studies.
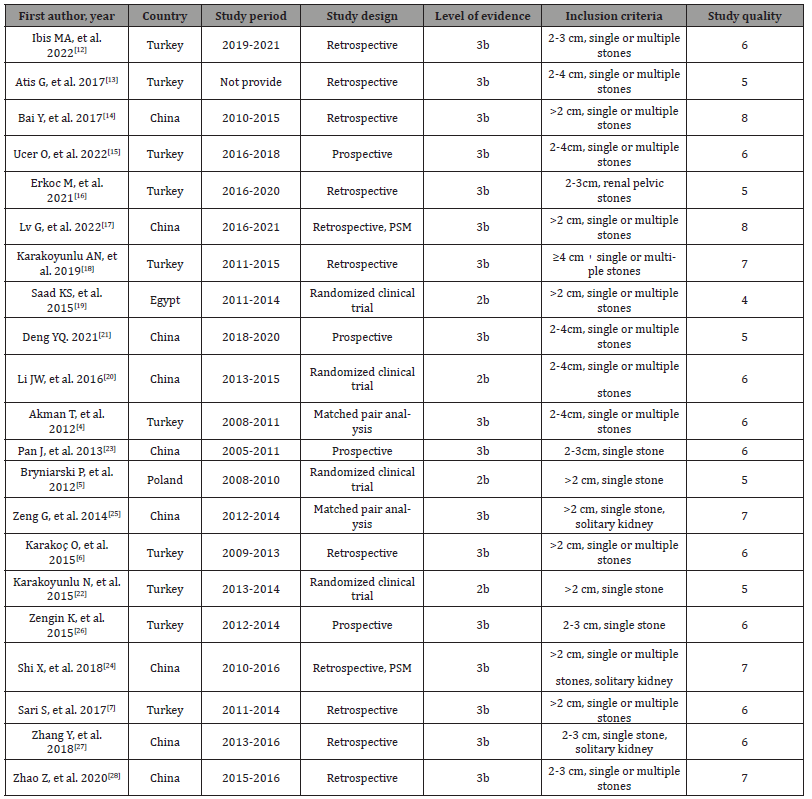
Table 2:Treatment methods in each included study.
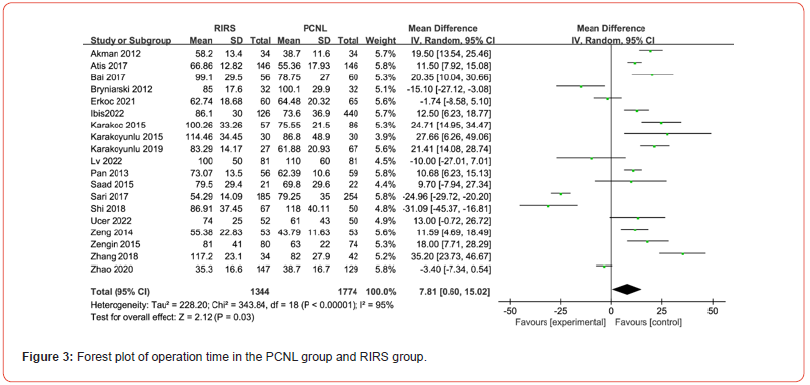
Meta-Analysis of Related Outcome indicators Operation Time
Nineteen studies included this outcome indicator, and the heterogeneity test (P < 0.00001; I² = 95%) indicated that there was a significant difference among the studies; therefore, a random effect model was used for the meta-analysis. The results indicated that the operative time was significantly shorter in the PCNL group than in the RIRS group (WMD = 7.81; 95% CI [0.60, 15.02]; P = 0.03) (Figure 3).
Initial Stone Clearance Rate
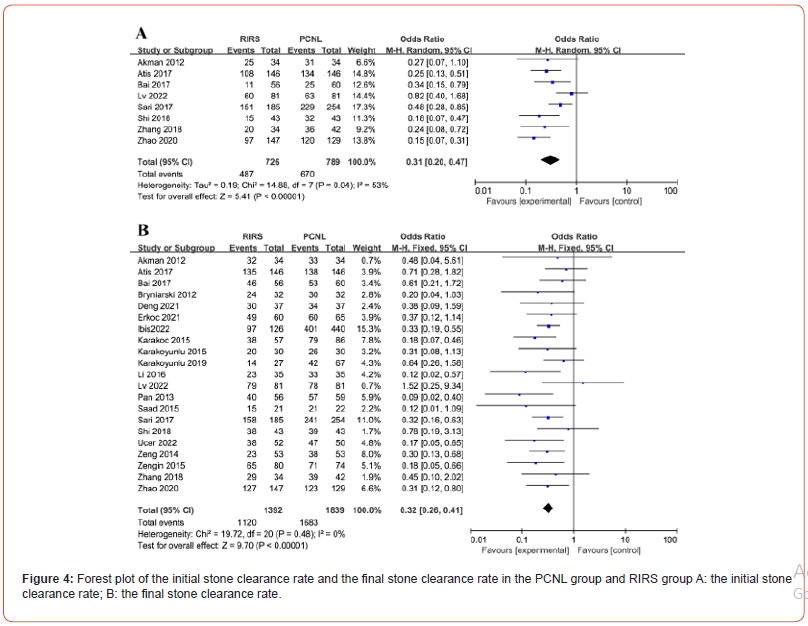
Initial stone clearance rate means the stone clearance rate after first procedure (one session). Eight studies included this outcome indicator, and the heterogeneity test (P = 0.04; I² = 53%) indicated that there was a significant difference among the studies; therefore, a random effect model was used for the meta-analysis. The results indicated that the initial stone clearance rate was higher in the PCNL group than in the RIRS group; the difference was significant (OR = 0.31; 95% CI [0.20, 0.47]; P < 0.00001) (Figure 4A).
Final Stone Clearance Rate
All included studies included this outcome measure. The heterogeneity test (P = 0.48; I² = 0%) indicated that there was no significant difference among the studies; therefore, a fixed effect model was used for the meta-analysis (Figure 4). The results indicated that the final stone clearance rate was significantly higher in the PCNL group than in the RIRS group (OR = 0.32; 95% CI [0.26, 0.41]; P < 0.00001) (Figure 4B).
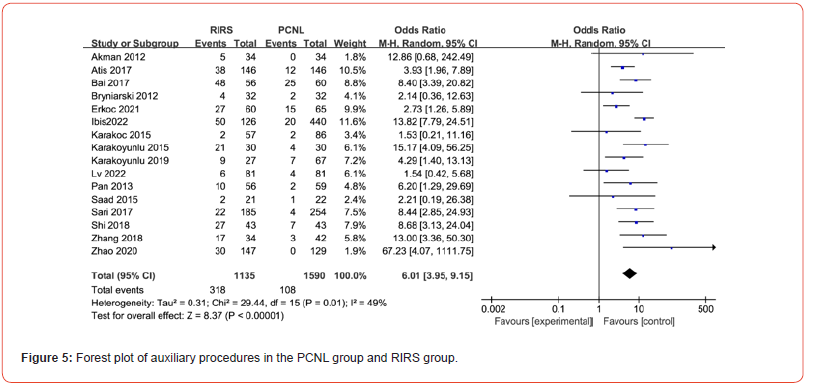
Auxiliary Procedure
If stone removal is unsatisfactory after the first procedure, further procedure, such as extracorporeal shock wave lithotripsy, RIRS or PCNL, is required to address the residual stone. Sixteen studies included this outcome measure, and the heterogeneity test (P = 0.01; I² = 49%) indicated that there was a significant difference among the studies; therefore, a random effect model was used for the meta-analysis. The results showed that the number of patients requiring auxiliary procedures were significantly lower in the PCNL group than in the RIRS group (OR = 6.01; 95% CI [3.95, 9.15]; P < 0.00001) (Figure 5), which means that RIRS needs auxiliary or staged procedure in more patients to improve stone clearance rate.
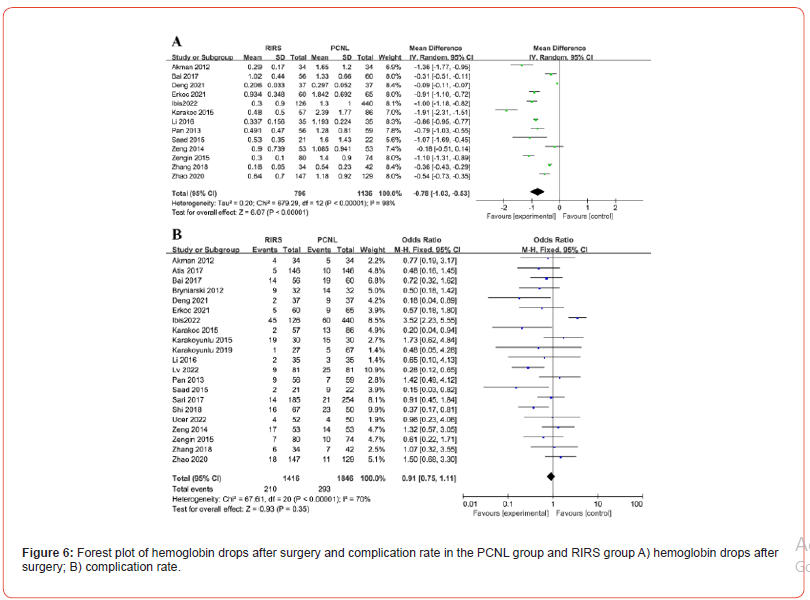
Hemoglobin Drop After Surgery
Thirteen studies included this outcome indicator, and the heterogeneity test (P < 0.00001; I² = 98%) indicated that there was a significant difference among the studies; therefore, a random effect model was used for the meta-analysis (Figure 6). The results indicated that the decrease in hemoglobin was significantly greater in the PCNL group than in the RIRS group (WMD = -0.78; 95% CI [-1.03, -0.53]; P < 0.00001) (Figure 6A).
Complication Rate
All studies included this outcome indicator, and the heterogeneity test (P < 0.00001; I² = 70%) indicated that there was a significant difference among the studies; therefore, a random effect model was used for the meta-analysis. The results showed that there was no significant difference in the incidence of complications between the PCNL group and the RIRS group (OR = 0.91; 95% CI [0.75, 1.11]; P = 0.35) (Figure 6B).
Length of Hospital Stay
Nineteen studies included this outcome indicator, and the heterogeneity test (P < 0.00001; I² = 98%) indicated that there was a significant difference among the studies; therefore, a random effect model was used for the meta-analysis. The results showed that length of hospital stay was significantly shorter in the RIRS group than in the PCNL group (WMD=-2.22; 95% CI [-2.77, -1.68]; P < 0.00001) (Figure 7).
Discussion
Currently, the main treatment for renal stones is minimally invasive surgery. Both the EAU and AUA recommend PCNL as the first-line treatment for renal stones larger than 2 cm. Although PCNL has a high stone clearance rate, the complication rate is also high [29,30]. The most common complications are sepsis and bleeding, which may require a blood transfusion or even embolization in severe cases, with an overall mortality rate of 0.3% [31-33]. To reduce these risks, many clinicians have replaced PCNL with RIRS. For larger stone burdens, staged treatment can be used to obtain higher stone clearance rates [34-37]. Some research reports have shown that the overall stone clearance rate with a single RIRS procedure can be as high as 92% [38,39]. Some scholars propose that RIRS can achieve the same stone clearance rate as PCNL for the treatment of renal pelvis stones larger than 2 cm and has the advantages of being minimally invasive and safe, with a quick postoperative recovery [40]. With continuous advancements in surgical techniques and improvements in various medical devices, more feasible solutions have been provided for the treatment of renal stones larger than 2 cm.
The stone clearance rate is the most intuitive evaluation measure of treatment effects. In this study, the meta-analysis indicated that both the initial stone clearance rate and the final stone clearance rate after auxiliary procedures was significantly higher for PCNL than for RIRS, indicating that PCNL has unique advantages in stone removal. Additionally, the analysis indicated that for renal stones larger than 2 cm, more repeated RIRS treatments are required to achieve a higher stone clearance rate. Although some studies suggest that the cost of multiple RIRS treatments is still lower than that of a single PCNL, but the cost is difficult to calculate in terms of time costs and other factors such as anesthesia damage to the body, which may also be another influencing factor for recommending RIRS as a second-line treatment for large renal stones. Postoperative complications are important indicators for evaluating the safety of related surgical methods. Although the meta-analysis showed that there was no significant difference in the incidence of complications between the PCNL group and the RIRS group, the postoperative hemoglobin level was significantly lower in the PCNL group than in the RIRS group.
Moreover, serious complications such as severe bleeding requiring blood transfusions or embolisms, pleural injuries, ileal injuries, and even cardiac arrest, have been reported for PCNL; therefore, RIRS appears to be safer than PCNL. Notably, there is a risk of urosepsis associated with greater stone burden, and the use of access sheath in RIRS effectively reduces intrarenal perfusion pressure, which can prevent the occurrence of urosepsis [41,42]. The complication rate of RIRS decreased further as the body size of ureteroscope decreased, from 6.6% to 1.5% [43]. RIRS is also a safer option for patients with solitary kidneys, spinal deformities, or coagulation disorders [44,45]. In addition, the operative time varies greatly between studies, and this meta-analysis indicated that the operation time for PCNL is shorter, which may be related to RIRS requiring the use of thinner optical fibers, having lower lithotripsy efficiency and a longer in vivo path, and involving inconvenient maneuvers, especially for calyx calculus.
In terms of the length of hospital stay, that for patients who
undergo RIRS is significantly shorter than that for patients who
undergo PCNL, with an average difference of 2.2 days, which means
that patients recover faster after RIRS and can return to normal
life and work earlier, which in turn leads to less economic loss. The
potential limitations of this study are as follows:
a) The definition of stone clearance rate among the included
studies is not completely consistent, and there may be reporting
bias.
b) There is a lack of further stratified analysis and
comparison of stone size and calyx distribution, and there may
be differential results.
c) This study included many retrospective studies, with only
4 RCTs, resulting in a relatively low level of evidence. Therefore,
more high-quality RCTs are needed to verify and improve these
results.
Conclusion
This meta-analysis indicated that both PCNL and RIRS are safe and effective surgical methods for the treatment of renal stones larger than 2 cm. PCNL has unique advantages in terms of stone clearance rate, while RIRS is less invasive with fewer severe complications and is associated with a faster postoperative recovery, and a satisfactory stone clearance rate can also be achieved through repeated procedures. It is even a better choice than PCNL in certain specific cases such as spinal deformities, coagulation disorders and isolated kidneys.
Acknowledgments
We thank Dr. Jianghua Wan from Department of Urology, Chongqing Daping Hospital for his valuable proposals to our manuscript.
Authorship Contribution Statement
Tianmin Li: Methodology (equal); writing – original draft (lead); formal analysis (lead); Data curation (equal); Formal analysis(equal). Chengjie Zhong: Methodology (equal); Software (lead); writing – original draft (supporting); Data curation (equal); Formal analysis (equal). Luofu Wang: Conceptualization (lead); Writing – review and editing (lead).
Author Disclosure Statement
No conflict of interest exists.
Funding Statement
None.
References
- Fontenelle LF, Sarti TD (2019) Kidney Stones: Treatment and Prevention. Am Fam Physician 99(8): 490-496.
- Assimos D, Krambeck A, Miller NL, Monga M, Murad M, et al. (2016) Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART I. J Urol 196(4): 1153-1160.
- Skolarikos A, Neisius A, Petřík A, Somani B, Thomas K, et al. (2022) EAU Guidelines on urolithiasis.
- Akman T, Binbay M, Ozgor F, Ugurlu M, Tekinarslan E, et al. (2012) Comparison of percutaneous nephrolithotomy and retrograde flexible nephrolithotripsy for the management of 2-4 cm stones: a matched-pair analysis. BJU Int 109(9): 1384-1389.
- Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, et al. (2012) A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol 26(1): 52-57.
- Karakoç O, Karakeçi A, Ozan T, Firdolaş F, Tektaş C, et al. (2015) Comparison of retrograde intrarenal surgery and percutaneous nephrolithotomy for the treatment of renal stones greater than 2 cm. Turk J Urol 41(2): 73-77.
- Sari S, Ozok HU, Cakici MC, Ozdemir H, Bas O, et al. (2017) A Comparison of Retrograde Intrarenal Surgery and Percutaneous Nephrolithotomy for Management of Renal Stones ≥2 CM. Urol J 14(1): 2949-2954.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS (1996) Evidence based medicine: what it is and what it isn't. BMJ 312(7023): 71-72.
- Greenhalgh T (1997) Assessing the methodological quality of published papers. BMJ 315(7103): 305-308.
- Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, et al. (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord 12(3): 232-236.
- Wells GSB, O’Connell D, Peterson J, Welch V, Losos M, et al. (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis.
- Ibis MA, Gokce MI, Babayigit M, Yitgin Y, Karagoz M, et al. (2022) Could retrograde intrarenal surgery be a safe and effective alternative to mini-percutaneous nephrolithotomy in the management of relatively large (20-30 mm) stones? A critical evaluation. Int Urol Nephrol 54(9): 2141-2148.
- Atis G, Culpan M, Pelit ES, Canakci C, Ulus I, et al. (2017) Comparison of Percutaneous Nephrolithotomy and Retrograde Intrarenal Surgery in Treating 20-40 mm Renal Stones. Urol J 14(2): 2995-2999.
- Bai Y, Wang X, Yang Y, Han P, Wang J (2017) Percutaneous nephrolithotomy versus retrograde intrarenal surgery for the treatment of kidney stones up to 2 cm in patients with solitary kidney: a single centre experience. BMC Urol 17(1): 9.
- Ucer O, Erbatu O, Albaz AC, Temeltas G, Gumus B, et al. (2022) Comparison stone-free rate and effects on quality of life of percutaneous nephrolithotomy and retrograde intrarenal surgery for treatment of renal pelvis stone (2-4 cm): A prospective controlled study. Curr Urol 16(1): 5-8.
- Erkoc M, Bozkurt M (2021) Comparison of Mini-Percutaneous Nephrolithotomy and Retrograde Intrarenal Surgery for Renal Pelvic Stones of 2-3 cm. J Laparoendosc Adv Surg Tech A 31(6): 605-609.
- Lv G, Wang K, Zhang Z, Zhou C, Li Y, et al. (2022) Comparison of flexible ureteroscopy and mini-percutaneous nephrolithotomy in the treatment for renal calculi larger than 2 cm: a matched-pair analysis. Urolithiasis 50(4): 501-507.
- Karakoyunlu AN, Cakici MC, Sari S, Hepsen E, Ozok H, et al. (2019) Comparison of Retrograde Intrarenal Surgery and Percutaneous Nephrolithotomy Methods For Management of Big- Sized Kidney Stones (≥4 cm): Single Center Retrospective Study. Urol J 16(3): 232-235.
- Saad KS, Youssif ME, Al Islam Nafis Hamdy S, Fahmy A, Hanno A, et al. (2015) Percutaneous Nephrolithotomy vs Retrograde Intrarenal Surgery for Large Renal Stones in Pediatric Patients: A Randomized Controlled Trial. J Urol 194(6): 1716-1720.
- LI JW, Wang F, Cai FZ (2016) A Comparison Between Staged Flexible Ureteroscopic Lithotripsy and Minimally Invasive Percutaneous Nephrolithotomy for Pelvis Stones 2-4 cm in Diameter: A Randomized Controlled Study (Chinese). Chinese Journal of Minimally Invasive Surgery 16(10): 884-888.
- Deng YQ (2021) Flexible Ureteroscopic Lithotripsy and Minimally Invasive Percutaneous Nephrolithotomy Clinical effect analysis of 2 ~ 4 cm renal stones (Chinese). Henan Journal of Surgery 27(4): 65-67.
- Karakoyunlu N, Goktug G, Şener NC, Zengin K, Nalbant I, et al. (2015) A comparison of standard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: a prospective randomized study. Urolithiasis 43(3): 283-287.
- Pan J, Chen Q, Xue W, Chen Y, Xia L, et al. (2013) RIRS versus mPCNL for single renal stone of 2-3 cm: clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis 41(1): 73-78.
- Shi X, Peng Y, Li X, Wang Q, Li L, et al. (2018) Propensity Score-Matched Analysis Comparing Retrograde Intrarenal Surgery with Percutaneous Nephrolithotomy for Large Stones in Patients with a Solitary Kidney. J Endourol 32(3): 198-204.
- Zeng G, Zhu W, Li J, Zhao Z, Zeng T, et al. (2015) The comparison of minimally invasive percutaneous nephrolithotomy and retrograde intrarenal surgery for stones larger than 2 cm in patients with a solitary kidney: a matched-pair analysis. World J Urol 33(8): 1159-1164.
- Zengin K, Tanik S, Karakoyunlu N, Sener N, Albayrak S, et al. (2015) Retrograde intrarenal surgery versus percutaneous lithotripsy to treat renal stones 2-3 cm in diameter. Biomed Res Int 2015: 914231.
- Zhang Y, Wu Y, Li J, Zhang G (2018) Comparison of Percutaneous Nephrolithotomy and Retrograde Intrarenal Surgery for the Treatment of Lower Calyceal Calculi of 2-3 cm in Patients with Solitary Kidney. Urology 115: 65-70.
- Zhao Z, Sun H, Zeng T, Deng T, Liu Y, et al. (2020) An easy risk stratification to recommend the optimal patients with 2-3 cm kidney stones to receive retrograde intrarenal surgery or mini-percutaneous nephrolithotomy. Urolithiasis 48(2): 167-173.
- Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, et al. (2011) The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, complications, and outcomes in 5803 patients. J Endourol 25(1): 11-17.
- Wiesenthal JD, Ghiculete D, Honey RJ, Pace KT (2011) A comparison of treatment modalities for renal calculi between 100 and 300 mm2: are shockwave lithotripsy, ureteroscopy, and percutaneous nephrolithotomy equivalent? J Endourol 25(3): 481-485.
- Aminsharifi A, Irani D, Eslahi A (2014) Massive hemorrhage after percutaneous nephrolithotomy: saving the kidney when angioembolization has failed or is unavailable. Int J Surg 12(8): 872-876.
- Unsal A, Resorlu B, Atmaca AF, Diri A, Goktug H, et al. (2012) Prediction of morbidity and mortality after percutaneous nephrolithotomy by using the Charlson Comorbidity Index. Urology 79(1): 55-60.
- Reddy SV, Shaik AB (2016) Outcome and complications of percutaneous nephrolithotomy as primary versus secondary procedure for renal calculi. Int Braz J Urol 42(2): 262-269.
- Al-Qahtani SM, Gil-Deiz-de-Medina S, Traxer O (2012) Predictors of clinical outcomes of flexible ureterorenoscopy with holmium laser for renal stone greater than 2 cm. Adv Urol 2012: 543537.
- Palmero Martí JL, Ganau Ituren A, Valls González L (2017) Current results of RIRS and comparison with PCNL (Spanish). Arch Esp Urol 70(1): 147-154.
- Pevzner M, Stisser BC, Luskin J, Yeamans JC, Lucey MC, et al. (2011) Alternative management of complex renal stones. Int Urol Nephrol 43(3): 631-638.
- Cohen J, Cohen S, Grasso M (2013) Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU Int 111(3 Pt B): E127-E131.
- Rodríguez-Monsalve Herrero M, Doizi S, Keller EX, Coninck V, Traxer O (2018) Retrograde intrarenal surgery: An expanding role in treatment of urolithiasis. Asian J Urol 5(4): 264-273.
- Ho A, Sarmah P, Bres-Niewada E, Somani B (2017) Ureteroscopy for stone disease: expanding roles in the modern era. Cent European J Urol 70(2): 175-178.
- El Hamed AMA, Elmoghazy H, Aldahshoury M, Riad A, Mostafa M, et al. (2017) Single session vs two sessions of flexible ureterosopy (FURS) for dusting of renal pelvic stones 2-3 cm in diameter: Does stone size or hardness play a role in number of sessions to be applied?". Turk J Urol 43(2): 158-161.
- Jung H, Osther PJ (2015) Intraluminal pressure profiles during flexible ureterorenoscopy. Springerplus 4: 373.
- Scotland KB, Lange D (2018) Prevention and management of urosepsis triggered by ureteroscopy. Res Rep Urol 10: 43-49.
- Ho CC, Hee TG, Hong GE, Singam P, Bahadzor B, et al. (2012) Outcomes and Safety of Retrograde Intra-Renal Surgery for Renal Stones Less Than 2 cm in Size. Nephrourol Mon 4(2): 454-457.
- Gao X, Peng Y, Shi X, Li L, Zhou T, et al. (2014) Safety and efficacy of retrograde intrarenal surgery for renal stones in patients with a solitary kidney: a single-center experience. J Endourol 28(11):1290-1294.
- Berardinelli F, De Francesco P, Marchioni M, Cera N, Proietti S, et al. (2017) RIRS in the elderly: Is it feasible and safe? Int J Surg 42:147-151.
-
Tianmin Li, Chengjie Zhong, Luofu Wang*. Percutaneous Nephrolithotomy or Retrograde Intrarenal Surgery with Flexible Ureteroscopes? A Systematic Review and Meta-Analysis of The Management of Renal Stones Larger Than 2 cm. Annals of Urology & Nephrology. 4(3): 2024. AUN.MS.ID.000587.
-
Percutaneous nephrolithotomy; retrograde intrarenal surgery; flexible ureteroscopy; renal stones; meta-analysis; systematic review; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






