 Research Article
Research Article
Easy Way for Double-J Stent Removal in A Pandemic Crisis Covid-19
Benslimane Hammou*
Pediatric Urology Department, Children Hospital of Oran, Faculty of Medicine of Oran, Algeria
Benslimane Hammou, Pediatric Urology Department, Children Hospital of Oran, Faculty of Medicine of Oran, Algeria
Received Date:April 01, 2024; Published Date:April 22, 2024
Abstract
Introduction: Double-J stent continues to be the gold standard in pediatric urology. Following the World Health Organization (WHO) declaration
of COVID19 as a pandemic, we have limited the surgical program in our country to situations that are of the utmost urgency because of the obvious
daily increase in new cases and the difficulties of performing COVID testing on every patient.
Material and Methods: prospective study performed in the pediatric urology. After establishment of the inclusion and exclusion criteria, A 6Fr
suction probe with a 4/0 thread was passed at the level of the first hole and knotted, and local anesthetic was applied with xylocaine gel, The thread
left long and protruding from the probe was introduced into the bladder through the urethra, and pain was assessed by a visual analog scale (VAS).
Results: Between January 2020 and May 2021, 98 patients were included according. No incidence: tied catheter, blocked JJ probe at the level of
the urethra and 1 case of partial extraction of JJ probe.
Discussion: Our study shows no difference regarding the method with cystoscopy.
Conclusion: Technique used as a conservative treatment for the ablation of the JJ probe in a specialized center to reduce the cost, time and
reduce the waiting list caused by COVID-19.
Keywords: Double J stent; covid-19; endoscopy
Introduction
The placement of a double-J stent remains the gold standard in pediatric urology for prophylactic or therapeutic purposes and provides drainage and protection of the anastomosis in urology [1]. After a delay, the JJ stent is removed by grasping forceps through rigid cystoscopy [2]. The procedure takes a few minutes, but the time is lengthened by the presence of the nursing staff in the operating room, and the admission of the patient to the operating room, anesthetic time, equipment sterilization time, and installation time (material and endoscopy) added to the operating time constitute the cost [3]. All of these factors add to the anesthesia risk present in all surgical procedures. All of these factors have prompted experts to seek alternatives to the placement of a JJ probe, especially ablation, such as flexible cystoscopy, flexible ureteroscopy, and magnetic stents, which are not available in all countries, until abandoning JJ placement [4].
Why this technique, timing: After COVID-19 was declared a pandemic by the World Health Organization (WHO), and we are gradually coming to better understand the mechanism of contamination between the population and especially in the hospital environment [5], we asked ourselves many questions for patients requiring surgical treatment. We thought of this technique in the midst of the COVID crisis. After having seen with great interest the publications concerning the organization of the operating rooms intended for COVID-19, the recent publications of the American Society of Gastrointestinal Surgery (Sages) and European Association of Endoscopy Surgery (Eases) found that the pressure room was negative [6]. In our country, given the clear daily increase in new cases and the impossibility of carrying out COVID-19 tests on all patients, the operating program has been reduced to cases of extreme urgency with the use of all staff and equipment. With the aim of gaining a place in the operating program for the benefit of seriously ill patients and after analyzing the risks of leaving a JJ probe, in particular, encrustations and micturition disorders [7].
Objectives
to evaluate the feasibility of this technique and its advantages, disadvantages compared of other techniques and evaluation of the cost of techniques.
Materials and Methods
Prospective study performed in pediatric urology. After establishment of the inclusion and exclusion criteria.
The inclusion and exclusion criteria were as follows:
a) After obtaining written consent from the parents, the
advantages of this technique were explained.
b) Radiological confirmation of the position of the double-J
stent by radiography was not performed in a systematic manner
before the procedures.
a) Inclusion criteria: All patients had JJ stents in place.
b) Exclusion criteria:
1) Presence of bilateral double -J stents.
2) Need for diagnostic or therapeutic cystoscopy.
3) Presence of signs of urinary tract infection.
Description of the method: Compared to the placement of a
urinary catheter in children in routine urology practice. Initially,
it was performed by a senior (first author, senior surgeon for
the second time) during the study period, followed by advanced
resident. Under local anesthesia with xylocaine gel introduced into
the urethra, a CH 6 aspiration probe with a 4/0 thread was passed
at the level of the first hole and tied. The thread was left long and
exceeded the probe, then introduced into the bladder through the
urethra. Once in the bladder, the wire is pulled in such a way as
to bring the end of the catheter back through the bladder neck,
the first sensation of crossing the neck (comparable to pulling on
the balloon of the Foley catheter). We pull on the probe (free end)
while maintaining tension on the wire. The aspiration probe is
exteriorized and brings the JJ stent into contact with it (Figure 1).
We set a threshold of 3 (three) attempts to declare a failure and
moved on to programming for ablation under general anesthesia
and/or by cystoscopy and general anesthesia. Pain was assessed
using the visual analog scale (VAS). All data were analyzed using
SPSS software.
I. Evaluation criteria:
a) Age, sex, side or laterality.
b) Operating time.
c) stenting duration JJ.
d) Length of hospital stay.
e) Cost, urinary tract infection, and pain were evaluated
using the visual analog scale (VAS) and compared with the
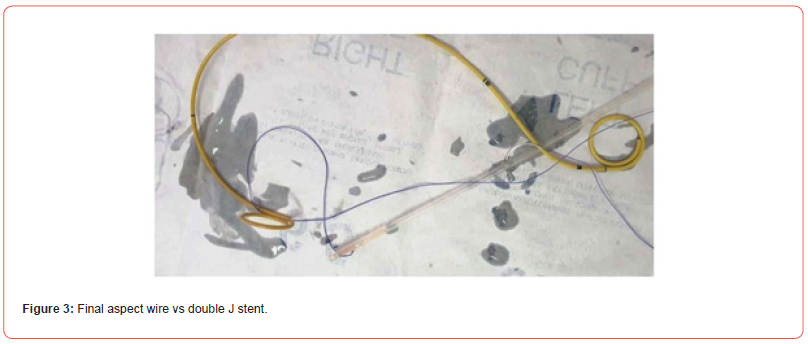
removal of a urinary catheter during the first procedure (Figure
2), and the final aspect aspiration probe with JJ stent as showing
the image (Figure 3).
f) Opinions of parents to optimize our study.


Results
Between April 2020 and May 2022, 98 patients aged between 0 and 15 years old participated in the study, with an average age of 30 months and an average duration of 85 days after the placement of a double-J stent.
The average number of attempts was 2, and 85% of the patients were male. Sixty percent of patients had a JJ stent on the left side. Ninety percent of patients undergo surgery for pyeloureteral junction disease (PUJ).
The operative time was 35 minutes for cystoscopy and 10 minutes for our method. Hospitalization for 2 h for our method vs. 6 h for cystoscopy with p-value of highly significant. 100% cystoscopy success versus 97% by our technique value not significant (5 cases of failure: including 3 removed by the same technique under general anesthesia and 2 cases cystoscopy). There were no knots at the aspiration probe level. One patient underwent partial extraction at the urethral orifice level. One case of urinary tract infection evolved favorably under antibiotic treatment. The P-value is very significant in terms of cost. Overly satisfied with parents.
Discussion
JJ stent is essential and provide safe methods for reconstructive surgery. Once in place, speech ablation general anesthesia, fasting, and placement in the operating program were initiated. Different materials for ureteral catheterization have been developed, but the availability of some is not guaranteed in all countries [8], especially incoming countries with a very large patient volume. Magnetic DJ stents are fascinating but expensive, not available, or very rarely available even in Western countries.
Conclusion
This technique was used as a conservative treatment for JJ stent ablation in a center dedicated exclusively to pediatric urology. The goal is to reduce the operating time, cost, and waiting list, and therefore forget the JJ stent, migration, and encrustation, given the volume of work during the COVID crisis. Informed Consent: given by patient parent for case presentation and all images.
Funding
No source of funding.
Competing Interests
The authors declare no competing interest.
Authors’ Contributions
B.H, give consent for acceptation of patient in the specialized center of pediatric urology department, examinate patients, coordinate all steps of work up, give diagnosis, operate patient, follow up, explain to parent all the clinical scenario, wrote notes and manuscript, review literature and submit manuscript, responsible of the content of manuscript and for all critical and review comment.
Acknowledgements
Thanks, given to parent patient to give consent for publishing this case.
References
- Finney RP (1978) Experience with new double J ureteral catheter stent. J Urol 120(6): 678‐681.
- Taylor WN, McDougall IT (2002) Minimally invasive ureteral stent retrieval. J Urol 168(5): 2020‐2023.
- Ozturk H (2017) Facilitate stent removal: magnetic DJ stent. Urol Case Rep 11: 55-56.
- Lai D, Chen M, Zha S, Wan S (2017) A prospective and randomized comparison of rigid ureteroscopic to flexible cystoscopic retrieval of ureteral stents. BMC Urol 17(1): 31.
- World Health Organization (2020) Coronavirus disease (COVID-2019) situation reports.
- Wax RS, Christian MD (2020) Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth 67(5): 568-576.
- Bregg K, Riehle RA (1989) Morbidity associated with indwelling internal ureteral stents after shock wave lithotripsy. J Urol 141(3): 510-512.
- Chew BH, Knudsen BE, Denstedt JD (2004) The use of stents in contemporary urology. Curr Opin Urol 14(2): 111-115.
-
Benslimane Hammou*. Easy Way for Double-J Stent Removal in A Pandemic Crisis Covid-19. Annals of Urology & Nephrology. 4(4): 2024. AUN.MS.ID.000592.
-
Double J stent; covid-19; endoscopy; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






