 Research article
Research article
Evidence-Based Practice & Strategies in Reducing Catheter Blood Stream Infection in Hemodialysis Patients
Myrna Tayco-Manuel, DNP, MSHI, RN, BSN, CNN, Governor State University, USA
Received Date:October 14, 2024; Published Date:October 25, 2024
Abstract
Patients on hemodialysis are vulnerable and have a substantial risk of getting life threatening infections. The Centers for Disease Control and Prevention (CDC) and Center for Medicare & Medicaid Services (CMS) collaborate to ensure that Dialysis Centers start core interventions to ensure the reduction of dialysis bloodstream infections. The staff members considered the structural element where they used policy and procedure manuals to improve and ensure the process of supplying the Central Venous Catheter (CVC) maintenance care. The purpose of this project is to assess the dialysis staff’s adherence to the evidence-based practices and strategies instituted by CDC. The focus is on the process of assessing the level of knowledge and skills and compliance in following the facility’s protocol and policies. A pre and posttest educational intervention design was used to find the level of understanding of the dialysis staff and their responsibility in applying their knowledge and skills to reduce the infection episodes of their patients during treatment. The audit tools and checklist were the resources for the dialysis member to complete and comply so that catheter related blood stream infection is prevented. Kurt Lewin’s change model and the Plan-Do-Check-Act (PDCA) method are used to guide this project. Lewins’s theory was used to improve patient outcomes, enhance nursing practice, and check health care costs. Overall, the dialysis staff members were able to follow the evidence-based practices and strategies recommended by CDC and the clinical practice guidelines derived from systematic review to achieve a high quality of care.
Keywords:Catheter blood stream infection (CRBSI); hemodialysis (HD); central venous catheter (CVC); end stage renal disease (ESRD); personnel protective equipment (PPE); Center for Disease Control (CDC); evidence-based practice (EBP)
Introduction
The use of vascular catheters is common in both inpatient and outpatient care. In the US, almost three hundred million catheters are used each year; around three million of these are central venous catheters (CVC) also known as central lines [1]. These CVCs have an essential role in modern health care. They are used for IV fluids, blood products, parental, medication and more importantly as an access for hemodialysis and hemodynamic monitoring. The focus of this project is to educate the staff members about catheter care maintenance and assess their knowledge level and skills in reducing catheter infection and check their adherence to evidencebased strategies instituted by CDC. In 2010, the prevalent CVC use increased to 25 % while 80% of patients start HD with a catheter. Due to so many patients using the catheters, trends in patient outcomes lead to high morbidity and mortality caused by infection. Exit site infections, tunnel infections and bacteremia are catheter related infections that have a high rate of having ability to transform into sepsis [2].
Catheter related blood stream infection (CRBSI) is the most common cause of death and major cause of hospitalization. A singlecenter study found that a CRBSI resulted in an average hospital stay of 11 days and cost approximately $23,000 [3]. For this reason, it becomes a safety leading concern. Despite the Fistula First Initiative, 80% of patients start hemodialysis with a central venous catheter [3]. This project is needed to demonstrate improved achievement of the quality outcome measures that have been set for use with CVC’s. Prevention and control of (CRBIs) is necessary to ensure safety and better patient outcome. The End Stage Renal (ESRD) Disease Safety Program advocates the use of to help the clinics prevent healthcare associated infection. Evidence suggested that CRBSIs were preventable with evidence-based educational interventions. It helps in increasing the nurses’ knowledge on the care of the patient with CVC.
It helps HD staff make care safer by following clinical best practices, to create culture of safety by using checklists and other audit tools and engaging with patients and their families (“AHRQ Safety Program for End-Stage Renal Disease Facilities – Toolkit”) (“Agency for Healthcare Research and Quality”) [4]. The CDC published guidelines for CRBSI where it became the standard for all CVC care recommendations. The guidelines known as core interventions recommend hand hygiene, use of personal protection equipment (PPE), chlorhexidine for skin preparations, catheter site dressing regimens and the use of antimicrobial agents, antibiotic lock solution and heparin for tunneled cuff central vein catheters (TCC) related infection, staff education and competency, patient education and engagement, and catheter hub disinfection (Centers for Disease Control and Prevention [CDC], 2016a). Hemodialysis (HD) catheters or central venous catheters (CVCs) are commonly used as vascular access for patients who require hemodialysis. These HD catheters are either non-tunneled (temporary) or tunneled catheters (permanent).
Complications, particularly infections, are a critical problem. It is associated with high rates of morbidity and mortality, prolonged hospitalization and increased medical costs. The cost of central line associated blood stream infection (CLABSI) is costly. Based on the national data from the US Renal data System, hospitalizations for CRBS among HD patients increased since 1993 (National Healthcare Safety Network (NHSN), 2013) [5]and the annual cost to the healthcare system in intensive care units (ICUs) was $296 million to $2.3 billion [6]. Approximately 19% of HD patients died within 12 weeks of the infection. CDC estimates that a particular case can cost as much as $48k or more per episode. Approximately 23,500 CLABSIs were reported to the National Safety Health Network (NSHN) from US hospitals in 2016. It leads to hospital stay, increase morbidity, and raises mortality rate by 12-25% [7].
The Joint Commission (JCAHO) emphasized that intravascular catheter related infections are a significant safety concern in healthcare today. The CRBSI are watched closely to reduce the potentially deadly outcomes as well as the financial burden placed on the healthcare system because of the necessary treatment of these infections [8]. In University of Illinois Medical Center (UIMC), between 4/16/23 to 4/15/2024, 19.4% of the population has a blood stream infection (BSI), twenty-four patients were identified with catheter blood related stream infection from 10/16/23 to 4/15/24. Those patients were from Intensive Care Units (MICU, NSICU, Transplant Unit, SICU, CICU) [9]. They were treated with systemic antibiotic therapy and catheter guidewire exchange. In UIMC Dialysis Center, only two patients from Dec. 2022 to May 2023 were identified with CRBSI. Both patients were treated with systemic antibiotics and antibiotic locks.
Materials
Literature was searched via the resources of Governors State University library. Databases includes the Cumulative Index to Nursing and Allied Health Literature (CINAHL) – 6 articles, Cochrane database of systematic reviews (3 articles), PUBMED (6 articles) & Google Scholar (19,000 articles) from 2000 to 2023. Appropriate and related articles were reviewed and examined. The keywords used in the search are evidence-based practice, catheter related blood stream infection, hemodialysis patients, infection control & prevention, educational intervention. After searching the databases, a selection of these studies was based on the inclusion and exclusion criteria. The following literature review consists of two sections: a specific consideration of the literature which fulfilled the selection criteria that shows the study characteristics and summary of evidence-based recommendation and general review of literature that focuses on prevention of catheter-related blood stream infection in patients on hemodialysis (HD). The search focused only on selecting the articles that met the inclusion criteria. The inclusion criteria included clinical study, clinical trial, meta-analysis, observational study, practice guideline, systematic review and randomized controlled trial, text written in English, articles with full text and abstract available, articles with male and female participants and who are above 18 years old. The exclusion criteria included pediatric literature.
Methods
Questionnaires
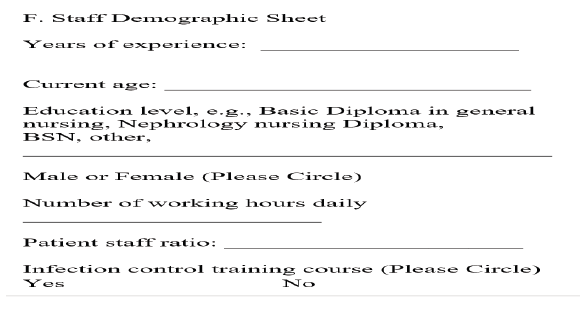
Participants answered a 20-question pretest and posttest (see Appendix A) after completing the competencies, audit tools and checklist. The questionnaires include knowledge about catheter maintenance care and seven questions in demographic sheet (Appendix B). The demographic questionnaire was developed to collect data about participants age, gender, level of education, years of experience, infection control training completion and the number of hours they worked. Pre and posttest questionnaires were knowledge based. The questionnaires covered aseptic techniques, process to obtain blood culture, guidelines for dressing change, the need to avoid femoral insertion site, CRBSI epidemiology and use of barrier precautions during catheter care maintenance. The participants spent 15 minutes of their working hours completing the pre-test; their patient care task was assigned to other staff while they were completing the pre-test & post-test. I collaborated with the Chief Tech to determine time allocation for the tests. The posttest was completed after reviewing the unit policy, audit tool and competency skill checklist completion and educational intervention. The post-test results were discussed with the participants. Tough questions where most of the participants made a mistake were reviewed and discussed. Plan of corrections were addressed.
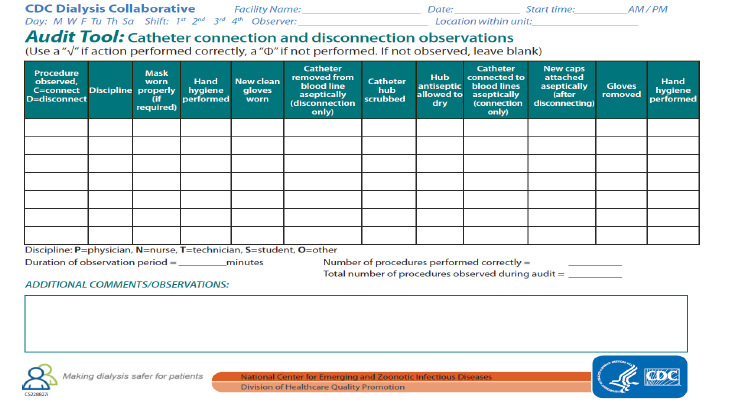
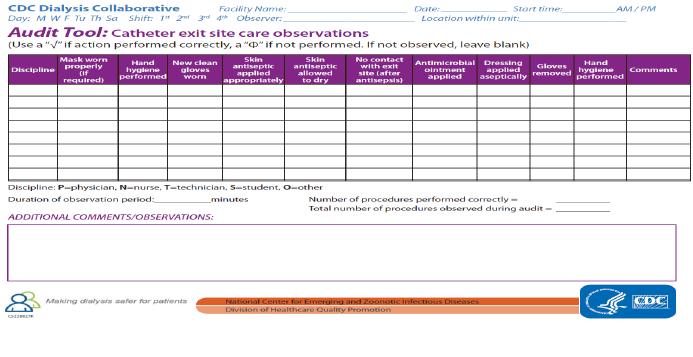
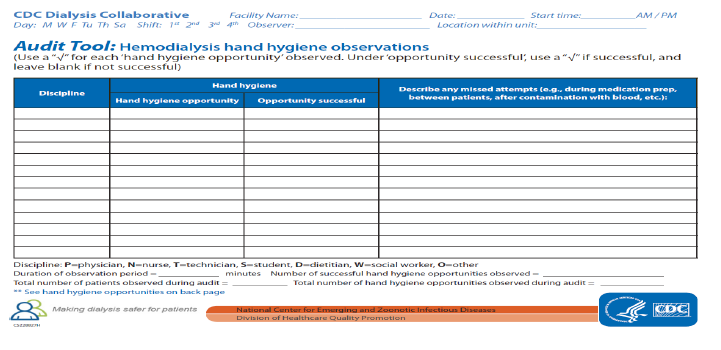
Audit Tools
The audit tool from the CDC was used to check the dialysis staff
compliance. In collaboration with the Chief Tech, the following audit
tools were completed (Center for Disease Control and Prevention,
2017) [10].
a) Catheter- connection – disconnection observations (see
Appendix C).
b) Catheter exit site care observations (see Appendix D).
c) Hemodialysis hand hygiene observations (see Appendix E).
Observations were done on hand hygiene, catheter disconnection and connection and catheter exit-site observation to ensure that the staff members follow correct infection control and prevention procedures.
The educational session presented the necessary information needed by the participants. Views and opinions expressed during the lecture were derived from CDC guidelines, unit policies and procedures of the HD unit. There is no disclosure of any conflicts of interest during the session. The emphasis was on CDC core intervention, signs, and symptoms of CRBSI, definition of CRBSI according to CDC and National Health Safety Network (NSHN) Surveillance, modifiable risk factors and prevention measures based on CDC & CRBSI bundles. The CRBSI bundle includes the following elements such as hand hygiene, sterile barrier precautions (sterile drape, sterile gown and gloves, mask, and cap, choosing the catheter insertion site with avoidance of femoral vein for access in adults, chlorhexidine skin antisepsis and daily review of line necessity and prompt removal of unnecessary lines.
Educational Intervention
The educational session presented the necessary information needed by the participants. Views and opinions expressed during the lecture were derived from CDC guidelines, unit policies and procedures of the HD unit. There is no disclosure of any conflicts of interest during the session. The emphasis was on CDC core intervention, signs, and symptoms of CRBSI, definition of CRBSI according to CDC and National Health Safety Network (NSHN) Surveillance, modifiable risk factors and prevention measures based on CDC & CRBSI bundles. The CRBSI bundle includes the following elements such as hand hygiene, sterile barrier precautions (sterile drape, sterile gown and gloves, mask, and cap, choosing the catheter insertion site with avoidance of femoral vein for access in adults, chlorhexidine skin antisepsis and daily review of line necessity and prompt removal of unnecessary lines.
Results
The data collection included the procedures to collect data and time requirement. Prior to data collection, Institutional Review Board (IRB) approval was secured. A demographic tool (see Appendix B) was developed. The responses were kept confidential and kept in a locked cabinet. Coding was the process of transforming data into numerical symbols for easier entry to the computer. The codebook was developed before data collection. The participant’s study code was written on each form completed and the forms were audited. The data collected was backed up and stored on a local C-drive and flash drive to avoid loss of data due to computer crashes. The project used a pretest-posttest educational intervention design to assess the knowledge level of the dialysis staff. According to Grove, et.al. [11] The design helped investigate the effectiveness of nursing intervention in achieving the desired outcome in a natural setting. Below is the timeline for the educational intervention.
Table 1:
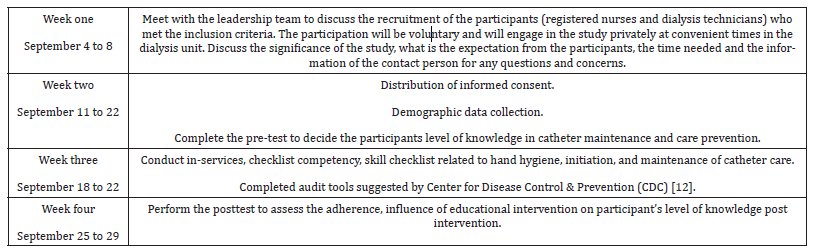
The pre-test questionnaire was distributed to nurses and dialysis technicians who agreed to participate. The participants willingly engaged in the scheduling of the pretest and posttest to minimize scheduling difficulties and disruption of workflow. Twenty participants completed the pretest, and they were allowed 10-15 minutes of their working hours, their patients and other duties were assigned to other staff while they were taking their test. The completed questionnaires and demographic sheets were collected, placed in a folder in a locked file drawer and entered electronically to ensure the participant’s privacy. The test was graded manually. Data from each participant was kept together until initiation of analysis. The pre and post test results were completed by the participants to be analyzed. Analysis of data included descriptive statistics (percent, means and standard deviation). Analysis was used to decide the relationships between nurses and dialysis technician’s knowledge of the evidence-based guidelines and demographic variables such as age, gender, years of experience, level of education, infection control training.
The quantitative data coded, entered, and analyzed using the IBM SPSS Statistics for Windows and Lumen Ex Machina (LEM) Software. The results were compared for reliability and internal consistency. Kuder-Richardson formula 20 (KR20) was used to measure the reliability of a test in which each question only has two answers: right or wrong [13] (“Kuder-Richardson Formula 20 (Definition & Example) - Stat ology”) (“Kuder-Richardson Formula 20 (Definition & Example) - Statology”) The KR20 formula is expressed using the number of items on the test (n), the variance of the total test scores (s2) and the proportion of persons getting the z-th item correct (pi). The product of p and q is computed for each item and summed over all (n) items (Kuder-Richardson Formula, 2024). (“Kuder-Richardson Formula - iEduNote”) (“Kuder- Richardson Formula - iEduNote”)
Applying the KR-20 shows the following for each item: KR-20 is
[n/n−1]∗[1−(Σ p∗q)/Var]
n = sample size for the test
Var = variance for the test
p = proportion of people passing the item
q = proportion of people failing the item
Σ = sum up.
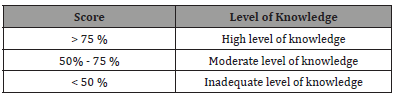
Multiply each question’s p by q, and then add them all up. (“Kuder-Richardson 20 (KR-20) & 21 (KR-21) - Statistics How To”) (“Kuder-Richardson 20 (KR-20) & 21 (KR-21) - Statistics How To”) So, there are twenty items, multiply p*q ten times, then add those items up to get a total. Each correct answer carried one score; the total score was twenty. The level of knowledge score converted into a percentage, and overall adequacy of knowledge graded according to the following criteria below.
Table 2:
The codebook named and defined each variable in the collected data. Variable gender was categorized and assigned them with numerical labels. See below the results of the participant’s demographic.
Table 3:
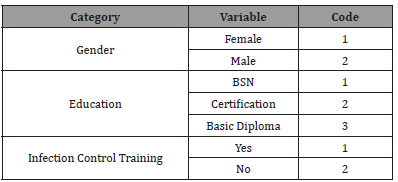
Table 1 shows the reliability results of the questionnaires designed by the researcher. As mentioned, there are twenty items only. The Cronbach’s alpha is only 0.277 while the acceptable is above 0.7). This result shows that the items are not acceptable. Table 2 shows the scale of the descriptive statistics for the pretest questionnaire/result and the items scored in percentage and the number of participants who selected the correct answer and those who picked the wrong answer. As for the item-total statistics, Table 3 shows there are items that are negatively correlated such as Q10, Q13, Q14, Q15, Q16, Q17. When those items are removed, there is a slight improvement in the Cronbach’s alpha result (see Table 4) and the total item correlation improved as well as shown in Table 5. Table 6 shows the percentage rate of each item answered by the participants. The correct answer is highlighted in yellow. Table 7 shows the result in percentage per item and the number of participants who made a mistake and who got it right. The Table shows the items that are true or false questions and the multiple choices question.
Table 4:Reliability of the Questionnaires.
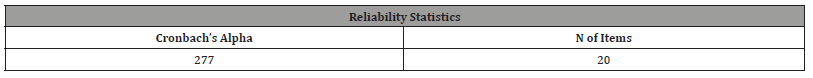
Table 5:Descriptive Statistics for the Pretest Questionnaires.
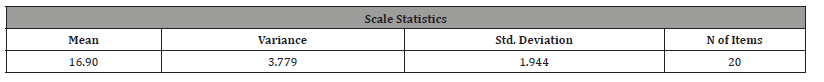
Table 6:Items that are negatively correlated.
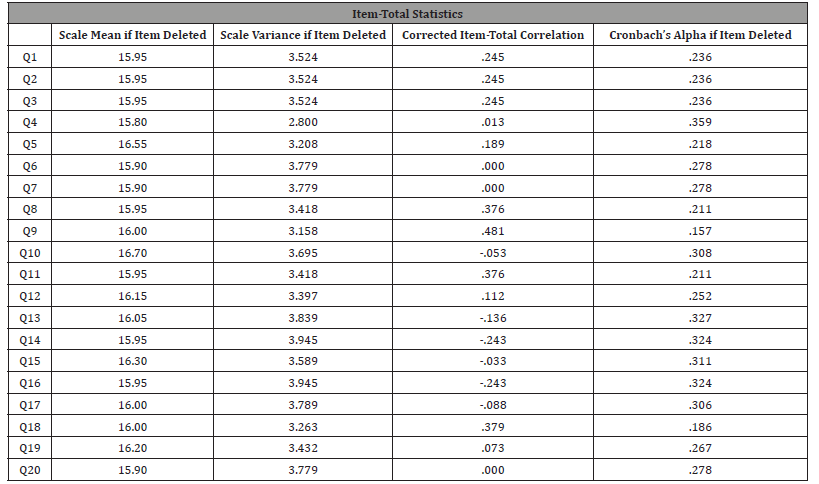
Table 7:Improvement in the Cronbach’s alpha result.
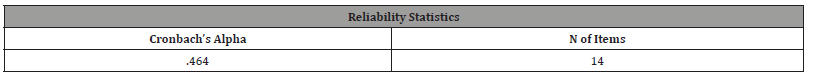
Table 8:Improved Total Item Correlation.
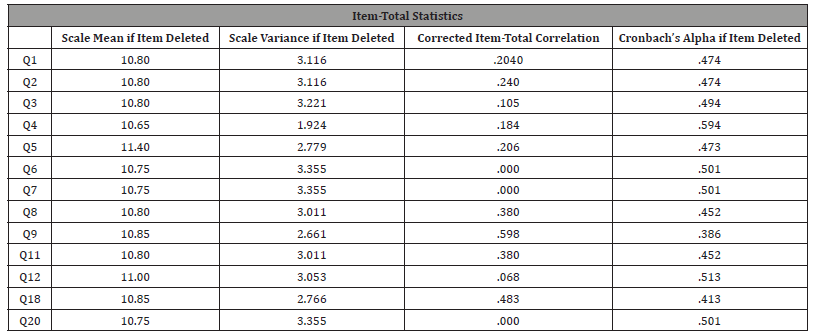
Table 9:Percentage Rate of Each Item.
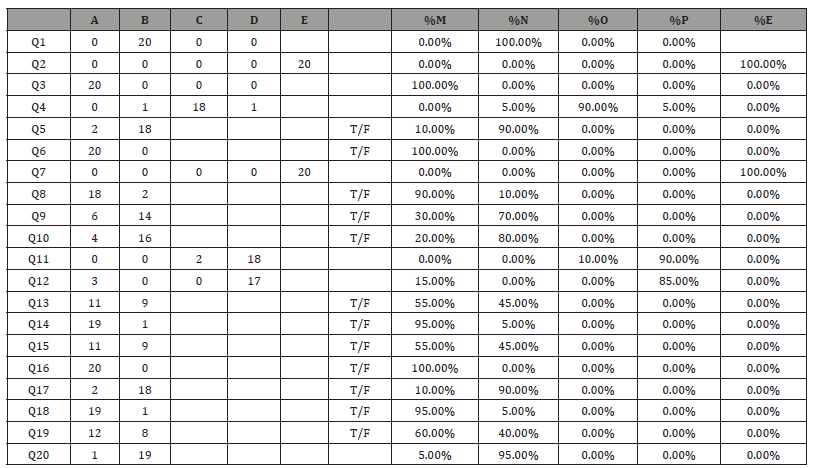
Table 10:Result (%) per Item and Participants Response.
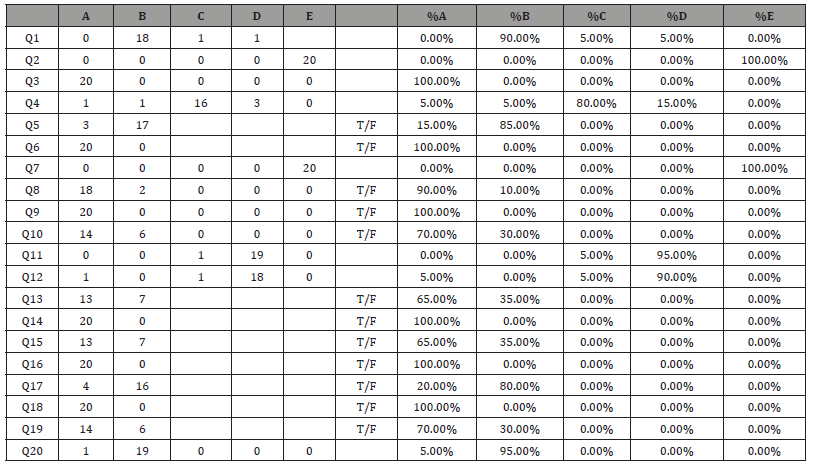
The correct answer for each item is shown with yellow highlighted. Table 8 showed the distribution of percentage scores for each multiple-choice question. The question revealed a substantial knowledge deficit of catheter care maintenance in this study population. The low score obtained in multiple-choice questions recognized the knowledge deficit of the participants. There were twelve true or false statements; the participants selected the letter that they believed was the correct answer for each item. Table 9 showed the breakdown of the percentage of correct scores for each of the individual twelve items in the test. The analysis revealed that two of the twelve items received a lower percentage answer rate of 65%. The ten items were a correct percentage score of 70 % and above. These questions revealed a higher level of knowledge concerning catheter care maintenance in the study population. All the items in the questionnaire scored one if the answer was right and zero if the answer was wrong or missed.
Table 11:Percentage of Correctly Answered Items for Multiple Questions.
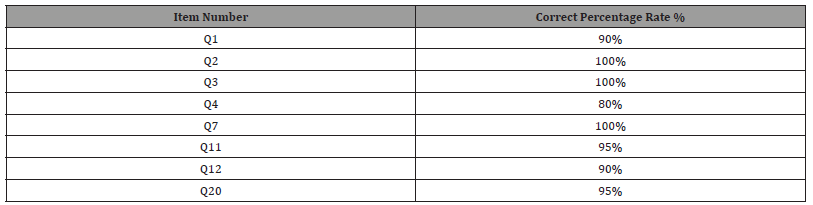
Table 12:Percentage of Correctly Answered Items on True/False Questions.
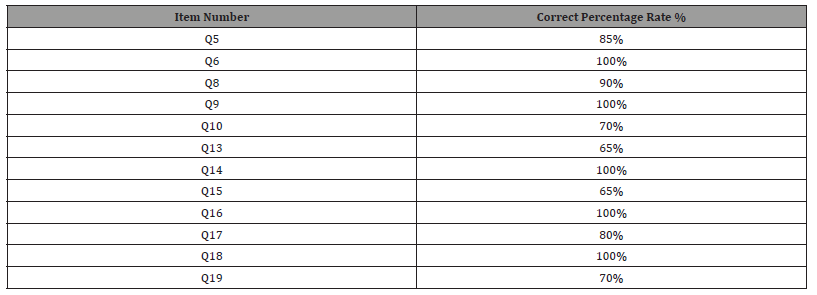
Table 10 shows the reliability analysis of the posttest. The post test result showed an improvement as compared to the pretest result. After the educational intervention, it showed an improvement in the Cronbach’s alpha. From .277 pretest result to .387 post test result. In the posttest, there is one item (Q15) that is removed as shown in Table 11 and the result revealed an improvement as well as shown in Table 12. As a comparison, the data is run through the LEM Software Program. It is a general system for the analysis of nominal, ordinal and interval levels, categorical data. I prefer to use the LEM program since it best fits the knowledge-based questionnaire reliability and internal consistency. The twenty questions are multiple choice and categorized as dichotomous and closed-ended. It also includes true or false questions that are considered as short answers, open-ended. It is dichotomous because the items have only two possibilities – correct or wrong. Close-ended are items that require the participants to pick from finite choices.
Table 13 shows the test specifics and central tendency of scores of the pretest. See Table 14 that shows the reliability measurement showing the KR-20 results. All dichotomous items are reliable (0.9 result) and the Cronbach’s alpha reveals that all items are not reliable with 0.4773 result. The analysis of each item question is shown in Table 15. There are 14 easy questions (n=70%), 5 average (n=25%) and only 1 hard item (n=5%). It revealed that the average discrimination is positive, which means that those participants who got the test item correct also had a high overall test score. The target population of the study was the staff members who are fulltime in the hemodialysis unit. The participants were (pretest N= 20, posttest N=20). As displayed in the Table 16, from the population surveyed, 50% were women, 50% were men. The participants were asked to specify their age. The reported ages were 33 and above. The level of education of the participants showed that the most predominant level of education for the nurses was Bachelor of Science in Nursing (n=40%). For the dialysis technicians, basic diploma such as High School (n= 30%) and other qualification like certification and associate degree (n= 30%).
Table 13:Improvement in the Cronbach’s Alpha.
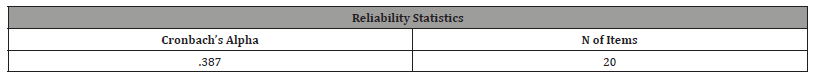
Table 14:Item Removed.
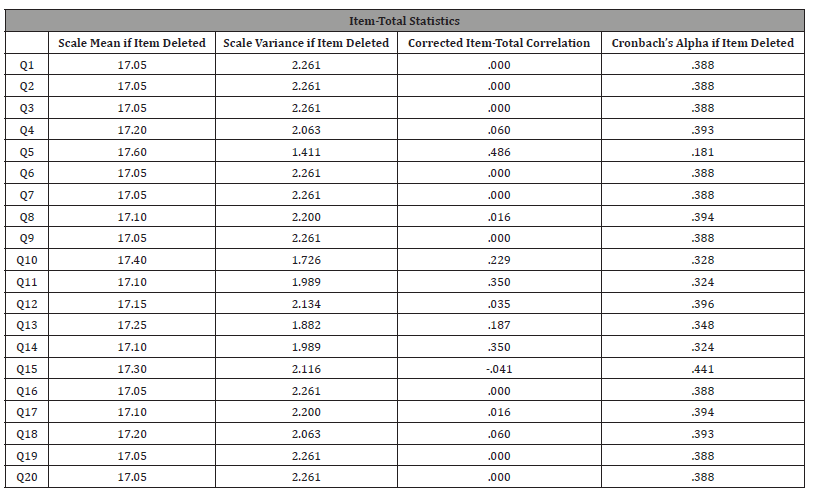
Table 15:Reliability Result.
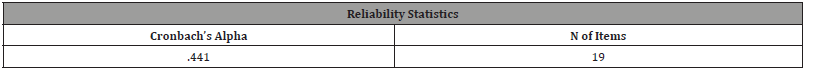
Table 16:Test Specific and Central Tendency Scores of Pre-tests.
Table 17:Reliability Measurements.
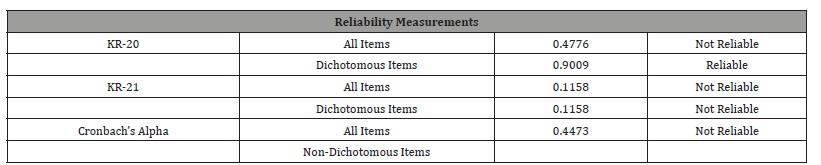
Table 18:Item Analysis of Each Question.
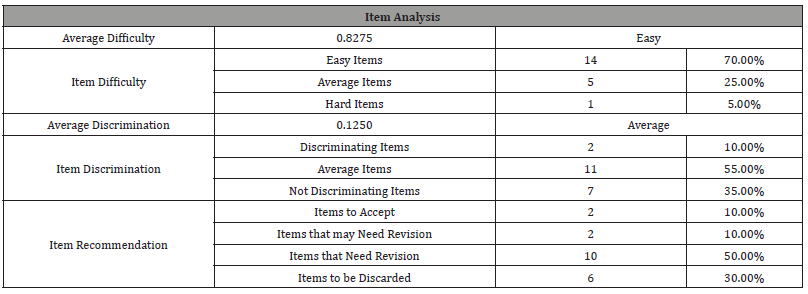
Table 19:Target Population.
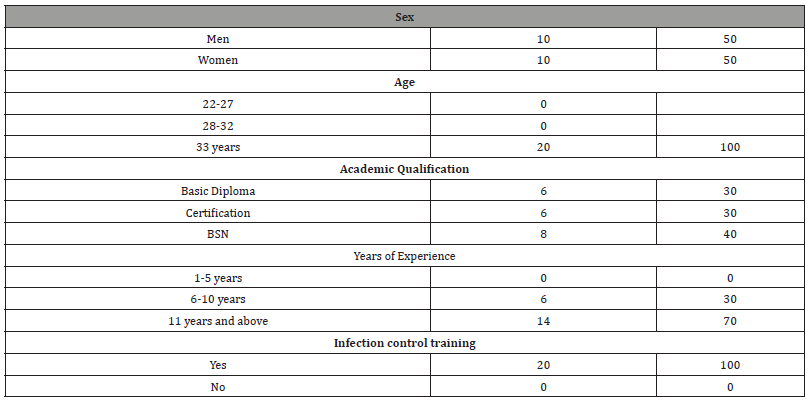
Table 20:Participants Group Pretest.
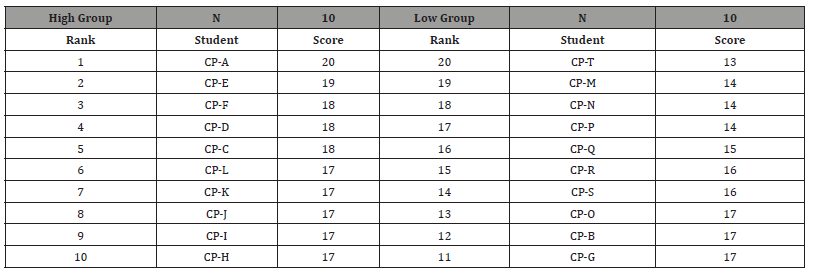
Table 21:Central Tendency of Scores.
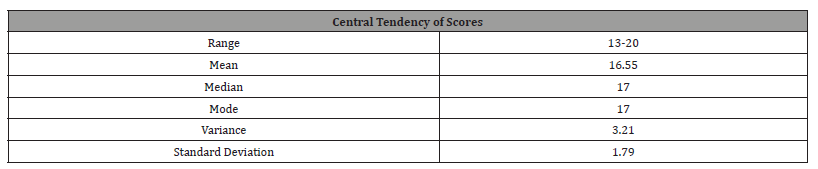
The participants were also asked to write down how many years of hemodialysis experience they had. Table 19 explained that a generous part of the participants, 70% had more than 11 years of dialysis experience and 30 % had six to ten years of experience. This was a significant description of the participants, and it showed that they are experienced dialysis staff. The dialysis unit normally conducts infection control training annually to prepare the staff and engage them in preventing and monitoring the spread of infection. The training covered the current practice and strategies based on the knowledge of the chain of infection, standard precautions, transmission-based precautions, and work practice control supported by clinical practice guidelines (handwashing, personal protective equipment uses and systemic use of antibiotics). Using the LEM program, Table 16 below revealed the high and low group of participants based on the total score of the pretest. The pretest scores ranged from 13 to 20. Table 17 shows the central tendency of scores.
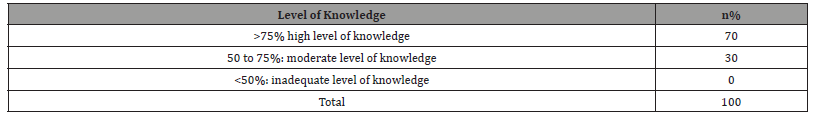
The participant’s knowledge level on the pretest revealed that 60% rated their knowledge as high level with 40% as a moderate level of knowledge (Table 18). None of the participants rated an inadequate level of knowledge. After educating the dialysis staff about catheter maintenance care, a posttest was given to the participants. As predicted, the educational intervention provided improved the knowledge level of the participants on the evidencebased practice and strategies for catheter care maintenance. The posttest scores markedly improved (Table 19). Although the scores of the pretest were already satisfactory, the posttest score showed a high satisfactory where the missed questions/items by the participants were addressed or corrected. The Table below shows the high and low group of participants based on their post test scores. The posttest scores ranged from 15 to 20. Table 20 shows the central tendency of scores. Post test results revealed an improvement. The participants’ knowledge level as shown in Table 21, the post test is 70% high level of knowledge and 30% moderate level of knowledge (Table 22).
Table 22:Level of Knowledge Result of Pretest.
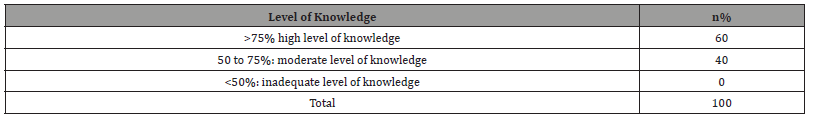
Table 23:Post Test Group of Participants.
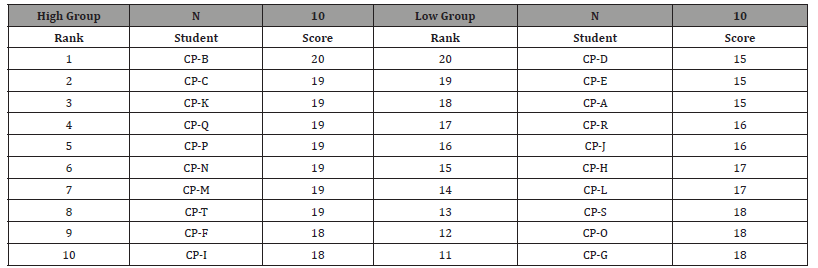
Table 24:Central Tendency of Scores.
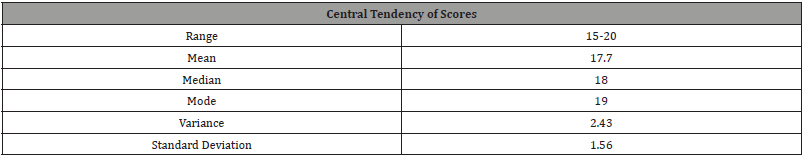
Table 25:Level of Knowledge Result of Post Test.
Discussion
Failure of staff members to complete the competency checklist due to poor knowledge and skills is an indicator to reinforce the educational intervention needed to achieve the best outcome. As mentioned, the educational intervention includes the review of the unit policy and procedures on catheter initiation, maintenance, and termination with hemodialysis catheter. Evidence based practices such as hand hygiene, Chlorhexidine, dressing changes, hub/ clave care, line necessity and daily review of line assessment were also enforced. Also, a competency checklist (Center for Disease Control and Prevention, 2017) [14] which is an essential element in assessing the knowledge and skills of the dialysis staff members was completed. Adherence to the core intervention protocol recommended by CDC is a safety process. Dialysis centers must continue to implement guidelines to reduce morbidity, mortality, and cost of the healthcare system. Sufficient knowledge and skills are important to ensure safety and promote efficient and effective quality patient outcomes. The systematic review helped to check and find relevant studies related to the prevention and control of CRBSI. Evidence from the systematic review suggests that there are infection control measures and core interventions that influence control and prevention of catheter infection. All the studies reviewed were graded as strong recommendations and were used to support the evidence-based clinical practice guidelines. The recommendations focus on adherence, practices, control, prevention, and education.
Adherence
Adherence to infection prevention and control practice is highly essential to provide safe and high-quality patient care. Particularly is the core set of infection prevention and control practices that are needed in healthcare settings. The core practices are intended to serve as a standard reference and reduce the need to evaluate practices that are considered basic and accepted as standards of medical care. (“Safe Care Campaign | Welcome”) (“Safe Care Campaign | Welcome”) The core practices and intervention include standard precaution (hand hygiene, use of personal protective equipment (PPE), environmental cleaning and disinfection, education, and training of healthcare personnel on infection prevention (Centers for Disease Control and Prevention [CDC], 2022). Milson, et.al (2019) [15] study, adherence to infection control standards improved when the ESRD Safety program was implemented. Audits improved 27%-82% of procedures performed correctly. CRBSI decreased from 2.33-1.07 events per one hundred patients per month.
Practices
Completion of audit tools and checklist suggested by the CDC guidelines and practices is recommended to reduce the CRBSI. The dialysis staff can use the audit tools and checklist to help guide their practices (see appendix A). Such audit tools (catheter care tools) are catheter connection and disconnection, catheter exit site care and hand hygiene observation. The checklist is designed to help staff in following those practices. The leadership team can use these resources to monitor and establish a set standard of practice in the dialysis unit. The following suggested tools and checklist ensures dialysis staff adherence to infection control practices. In addition, a return demonstration of catheter care using the chest mannequin (see appendix G) with CHG impregnated dressing and following the unit policy and procedure in initiation, care and maintenance were done by the participants.
Control and Prevention
In the presence of active infection and control and prevention, the use of systemic antibiotic therapy such as Vancomycin and Gentamycin are highly effective for the reduction of morbidity and mortality. The antibiotic protocol was free of side effects. The study also revealed that the antibiotic-heparin /citrate locks for the prevention of gram-positive CVC related bacteremia have shown encouraging results; none of the sixty patients receiving vancomycin- heparin lock developed CRBSI over an average of 10 days of observation period (Carratala et al., 2009). Also, the study also revealed that patients receiving emergency -only HD via TCC have a high CRBSI rate compared with infection rates previously reported in patients receiving scheduled maintenance HD. The study also considers another way which is to transition patients to arteriovenous or grafts for HD access or with antimicrobial lock therapy which prevents catheter infection receiving scheduled HD. Thus, increased CRBSI risk contributes to the increased morbidity and mortality in ESRD patients receiving emergency-only HD [16].
The use of Bio Patch is also recommended. Studies have shown that it is the only dressing proven to reduce the rate of CRBSI. (“Use of Bio Patch® (Protective Disk with Chlorhexidine Gluconate) in Closed-Suction Drainage for Penile Implant Surgery”) (“Use of BioPatch® (Protective Disk with Chlorhexidine Gluconate) in Closed-Suction Drainage for Penile Implant Surgery”) A randomized controlled study of 1,699 central venous or arterial catheter sites showed a 44% reduction in the incidence of local infections. This is a statistically significant reduction, as is the reported 60% reduction in the incidence of CRBSI (Khurgin & Garber, 2014, p. 192). Bio patch™ is also useful in reducing local exit site infections in patients who have tunneled, cuffed catheters [17]. Another evidence-based guideline is chlorhexidine use as skin antisepsis. Optimization of skin antisepsis is essential to prevent short-term catheter related infection. Chlorhexidine-alcohol was associated with lower incidence of catheter-related infections (0·28 vs 1·77 per 1000 catheter-days with povidone iodine-alcohol; hazard ratio 0·15, 95% CI 0·05-0·41; p=0·0002). For skin antisepsis, chlorhexidine-alcohol provides greater protection against shortterm catheter-related infections than does povidone iodine-alcohol (Mimoz et al., 2015, p. 2069).
Education
An educational intervention significantly increased the dialysis staff knowledge on the care of the patient with central venous catheters (tunneled or non-tunneled). It improved patient outcomes. Staff were responsible for applying their knowledge to reduce infection episodes. Non-adherence to recommended evidencebased guidelines for preventing CRBSI could be due to inadequate knowledge of the guideline. An educational intervention provided such as in-services or training may lead to a decrease incidence of CRBSI and may also result in a remarkable reduction in the cost of medical treatment and patient morbidity when implemented on a mandatory basis (Warren et al., 2004). The analysis showed a good improvement in the dialysis of staff knowledge before and after the educational intervention. The positive response of the staff by engaging in the study reflected that education could create a change in knowledge level. As expected, the educational intervention helped the staff members to improve their knowledge level on evidence-based guidelines for HD catheter care. The auditing tools such as competency and checklist were good and helpful resources to know the performance level of the participants. Such tools are aligned with Core Interventions and allow for more observations or monitoring to be performed. The procedural checklist was used to teach and guide the practice of the dialysis staff members [13]. A new catheter kit was presented to the staff and demonstration of the use of the new kit with adherence to the unit policy on catheter initiation, care, and maintenance. After educating the staff with the new catheter kit, the staff was asked to do a return demonstration of catheter care using the chest mannequin and the new kit. The staff were able to show the step-by-step process of catheter care based on the unit policy and procedure.
Conclusion
The increase rate of catheter infection dialysis patients is a safety leading concern in End Stage Renal Disease (ESRD) population. It has become a critical issue in the dialysis center. These health care concerns extend to critically ill patients who use CVC for IV fluids, blood products and hemodynamic monitoring. The inability to meet the quality and safety standards becomes a systemic situation. Thus, the control and prevention of CBRSI is considered significant. This project was vital to the dialysis team, patients, and families. The dialysis staff are frontliners that require sufficient knowledge. They play a huge role in saving lives, promoting safety and quality of care. The participants in this project can be a valuable resource and example for other dialysis staff members, particularly the newly hired staff. It is important to assess the ability of the dialysis staff members to create positive changes in the practice. The audit and checklist tools are used monthly as a competency assessment and training to address adherence and compliance of the dialysis staff. It was expected that the dialysis staff awareness and the learning from the project ensures that the knowledge was practical to help patients. The leadership should encourage a therapeutic learning environment.
The study focuses on social change contribution by looking for an educational intervention that helped the dialysis staff knowledge improvement to promote patient safety and reducing infectious complications. When the dialysis staff were empowered to share their experiences and insights they learned from the study, they could advocate for patients professionally and can serve as a motivating force in the policy-making process. It is a wonderful opportunity to create a quality improvement project. The content of the educational intervention was appropriate to address the risk for CRBSI and promote evidence-based practice and strategies. Participants of this study will serve as resource people, for example, and a preceptor for other dialysis personnel. The study also has relevance for the training and ensuring the skills and competency of the staff in the dialysis center. The application of the learnings from the educational intervention would significantly contribute to the body of nursing knowledge. Implementing the evidence-based practices and strategies contributes to the improvement of the participants’ knowledge and provides positive outcome to patients and physicians as well.
Therefore, the study could proactively help and become a profound influence on the dialysis staff and even nurses working in a critical care unit to effect the needed changes to strengthen and provide quality and safe patient care. The very satisfactory result of the post-test and excellent cooperation from the participants was remarkable. The success of the educational intervention was noted in the compliance of the participants in following evidence-based practice and strategies. The review of the unit policy, skill checklist, competency training and adherence to infection control standards and practices (PPE, hand hygiene, catheter care maintenance) were perceived and absorbed by the participants without any issues or difficulty. The questionnaires were not difficult to explain to the participants and they were able to answer it with honesty and with no use of resources/references related to the educational intervention. Another strength of the study was that the information shared and obtained through the survey provided valuable information and guidance to develop the clinical practice guidelines based on evidence-based practices and strategies recommended by CDC, CMS & Renal Network.
Overall, the findings of the study showed a moderate & satisfactory knowledge of the dialysis staff in UIC dialysis center. The results revealed that the pretest and posttest score improved after an educational intervention. The most major areas which showed noteworthy knowledge deficit are hand hygiene after catheter care, use of Tegaderm and the actions used to reduce CBRSIs such as the correct way and time to change transparent dressings. Educational intervention through huddles, webinars and return demonstration addressed the issues and concerns. Return demonstration and huddles addressing valuable information related to catheter care and maintenance using CPGs and EBPs was one of the efficient methodologies of promoting and improving the knowledge of dialysis staff. Infection control surveillance and monitoring the CRBSI rates should be included in the quality assurance/ quality initiative of the dialysis center to ensure patient safety and quality of care. Adherence to unit policy and completing competency, skill checklist and constant education helps control and prevent catheter related infection.
Acknowledgement
This article and the research behind it became possible with the support of my Committee Chairpersons: Dr. Linda Samson, Dr. Anthony Bucki & Dr. Patricia Martin. Their guidance, enthusiasm, expertise and honest feedback to details have been an inspiration and kept my work focused from conceptualizing, data collection and gathering, plan execution. They generously give their time to better my dissertation. I am also grateful for the support of Dr. Claudia Lora, Medical Director of UIC Dialysis Center for her excellent cooperation and commitment in getting started this study in UIC Dialysis Center. With the support of the dialysis staff, this project would not have been completed. Their participation and their excellent contribution foster a huge encouragement to put my sincerest commitment. Lastly, to my family (loving husband and two beautiful children), friends and colleagues for their full support and trust that I will successfully finish this study.
Conflict of Interest
I certify that I have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Appendices
Appendix A
Questionnaires: Pretest-Posttest for Catheter-related bloodstream infection prevention.
Instruction:
a) Please do not sign your name.
b) Each correct answer corresponds to one grade.
c) Your answer will store with a high degree of security.
Circle the correct answer to the following questions.
1. What is the best site for a central vascular catheter?
a. Femoral
b. Subclavian
c. Internal jugular
d. None of the above
2. Infections associated with the use of CVC has an elevated risk of
a. Mortality
b. Morbidity
c. Hospital length of stay
d. Costs
e. All the above
3. The antimicrobial ointment should be applied to the exit site of dialysis catheters because it does help decrease the incidence of
CRBIs.
a. True
b. False
4. In the insertion of CVC, the insertion site is oozing. You should
a. Apply a transparent dressing.
b. Apply gauze dressing.
c. Apply both gauze and a transparent dressing.
d. Wait until the site has stopped oozing then apply any dressing.
5. There is no need to wash or gel hands if you wear clean gloves when checking the exit site or changing the dressing of a central
venous catheter.
a. True
b. False
6. The use of chlorhexidine as a skin preparation (as opposed to Povidone-iodine) is associated with decreased CRBSs rates in
studies.
a. True
b. False
7. Which actions will decrease the risk of CRBIs?
a. Use of antimicrobial ointment
b. Use of bio patch protector
c. Use of catheter kits provided by the unit/organization.
d. Use of mask, gloves during catheter care
e. All the above
8. If a catheter culture comes back positive, but the blood sample cultures are negative, evaluate the entire picture. Reassess the
patient before giving antibiotics.
a. True
b. False
9. The catheter port/hub should be scrubbed 10-15 seconds every time the accessed is accessed during treatment.
a. True
b. False
10. If the dressing is loose, you should reinforce it with a tape until the next schedule dressing change.
a. True
b. False
11. John Doe has an unexplained fever and chill, and you suspect a blood stream infection. When you inspect his catheter site, there
is erythema and a small amount of yellowish discharge. What should you do?
a. Consider removing the catheter and replacing it with a guidewire exchange and assess the need for antibiotics.
b. Consider removing the catheter and place another on a new site and assess the need for antibiotics.
c. Collect a blood culture and swab the exit site.
d. All above
12. If you suspect a blood stream infection, two sets of blood samples should be drawn for culture. The proper sites to culture are:
a. One from catheter hub/port, the other from peripheral source
b. Two different peripheral sources
c. From a catheter hub, for 15 mins. Apart of collection
d. Either a or c
13. The proper way to draw culture blood from a suspected source is to draw 20cc and place 10 cc in each of two bottles.
a. True
b. False
14. The two common sources of CVC infections are from patient’s skin flora and healthcare providers hands.
a. True
b. False
15. Transparent dressings should be changed every 48 hours.
a. True
b. False
16. Mask should be worn for all CVC dressing changes and before the dressing is removed.
a. True
b. False
17. Bio patch is changed every 24 hours.
a. True
b. False
18. CVC infections are preventable by ensuring proper insertion techniques, proper maintenance and care and removing the catheter
if no longer needed.
a. True
b. False
19. When applying antiseptic to exit site, using mild friction in a circular motion wiping away from the exit site to the surrounding
skin area for thirty second, then dry the skin using a clean gauze.
a. True
b. False
20. Scrub the catheter hub one at a time using an approved antiseptic pad for each hub for _______ seconds. Scrub the end and sides
of each hub with friction, ensuring that all debris is removed.
a. 5 seconds
b. 10-15 seconds
c. 20 seconds
d. 60 seconds
Appendix B
Appendix C
Appendix D
Appendix E
Appendix F

Appendix G

References
- Muthukumar V, Arumugam PK, Bamal R (2020) Role of systemic antibiotic prophylaxis in acute burns: A retrospective analysis from a tertiary care center. Burns: journal of the International Society for Burn Injuries 46(5): 1060-1065.
- Temiz A, Ayşe Albayrak, Rıfat Peksöz, Esra Dışcı, Ercan Korkut, et al. (2020) Factors affecting the mortality at patients with burns: Single center results. Turkish 26(5): 777-783.
- Ashouri S (2022) An Introduction to Burns. Physical Medicine and Rehabilitation clinics of North America 33(4): 871-883.
- Ozlu B, Basaran A (2022) Infections in Patients with Major Burns: A Retrospective Study of a Burn Intensive Care Unit. Journal of Burn Care & Research 43(4): 926-930.
- Arturson G (1980) Pathophysiology of the burn wound. Ann Chir Gynaecol 69(5): 178-190.
- Sharma BR (2007) Infection in patients with severe burns: causes and prevention thereof. Infectious disease clinics of North America 21(3): 745-759.
- Ramos G, Cornistein W, Torres Cerino G, Nacif G (2017) Systemic antimicrobial prophylaxis in burn patients: systematic review. Journal of Hospital Infection 97(2): 105-114.
- Church D, Elsayed S, Reid O, Winston B, Lindsay R (2006) Burn wound infections. Clinical Microbiology Reviews 19(2): 403 -434.
- Millan LS, et al. (2012) Bloodstream infection by multidrug-resistant bacteria in patients in an intensive care unit for treatment of burns: a 4-year experience. Revista Brasileira de Cirurgia Plástica 27(3): 374-378.
- Critical Appraisal Skills Programme (CASP) (2013) CASP Checklist (Online). Oxford.
- Harbour R, Miller J (2001) A new system for grading recommendations in evidence-based guidelines. British Medical Journal 323(7308): 334-336.
- Yeong E, Wang-Huei Sheng, Po-Ren Hsueh, Szu-Min Hsieh, Hui-Fu Huang, et al. (2020) The Wound Microbiology and the Outcomes of the Systemic Antibiotic Prophylaxis in a Mass Burn Casualty Incident. Journal of Burn Care & Research 41(1): 95-103.
- World Medical Association (2013) World Medical Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310(20): 2191-2194.
- Durtschi M, Orgain C, Counts G, Heimbach D (1982) A prospective study of prophylaxis penicillin in acutely burned hospitalized patients. The Journal of Trauma 22(1): 11-4.
- Timmons M (1983) Are systematic prophylactic antibiotics necessary for burns?. The Annals of the Royal College of Surgeons of England 65(80-82).
- Alexander J, Macmillan B, Law E, Kern R (1984) Lack of beneficial effects of restricted prophylactic antibiotics for debridement and/or grafting of seriously burned patients. Bulletin and Clinical Review of Burn Injuries 1: 20.
- Piel P, Scarnati S, Goldfarb IW, Slater H (1985) Antibiotic prophylaxis in patients undergoing burn wound excision. The Journal of Burn Care & Rehabilitation 6(5): 422-424.
- Griswold J, Grube B, Engrav L, Marvin J, Heimbach D (1989) Determinants of donor site infections in small burn grafts. The Journal of Burn Care & Rehabilitation 10(6): 531-535.
- Munster A, Xiao G, Guo Y, Wong L, Winchurch R (1989) Control of endotoxemia in burn patients by use of polymyxin B. The Journal of Burn Care & Rehabilitation 10(4): 327-330.
- Deutsch D, Miller S, Finley R (1990) The use of intestinal antibiotics to delay or prevent infections in patients with burns. The Journal of Burn Care & Rehabilitation 11(5): 436-442.
- Steer J, R P Papini, A P Wilson, D A McGrouther, L S Nakhla, et al. (1997) Randomized placebo-controlled trial of teicoplanin in the antibiotic prophylaxis of infection following manipulation of burn wounds. British Journal of Surgery 84(6): 848-853.
- Rodgers G, Fisher M, Lo O, Creswell A, Long S (1997) Study of antibiotic prophylaxis during burn wound debridement in children. The Journal of Burn Care & Rehabilitation 18(4): 342-346.
- Kimura A, T Mochizuki, K Nishizawa, K Mashiko, Y Yamamoto, et al. (1988) Trimethoprim-sulfamethoxazole for the prevention of methicillin-resistant Staphylococcus aureus pneumonia in severely burned patients. Journal of Trauma 45(2): 383-387.
- Sheridan R, Weber J, Pasternack M, Tompkins R (2001) Antibiotic pro-phylaxis for group A streptococcal burn wound infection is not necessary. The Journal of Trauma 51(2): 352-355.
- Ergün O, Celik A, Ergün G, Ozok G (2004) Prophylactic antibiotic use in pediatric burn units. European Journal of Pediatric Surgery 14: 422-426.
- Ugburo A, Atoyebi O, Oyeneyin J, Sowemimo G (2004) An evaluation of the role of systemic antibiotic prophylaxis in the control of burn wound infection at the Lagos University Teaching Hosptial. Burns 30(1): 43-48.
- De La Cal M, Enrique Cerdá, Paloma García-Hierro, Hendrick K F van Saene, Dulce Gómez-Santos, et al. (2005) Survival benefit in critically ill burned patients receiving selective decontamination of the digestive tract: a randomized, placebo-controlled, double-blind trial. Annals of Surgery 241(3): 424-430.
- Lyons J, Christopher Davis, Mary T Rieman, Robert Kopcha, Ho Phan, et al., (2006) Prophylactic intraveneous immune globulin and polymyxin B decrease the incidence of episodes and hospital length of stay in severely burned children. Journal of Burn Care & Research 27(6): 813-818.
- Ramos G, Marcela Resta, Enrique Machare Delgado, Ricardo Durlach, Liliana Fernandez Canigia, et al. (2008) Systemic perioperative antibiotic prophylaxis may improve skin autograft survival in patients with acute burns. Journal of Burn Care & Research 29(6): 917-923.
- Chahed J, et al. (2014) Burns injury in children: is antibiotic prophylaxis recommended?. African Journal of Paediatric Surgery 11(4): 323-325.
- Mulgrew S, Khoo A, Cartwright R, Reynolds N (2014) Morbidity in pediatric burns, toxic shock syndrome, and antibiotic prophylaxis: a retrospective comparative study. Annals of Plastic Surgery 72(1): 34-37.
- Tagami T, Matsui H, Fushimi K, Yasunaga H (2016) Prophylactic antibiotics may improve outcome in patients with severe burns requiring mechanical ventilation: propensity score analysis of Japanese nationwide database. Clinical Infectious Diseases: an official publication of the Infectious Diseases Society of America 62(1): 60-66.
- Sherry N L, Padiglione A A, Spelman W, Cleland H (2013) Microbiology of wildfire victims differs significantly from routine burns patients: data from an Australian wildfire disaster. Burns 39(2): 331-334.
-
Myrna Tayco-Manuel*. Evidence-Based Practice & Strategies in Reducing Catheter Blood Stream Infection in Hemodialysis Patients. Annals of Urology & Nephrology. 5(1): 2024. AUN.MS.ID.000601.
-
Catheter blood stream infection (CRBSI); hemodialysis (HD); central venous catheter (CVC); end stage renal disease (ESRD); personnel protective equipment (PPE); Center for Disease Control (CDC); evidence-based practice (EBP); iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






