 Research Article
Research Article
Enuresis of Children in A Hospital Environment: Epidemiological, Diagnostic and Therapeutic Aspects in The Thies Region
Kouka SCN1*, Sissokho M2, Thiam NM2, Jalloh M2, Diop M3, Faye M3, Diame A1, Diallo Y1 and Sylla C2
1Department of Urology, Faculty of Health Sciences, University Iba Der Thiam of Thies, Senegal.
2Department of urology, Mbour hospital, Senegal.
3Department of Urology, University Cheikh Anta Diop De Dakar, Senegal.
Saint Charles Nabab Kokua, Department of Urology, Faculty of Health Sciences, University Iba Der Thiam of Thies, Senegal
Received Date:December 20, 2023; Published Date:January 03, 2024
Abstract
Introduction:Enuresis is a functional abnormality of urination. Its management requires a simple but rigorous clinical assessment and
treatment adapted to each child.
Objectives:To study the epidemiological, clinical, and therapeutic characteristics of enuretic patients consulting in a hospital environment in
the Thies region.
Patients and Methods:We conducted a prospective descriptive study from January 1st, 2019, to October 31st, 2019. We included all cases of
enuresis in the urology departments of the regional hospital of Thies, the Hospital of Tivaouane and the Diamniadio children’s hospital.
Results:We recorded 30 cases of enuresis during the study period. The prevalence of enuresis was 3.71% with a sex ratio of 1.5 in favor of boys.
The average age of the children was 9.63 ± 2.4 years. It was primary enuresis in 86.66%. and secondary in 13.33%. In 86.66% of cases, enuresis was
nocturnal and isolated. Enuretic episodes occurred in 56.66% of cases 2 to 3 times per week. The urological examination was normal in 97% (n=29).
The behavioral treatment associated with the medical treatment resulted in a cure rate of 69% after a 6-month follow-up.
Conclusion:Nocturnal enuresis is common in our regions. A cure can be obtained with comprehensive management by a well-trained medical
staff.
Keywords:Nocturnal enuresis; child; treatment
Introduction
Enuresis is a functional abnormality of urination [1]. It is defined by the existence of nocturnal and sometimes daytime urination that is involuntary and unconscious, persisting or reappearing after the average age of acquisition of sphincter control, but not resulting from an organic cause [2]. Usually, enuresis is considered from the age of 5 years, when urination control is most often acquired. Enuresis is called Primary Enuresis if the child has never had a period of continence during sleep for at least six months [3]. The resumption of incontinence during sleep after six months of voiding control is secondary enuresis [4]. The true incidence of enuresis is currently unknown in Senegal [5]. Its management requires a simple but rigorous clinical assessment and treatment adapted to each child. The aim of this work was to determine the epidemiological, clinical and therapeutic characteristics of enuretic patients consulting in a hospital environment.
Patients and Methods
This is a prospective, descriptive study carried out between
January 2019 and October 31, 2019, in the Pediatrics department
of the Diamniadio children’s hospital and the urology departments
of Thiès and of Tivaouane hospitals. It concerned all children
of both sexes, aged at least 6 years, referred by their parents to
the hospital. We included 30 patients presenting with enuresis
during this period. The parameters studied were collected from a
questionnaire and concerned:
a) The identity of the patients (schooling, urban, suburban,
rural origin).
b) Epidemiological data (hospital frequency, age, sex).
c) Enuretic factors (family factor, bladder factor, hormonal
factor; sleep factor, constipation factor and psychological
factor).
d) The characteristics of enuresis: type, periodicity,
frequency.
e) assessment of the parents’ behavior regarding the
problem: indifference, abuse, humiliation, understanding.
f) Physical finding and work up.
g) Therapeutic data (restriction of drinks after 7 p.m.,
complete urination before sleep, awakening induced with the
regularity of daytime urination, medical treatment, either
Desmopressin, Oxybutynin or Clomipramine, voiding calendar).
h) The results of the treatment, the rate of follow-up (1
month, 3 months, 6 months).
i) Data entry and analysis were carried out using Word
2013, Excel 2013, and SPSS 2020.
Results
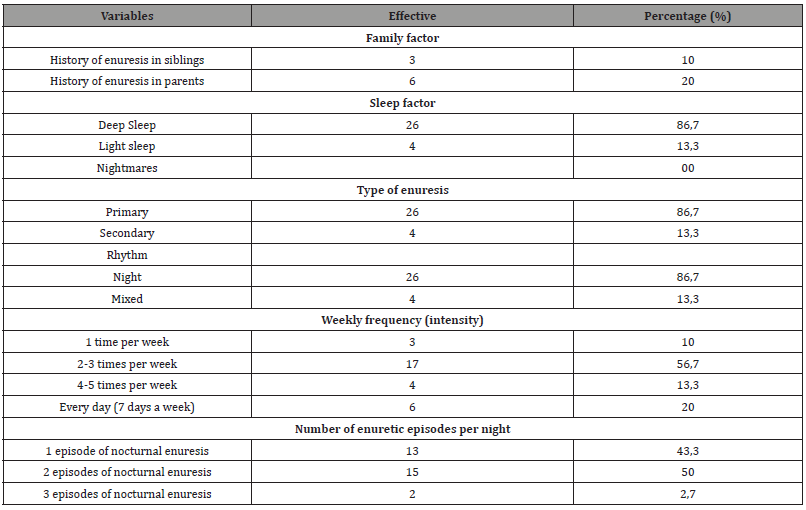
Out of a total of 808 children consulted, 30 children presented with enuresis during the study period, i.e. a prevalence of 3.71%. The average age of the children at the time of diagnosis was 9.63 +/-2.414 years with a range of 5 to 16 years. The most represented age group was 7 to 8 years old accounting for 33,33% of cases (n = 10). The sex ratio was 1.5 in favor of boys (60%). All children referred for enuresis were pupils. The majority of children lived in urban areas (66.7%) while 23.3% lived in rural areas. There was no history of diabetes, sickle cell disease or asthma. The family history of enuresis was reported in 9 patients (30%), including 10% (n=3) among siblings and 20% (n=6) among parents (Tables 1&2). No socio-family factor or other urinary symptoms was found. Enuresis was primary in 26 children (86.7%), secondary in 4 children (13.3%). The weekly frequency was 2 to 3 enuretic episodes in 17 children (56.7%), 1 episode in 3 patients (10%), 4 to 5 episodes in 4 patients (13,3%) and 7 episodes in 6 patients (20%). The enuretic episode generally occurred once per night in 13 children (43,3%), twice per night in 15 children (50%) and three times per night in 2 children (6,7%) (Figure 1).

Table 1:General characteristics.
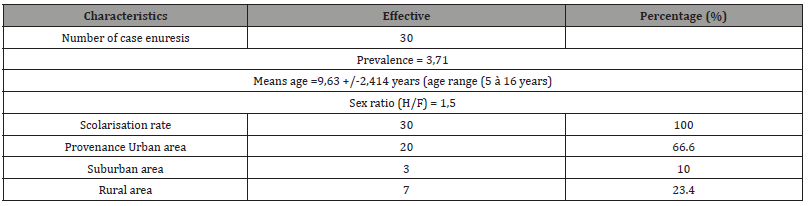
Table 2:Distribution of the patients according to risk factors and characteristics of enuresis.
Parents reported a notion of deep sleep in 86%, light sleep in 14%. No child reported nightmares during the sleep phase. The parents in our series had a passive attitude regarding the enuresis in 36.7% of cases (Table 3). On the other hand, 63.3% of parents humiliated or punished their children. However, only 6.7% of parents reassured their children about enuresis, and 30% understood the situation and accepted the symptoms as being a pathology that requires treatment (Figure 2). The urological examination found 1 case of phimosis and was normal in 29 children. Urine culture was carried out in 70% of cases and was normal in all cases. Fasting blood sugar levels were only performed in 3 patients, i.e. 10%, and were negative. All our patients received behavioral treatment for 1 month. Medical treatment was prescribed in 45% of cases: 35% of enuretic children were on Oxybutynin, 7% of patients were on Desmopressin, 3% on Clomipramine. Behavioral treatment alone resulted in a 50% cure rate (Figure 3). Relapses at medical treatment interruption or before the end of the treatment period were reported in 8% of cases.
Table 3:Distribution of the patients according to type of treatment and evolution.



Discussion
Epidemiology
In our study, the prevalence of enuresis is estimated at 3.71%. Huang [6] in China, noted a prevalence of 3.99%. Senegal found a prevalence of 1.44%. This prevalence is relatively low compared to the data reported in the literature with rates varying from 12.95% in Burkina Faso by Ouédraogo [7], 5.4% in France. Hjalmas [8] reported an estimated prevalence of 8%. This difference in prevalence could be explained by the variability of the study populations. In addition, the real incidence of enuresis remains unknown. The average age of our patients was 9.63 years. This average age is close to 8 years reported. However, Sylla reported a hiher average age of 15 years. This difference could be explained by the fact that their study focused on adolescent enuresis. In our series, we noted a higher frequency in boys (60%). This agrees with the study where the frequency of enuresis was higher in boys (9.09%) than in girls (8.03%). On the other hand, Sylla noted a higher frequency among girls with a sex ratio (M/F) of 0.85. There was no medical history found in the children in our study. Some authors like Sylla reported a medical history in their study with great variability. The notion of a family factor in enuresis exists in 30 to 60% of cases. In our study it was estimated at 30% and concerned parents in 20% of cases or siblings in a proportion of 10% of our patients. This family factor was frequently reported in literature varying from 32.35% for Sylla and 10.3 % for Chan.
Diagnosis
The diagnosis of enuresis is essentially clinical and is based on questioning the patient and/or parents and physical examination. Patient age, enuresis periodicity and frequency must be specified; quality of sleep and psychosocial impact of patients must be assessed, and a voiding calendar must be completed.
Type of enuresis
In our study, primary enuresis was common accounting for 87% of patients, compared to 13% of secondary enuresis. This corroborates the majority of authors who report a predominance of primary type enuresis varying from 77% for Sylla 78.9% for Ouédraogo. In our series, 56.7% of children had 2 to 3 episodes of enuresis per week, 20% had 7 episodes of enuresis per week (enuresis every day of the week) and 13% of patients had 4 and 5 episodes of enuresis per week. For Lachguer K [9], depending on the intensity, enuresis was severe (at least 3 episodes per week) in 88.8% of patients while in the series by Sylla enuresis was moderate in 42% of patients and with average intensity in 58% of cases.
Parental reaction
The parents in our series were passive in 36.7% of cases. On the other hand, 63.3% of parents punished their enuretic children. Sylla C found 76% punishment. In Burkina Faso, Ouédraogo found 27% of enuretic children were punished by their parents.
Physical examination
Examination of the urogenital tract was normal in 97% of children. For Lachguer K also, the physical examination was normal in 95.4% of cases of enuresis.
Workup
Urine culture and blood glucose level were normal in all cases. In the literature, urinary infection has been reported in between 3% and 16% of cases. In the work of Sylla as well as that of Lachguer blood sugar was normal in 100% of cases. These results confirm that the diagnosis of enuresis does not require additional examination as in the first instance. Imaging was not systematically performed. Maintaining a 48-hour voiding calendar is the recommended way to confirm or correct the diagnosis.
Treatment
Parents and their children sometimes need psychological support to reassure them that enuresis is a symptom that tends to disappear spontaneously with age. Management requires good information and therapeutic education (hygienic and dietary measures and keeping a voiding calendar). In our series, all our patients benefited from behavioral treatment. In enuresis associated with nocturnal polyuria and refractory to hygienic and dietary measures alone, the desmopressin is the treatment of choice [10]. In our study 7% of patients were on desmopressin, 35% on Oxybutynin and 3% on Antidepressant treatment. According to some athors, in children suspected of having low nocturnal bladder capacity, oxybutynin can be prescribed as secondline monotherapy when specific treatments have failed [11]. In our stady, 69% of our patients were cured, 23% achieved improvement and treatment failure was noted in 8% of cases.
Behavioral treatment alone resulted in a 34% cure rate, 33% improvement rate and 33% failure rate. In our study 50% of our patients treated by desmopressin responded well to the treatment in combination with the behavioral treatment. For Glazene [12], desmopressin can rapidly decrease the number of wet nights. And [13] reported that up to 70% of patients have dry nights after treatment and 50% of the “successful” patients had relapse after stopping the medication and 50% of them had an improvement. Some authors have recommended, in the treatment of enuresis with polyuria, a reduction in salt consumption or combining desmopressin in the evening and diuretics in the morning [14,15]. Other specialists may opt for individualized combination therapies including components such as the enuresis alarm, desmopressin, anticholinergics, or antidepressants. Also, alternatives to imipramine such as atomoxetine or reboxetine have been shown to have antienuretic effects [16-18]. Also, for severely therapyresistant enuresis, may opt for peripheral electrical stimulation or botulinum toxin injections into the detrusor and reported that moxibustin, injection acupuncture and laser acupuncture were effective treatments for childhood nocturnal enuresis. However, the effects of acupuncture compared to desmopressin remain inconclusive.
Conclusion
Nocturnal enuresis is common in our regions. Behavioral treatment associated with taking desmopressin can give good results.
Declaration of interests
The authors declare that they have no conflict interest for this article.
Ethical approval
None sought.
Funding
None declared.
References
- Aubert D, Berard E, Blanc JP, Lenoir G, Liard F, et al. (2010) Isolated primary nocturnal enuresis: International evident based management. Consensus recommendations by french expert group. Progrès en urologie 20(5): 343-349.
- Hjalmas K, Arnold T, Bower W, Caione P, Chiozza LM, et al. (2004) Nocturnal enuresis: an international evidence-based management strategy. J Urol 171(6Pt 2): 2545-2561.
- Neveus T, Gontard A, Hoebeke P, Hjalmas K, Bauer S, et al. (2006) The standardization of terminology of lower urinary tract function in children and adolescents: Report from the standardization committee of the Interna- tional Children’s Continence Society (ICCS). J Urol 176(1): 314-324.
- Haab F, Amarenco G, Coloby P, Grise P, Jacquetin B, et al. (2004) Terminologie des troubles fonctionnels du bas appareil urinaire: adaptation fran, caise de la ter- minologie de lInternational Continence Society. Prog Urol 14: 1103-1111.
- Sylla C, Moreira C (2005) Réflexions sur la prise en charge de lénurésie dans un centre hospitalier au Séné Progrès en Urologie 15: 296-301.
- Huang EM, Wei J, Sharma S, Bao Y, Li F (2020) Prevalence and risk factors of nocturnal enuresis among children ages 5–12 years in Xian, China: a cross-sectional study. BMC Pediatrics 20(1): 305.
- Ouedraogo A, Kere M, Ouedraogo T L, Jesu F (1997) Epidémiologie de Iénurésie chez les enfants et les adolescents de 5 à 16 ans à Arch Pediatr 4(10): 947-951.
- IHY Chan, KKY Wong (2019) Common urological problems in children: primary nocturnal enuresis. Hong Kong Med J 25(4): 305-311.
- Lachguer K (2007) Lénurésie chez lenfant: A propos de 154 cas. Thèse de médecine, Faculté de médecine et de pharmacie de Marrakech: Université Cadi Ayyad 47.
- Lottmann H (2000) Traitement de lénurésie nocturne en France. Presse Med 29(18): 987-990.
- Neve ́us T, Fonseca E, Franco I, Kawauchi A, Kovacevic L, et al. (2020) Management and treatment of nocturnal enuresisdan updated standardization document from the International Children’s Continence Society. J Pediatr Urol 16(1): 10-19.
- Glazener CM, Evans JH (2002) Desmopressin for nocturnal enuresis in children. Cochrane Database Syst Rev 2002(3): CD002112.
- Kwak KW, Lee YS, Park KH, Baek M (2010) Efficacy of desmopressin and enuresis alarm as first and second line treatment for primary monosymptomatic nocturnal enuresis: prospective randomized crossover study. J Urol 184(6): 2521-2526.
- De Guchtenaere A, Vande Walle C, Van Sintjan P, Donckerwolcke R, Raes A, et al. (2007) Desmopressin resistant nocturnal polyuria may benefit from furosemide therapy administered in the morning. J Urol 178(6): 2635-2639.
- Kamperis K, Hagstroem S, Faerch M, Mahler B, Rittig S, et al. (2016) Combination treatment of nocturnal enuresis with desmopressin and indomethacin. Pediatr Nephrol 32(4): 627-633.
- Ohtomo Y (2017) Atomoxetine ameliorates nocturnal enuresis with subclinical attention-deficit/hyperactivity disorder (ADHD). Pediatr Int 59(2): 181-184.
- Lundmark E, Ha gglo f B, Stenberg A, Neve ́us T (2016) Reboxetine in therapy-resistant enuresis e a randomized, placebo- controlled study. J Pediatr Urol 12(6): 397.
- Dalrymple RA, Wacogne ID (2017) Gradual withdrawal of desmopressin in patients with enuresis leads to fewer relapses than an abrupt withdrawal. Arch Dis Child Educ Pract Ed 102(6): 335.
-
Kouka SCN*, Sissokho M, Thiam NM, Jalloh M, Diop M, Faye M, Diame A, Diallo Y and Sylla C. Enuresis of Children in A Hospital Environment: Epidemiological, Diagnostic and Therapeutic Aspects in The Thies Region. Annals of Urology & Nephrology. 4(1): 2024. AUN.MS.ID.000576.
-
Regulatory dendritic cells, Kidney transplantation, Cell therapy, Specific immune microenvironment, Immunosuppressive agents, Kidney immunology, Genetic modification, Human leukocyte, Genetic modification, Drug intervention, Cytokine exposure, Immunosuppressant, Renal parenchyma
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






