 Research Article
Research Article
Minimally Invasive Urodynamics: “One-Exam-Fits-All”?
João Antonio Pereira Correia*, Gustavo Brandão Teixeira Leite, Heitor Soares Morais, Bruno de Andrade Salomão, Raphael Moura Xavier Enne, Valter José Fernandes Muller
Department of Urology – Servidores do Estado Federal Hospital, Rio de Janeiro, Brazil
João Antonio Pereira-Correia, Department of Urology – Servidores do Estado Federal Hospital, Rio de Janeiro, Brazil
Received Date:April 09, 2024; Published Date:April 16, 2024
Abstract
Aims: To evaluate whether minimally invasive urodynamics (MIU) is capable of being performed by men with characteristics that may affect the
ability to perform the exam, such as cognitive impairment and increased abdominal circumference.
Methods: Male patients who were on the waiting list for urodynamic assessment with complaints of storage and emptying low urinary tract
symptoms (LUTS) were analyzed in a prospective and randomized manner. All patients underwent the 3 phases of the urodynamic study, with
replacement of the uroflowmetry stage by MIU. Before the exam, patients were asked to fill out, the Brazilian version of the Cognitive Failures
Questionnaire (CFQ) and were classified into three ranges based on the sum of their points: 0–30, 31–60, and 61–100. After completing the exam,
patients had their abdominal circumference measured and were classified into three ranges: 60–90, 91–101, and 102–132 cm.
Results: Sixty-three patients were invited to undergo the urodynamic evaluation with the uroflowmetry phase replaced by the minimally
invasive study, and 62 (98.4%) were able to perform the exam. There was no statistically significant difference between the examination when
considering cognitive data (p = 0.2226) or abdominal circumference (p = 0.9531).
Conclusion: MIU is an excellent option for the diagnosis and therapeutic follow-up of intravesical obstruction in men, even in patients with
increased abdominal circumference or cognitive changes.
Keywords: Minimally invasive urodynamics; low urinary tract symptoms; bladder outlet obstruction; abdominal circumference; cognitive disorders
Introduction
The role of urodynamic assessment for the diagnosis of bladder emptying disorders is well established. Pathological conditions such as bladder outlet obstruction (BOO) and detrusor underactivity, for example, find their gold standard for diagnosis in urodynamics [1]. However, urodynamics offer some challenges as well. It is an invasive, time-consuming, and expensive exam [2] that presents a significant potential for undesirable effects during (embarrassment) and after (dysuria, macroscopic hematuria and urinary tract infection) its implementation [3]. In this context, alternative, minimally invasive options have been gaining ground, especially with regard to the diagnosis of BOO in men – one of the main pieces of information to help make therapeutic decisions in benign prostatic hyperplasia associated with lower urinary tract symptoms (LUTS) [4]. The ultimate objective is to enable early treatment, before an individual develops damage to their detrusor muscle.
Since Schafer and collaborators first described the minimally invasive urodynamics (MIU) method in 1994 [5] many devices and techniques have emerged in this field. Most methods analyze isometric bladder pressure resulting from interruption of urinary flow during the patient’s spontaneous urination. The method developed by D`Ancona and collaborators in 2008 follows the same precepts proposed by Schafer, but with the development of a new device, which must be fitted into the navicular fossa through the external urethral meatus [6]. The method minimizes cost, discomfort, and rates of urinary infection [7]. To implement the MIU, however, patients must have good visualization of the penis since it is up to them to insert (under medical supervision) and hold the device throughout urination. Considering this point, we raised the hypothesis that men with increased abdominal circumference and/or cognitive deficits could have difficulties in carrying out this diagnostic assessment. In this study we aim to evaluate whether MIU is capable of being performed by men with characteristics that may affect the ability to perform the exam, such as cognitive impairment and increased abdominal circumference.
Materials and Methods
After authorization from the local Ethics and Research Committee, male patients who were on the waiting list for urodynamic assessment with complaints of storage and emptying LUTS were analyzed in a prospective and randomized manner. Randomization was performed by computer. Patients were excluded if they had suspicion or presentation of central or peripheral neuropathies, retinopathies, blindness, hand tremor, or diabetes mellitus. All patients underwent the 3 phases of the urodynamic study (uroflowmetry, cistometry and voiding pressure/flow study), with replacement of the uroflowmetry stage by minimally invasive urodynamics. Testing occurred from January to October 2023, in our urodynamic center, using the latest version of DynamedTM (DynamedTM), urodynamic equipment (Dynapack SlimTMHardware and UrocommanderTM Software). All testing followed the recommendations for good practice endorsed by the International Continence Society (ICS) [8-10]. Before the exam, patients were asked to fill out, on their own, the Brazilian version of the Cognitive Failures Questionnaire (CFQ).
This questionnaire is a self-report instrument containing 25 questions about cognitive failures committed by adults on a daily basis. The instrument was standardized for clinical use and validated for use in Brazil [11,12]. The questionnaire has a brief and relatively simple application and provides an ecological variable, representing the frequency, intensity and pattern of cognitive failures that the subject presents in everyday life. The results range from 0 to 100 and higher scores indicate a greater occurrence of cognitive failures. Patients were classified into three ranges based on the sum of their points: 0–30, 31–60, and 61–100. After completing the exam, patients had their abdominal circumference measured using a flexible measuring tape, using the navel as a reference [13]. Patients were classified into three ranges: 60–90, 91–101, and 102–132 cm. Statistical analysis was performed using GraphPad PrismTM software, version 7, applying Kolmogorov– Smirnov’s test for normality analysis. For data with a Gaussian distribution, a comparative intergroup evaluation Student’s t‐test was used. However, for data with a non‐Gaussian distribution, the Kruskal–Walli’s test was used, adopting the standard significance value of p < 0.05.
Results
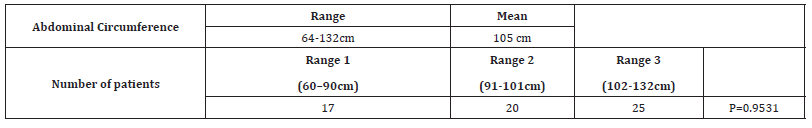
Sixty-three patients were invited to undergo the urodynamic evaluation with the uroflowmetry phase replaced by the minimally invasive study, and 62 (98.4%) were able to perform the exam. Demographic characteristics are shown in Table 1. The only patient who was unable to perform the exam had difficulty fitting the device into his external urethral meatus/navicular fossa. The man’s cognitive data and abdominal circumference measurements were within normal limits. Results of the cognition questionnaire and measurement of the abdominal circumference of the patients who were able to undergo the minimally invasive assessment are shown in Tables 2&3, respectively. There was no statistically significant difference between the examination when considering cognitive data (p = 0.2226) or abdominal circumference (p = 0.9531).
Table 1:Patient`s demographic characteristics.
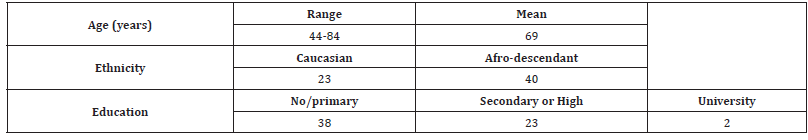
Table 2:Results of the Cognitive Failures Questionnaire (CFQ) of the patients who were able to undergo MIL evaluation.
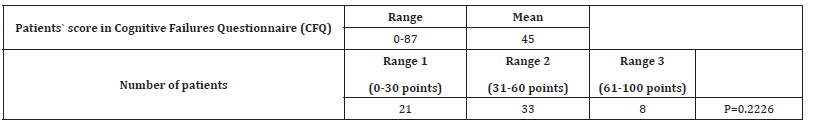
Table 3:Results of the abdominal circumference of the patients who were able to undergo MIU evaluation.
Discussion
Due to its diagnostic accuracy, MIU is a viable and easily repeatable option for identifying BOO and monitoring its treatment, but there are no previous studies evaluating whether this type of exam can be applied to men with high abdominal circumference and/or cognitive impairment. It can be challenging to perform diagnostic procedures on obese individuals. Research in the area of abdominal imaging highlights the difficulty of performing magnetic resonance imaging, computed tomography, and ultrasound in this population [14,15]. Our findings, however, demonstrate that, even in patients with increased abdominal circumference, where difficulty in visualizing the penile extremity is expected, there was no impediment to carrying out the examination. We believe that the patients’ tactile ability, using both hands during urination, to manipulate their own penis and the device, was sufficient to overcome the lack of visualization.
Another question we tried to answer was in regard to the impact of cognitive changes when performing MIU. We know that men with cognitive deficits have greater difficulties in manipulating devices attached to the genitals, as in the case of the artificial urinary sphincter for incontinence. Ballantyne and colleagues report that patients with impaired cognition were more likely to report difficulty with artificial urinary sphincter use compared to those with normal cognition (39% vs. 9%, p = 0.01) [16]. A recent review on the impact of cognitive impairment in urologic implants recommends that: “while data on the association between urologic implants and cognitive impairment are sparse, urologists can provide appropriate preoperative counseling (including recommending against implantation) and can provide closer postoperative monitoring” [17].
In this study we used the CFQ questionnaire as an instrument to measure patients’ cognitive capacity. Even in patients with high CFQ scores, the MIU exam went smoothly, without compromising the analysis of the results. This discrepancy between the manipulation of genital implants and the urodynamic device, in patients with cognitive impairment, likely occurs due to the difference in complexity between these elements. The device that the patient holds adhered to the penis, during urination, is easy to handle and does not require much skill to keep it in place.
Conclusion
Minimally invasive urodynamics is an excellent option for the diagnosis and therapeutic follow-up of intravesical obstruction in men, even in patients with increased abdominal circumference or cognitive changes. We believe that more studies on this topic can help us to establish an increasingly safer diagnosis, significantly reducing the harmful consequences of more invasive tests.
Acknowledgments
No acknowledgments.
Conflict of Interests
None declared.
Funding Statement
There was no funding for this study.
Clinical Trial Registration Number
Not necessary since our study is not based on clinical intervention, but only on observational analysis.
Ethics of Approval Statement
Study approval number by the local ethics committee: 74323617.5.0000.5377.
Patient Consent Statement
Not applicable.
Data Availability Statementt
Not applicable.
Permission to Reproduce Material from Other Sources
We do not use materials from other sources.
References
- Haylen B, D’Ancona C, Oelke M, Herschorn S, Abranches-Monteiro L, et al. (2019) The international continence society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn 38(2): 433-477.
- Gomes CM, Arap S, Trigo-Rocha FE (2004) Voiding dysfunction and urodynamic abnormalities in elderly patients. Rev Hosp Clin Fac Med Sao Paulo 59(4): 206-215.
- Klingler HC, Madersbacher S, Djavan B, Schatzl G, Marberger M, et al. (1998) Morbidity of the evaluation of the lower urinary tract with transurethral multichannel pressure-flow studies. J Urol 159(1): 191-194.
- Sandhu JS, Bixler BR, Dahm P, Goueli R, Kirkby E, Stoffel JT, et al. (2024) Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia (BPH): AUA Guideline amendment 2023. J Urol 211(1): 11-19.
- Schafer W, Kirschner-Hermans R, Jakse G (1994) Non-invasive pressure/ flow measurement for precise grading of bladder outflow obstruction. J Urol 151(Suppl): 323.
- D'Ancona CAL, Bassani JWM, Querne FAO, Carvalho J, Oliveira RRM, et al. (2008) New method for minimally invasive urodynamic assessment in men with lower urinary tract symptoms. Urology 71(1): 75-78.
- D'Ancona CA, Bassani J, Almeida JC (2012) Noninvasive urodynamic evaluation. Int Neurourol J 16(3): 116-121.
- Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, et al. (2002) Good urodynamic practices: uroflowmetry, filling cystometry and pressure‐flow studies. Neurourol Urodyn 21(3): 261‐274.
- Rosier PFWM, Schaefer W, Lose G, Goldman HB, Guralnick M, et al. (2017) International Continence Society Good Urodynamic Practices and Terms 2016: urodynamics, uroflowmetry, cystometry, and pressure‐flow study. Neurourol Urodyn 36(5): 1243‐1260.
- Drake MJ, Doumouchtsis SK, Hashim H, Gammie A (2018) Fundamentals of urodynamic practice, based on International Continence Society good urodynamic practices recommendations. Neurourol Urodyn 37(S6): S50‐S60.
- Paula JJ, Costa DS, Miranda DM, Romano-Silva MA (2018) Brazilian version of the Cognitive Failures Questionnaire (CFQ): cross-cultural adaptation and evidence of validity and reliability. Braz J Psychiatry 40(3): 312-315.
- Bridger RS, Johnsen SÅ, Brasher K (2013) Psychometric properties of the Cognitive Failures Questionnaire. Ergonomics 56(10): 1515-1524.
- Blaha MJ, DeFilippis AP (2021) Multi-Ethnic Study of Atherosclerosis (MESA): JACC Focus Seminar 5/8. J Am Coll Cardiol 77(25): 3195-3216.
- Mancini MC (2001) Diagnostic obstacles and therapeutic challenges in obese patients. Arq Bras Endocrinol Metab 45(6): 584-608.
- Harada T, Obokata M (2020) Obesity-Related Heart Failure with Preserved Ejection Fraction: Pathophysiology, Diagnosis, and Potential Therapies. Heart Fail Clin 16(3): 357-368.
- Ballantyne CC, Sharma D, Rapp DE, Boatman KR, Krzastek SC, et al. (2021) Prevalence of Cognitive Impairment and Sphincter Misuse Among Men with Artificial Urinary Sphincters. Urology 148: 292-296.
- Bryk DJ, Zillioux J, Kennady EH, Sun F, Hasken W, et al. (2023) The impact of cognitive impairment in urologic implants: a narrative review. Transl Androl Urol 12(9): 1426-1438.
-
João Antonio Pereira Correia*, Gustavo Brandão Teixeira Leite, Heitor Soares Morais, Bruno de Andrade Salomão, Raphael Moura Xavier Enne, Valter José Fernandes Muller. Minimally Invasive Urodynamics: “One-Exam-Fits-All”?. Annals of Urology & Nephrology. 4(4): 2024. AUN.MS.ID.000591.
-
Minimally invasive urodynamics; low urinary tract symptoms; bladder outlet obstruction; abdominal circumference; cognitive disorders; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






