 Mini Review
Mini Review
Thymus is the Joker of the Neck in Children
Elham A Elgabaly Moustafa Ahmed1*, Amani Hilal Al Ysar2, Manal Ali Alraeesi2
1Department of Radiology, Consultant radiologist, Aljalia children specialty hospital, UAE
2Department of Radiology, Radiology technologist and Sonographer, Aljalia children specialty hospital, UAE
Elham A Elgabaly Moustafa Ahmed, Department of Radiology, Consultant radiologist, Aljalia children specialty hospital, UAE.
Received Date: February 07, 2021; Published Date:February 25, 2021
Abstract
In spite, remnants of thymus tissue can be found anywhere in the neck along the course of thymus decent from the submandibular region to the anterior mediastinum, the ectopic thymus is rarely recorded as a cause of neck masses especially in the pediatric age group. However, it should be included in the differential diagnosis of any neck mass or thyroid nodule in pediatric patients, according to clinical work.
Introduction and Background
The thymus gland is a lymphatic organ that is active in T lymphocyte differentiation. To understand the potential sites of the ectopic thymus tissue, the embryogenesis of the thymus and the thyroid glands should be clear.
During embryogenesis, the thymus gland developed from the ectoderm of the third branchial cleft and the endoderm of the third branchial pouch. The thymus gland is formed by the fusion of the right and left thymus primordial. Then it descends to the upper anterior mediastinum [1,2].
During embryogenesis, the thyroid gland developed between the first and second pharyngeal pouches near the tongue base forming the thyroid diverticulum which decent caudally along the midline and attached to the tongue by the thyroglossal duct [3].
Any interruption at any stage during thymus descent can lead to ectopic thymus, either extra thyroid or intra thyroid focus.
This study aims to demonstrate series of different varieties of neck ectopic thymus discovered during performing pediatric neck ultrasound for patients either presented by neck lesion or incidentally discovered during doing neck ultrasound for other reason, to increase the awareness of radiologist about the importance of considering the ectopic thymus in the differential diagnosis of any neck mass or any intrathyroidal nodule. Emphasizing the ultrasound features of the ectopic thymus tissues.
Review
Remnants of thymus tissue can be located all over the thymus descent path from the upper neck into the anterior mediastinum [4].
Aberrant thymic migration could be an extra thyroid or an intrathyroidal focus [5]. Because ectopic thymic tissues are typically asymptomatic, the actual prevalence is not known; the recorded prevalence in children is very low and was reported as 0.99% to 1.8% [5,6].
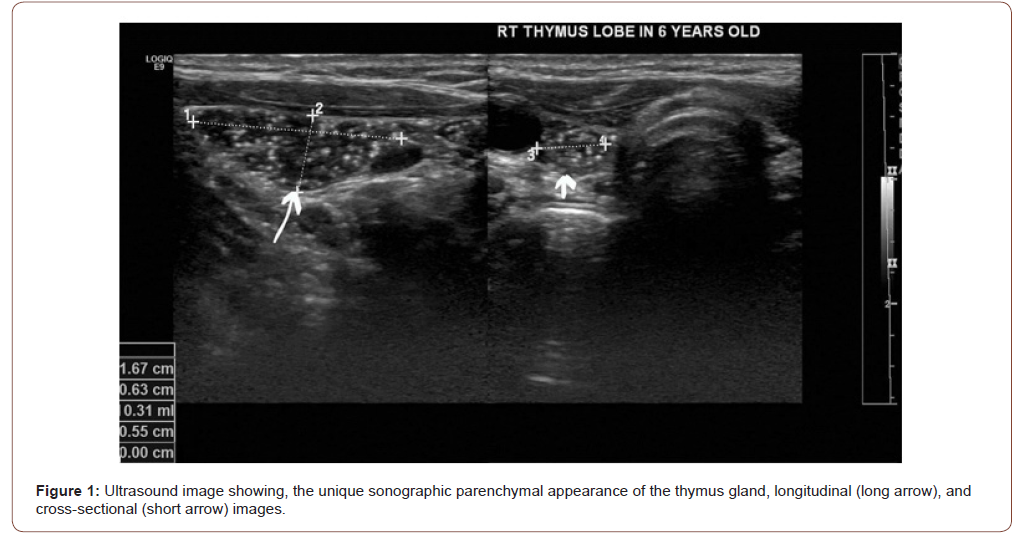
In one cohort study, the ectopic thymus was incidentally found in 16 (9 males, 7 females) of 690 (2.3%) children who underwent neck or thyroid ultrasonography [5]. By ultrasound, the thymus gland appears homogenous with multiple echogenic foci giving a “starry sky” appearance [7] (Figure 1).
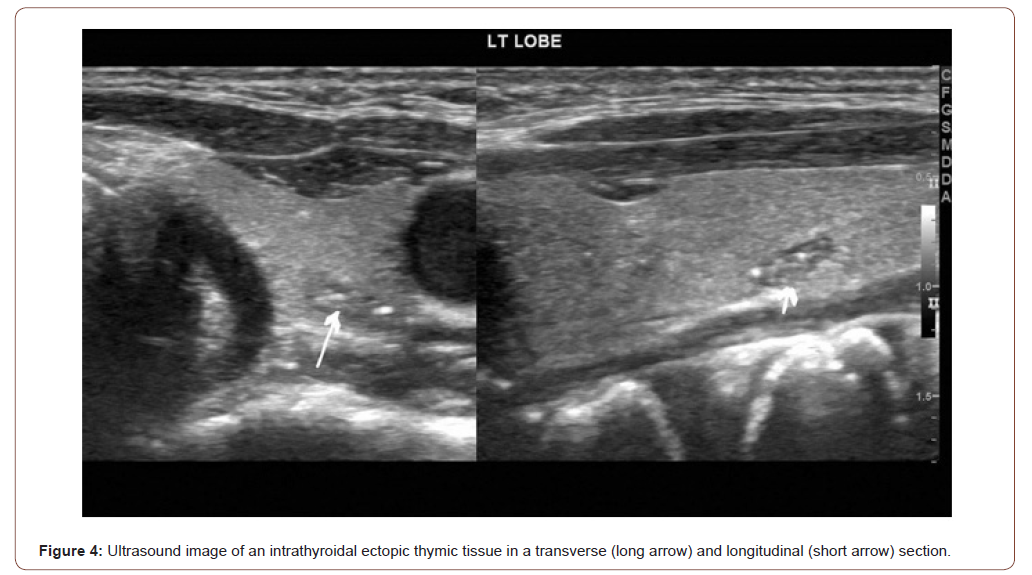
By ultrasound, most of the intrathyroidal ectopic thymic tissue was found in the middle portion of the right lobe, they are fusiform or oval in shape [6].
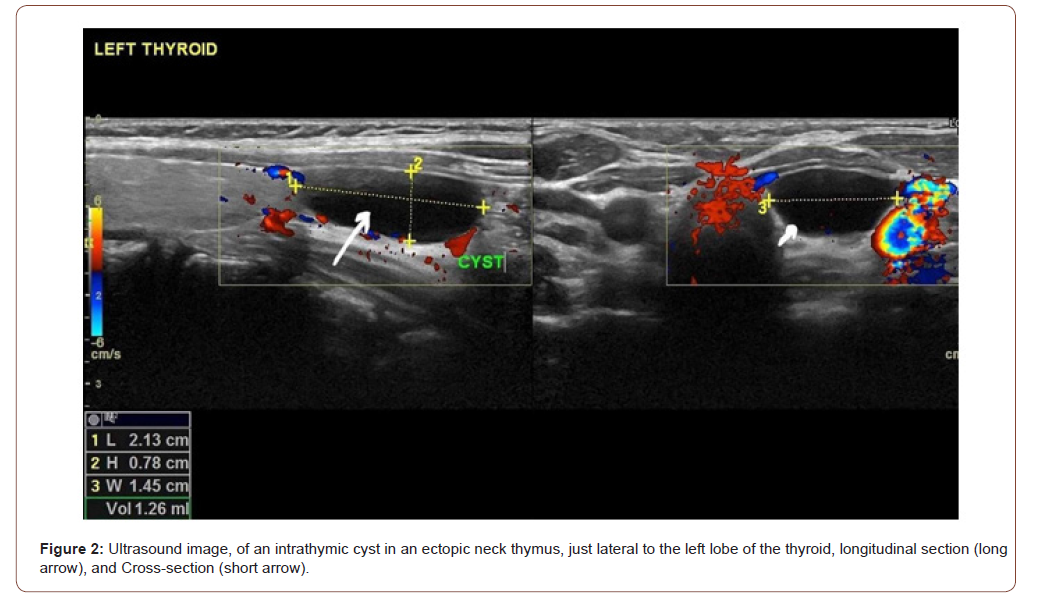
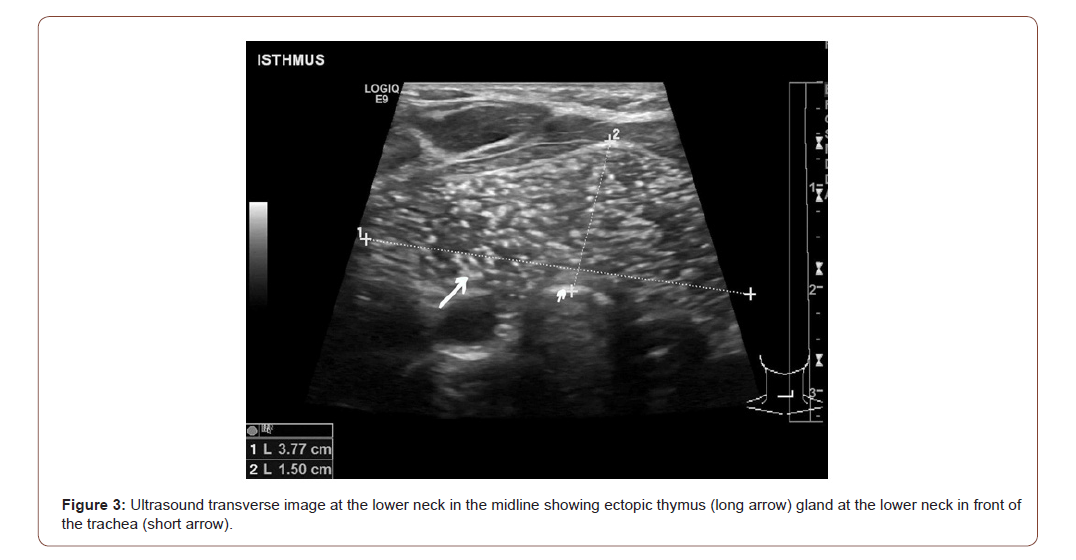
The extra thyroid thymus gland shows two distinct macroscopic forms-cystic and solid. The cystic type [8,9] is recorded more commonly. Two separate entities are found in this form: a thymic cyst, originating from a thymopharangeal duct, and a solid extra thyroid thymus with cystic changes [8,9] (Figure 2&3).
The ultrasound appearance of the intrathyroidal ectopic thymic tissue can strongly mimic papillary thyroid carcinoma. The extrathyroid ectopic thymic tissue is similar to pathological lymph nodes in the ultrasound [5]. Therefore, the differential diagnosis of thyroid nodules or neck masses should include ectopic thymus [6] (Figure 4).
Because of the high risk of malignancy in thyroid lesions in children, the resemblance of ultrasound features of papillary thyroid carcinoma and intra thyroid ectopic thymus, and the possibility of malignancy in ectopic thyroid, only cytological evaluation provides a definitive diagnosis [5] (Figure 5).
Conclusion
Every radiologist working with a pediatric neck ultrasound should bear in mind the unique ultrasound appearance of thymic tissues (starry sky appearance). This would help discourage a neck lesion from being misinterpreted and therefore prevent unwanted anxiety or interference.
Cytological examination only gives a conclusive diagnosis because of the high risk of malignancy in thyroid lesions in infants, the resemblance of ultrasound characteristics of papillary thyroid carcinoma and intra thyroid ectopic thymic tissues, and the probability of malignancy in the ectopic thymus.
Acknowledgement
Dr. Nandu Nandu KS Thalange, MBBS BSc, FRCP, FRCPCH, FHEA (Consultant Paediatric Endocrinologist in Aljalila Children Speciality Hospital) and Miss Jukha Sh.A.Al Marzooqi, Director of the Clinical Support Services in Aljalila Children Speciality Hospital for support.
Conflict of Interest
No conflict of interest.
References
- Kim HG, Kim MJ, Lee MJ (2012) Sonographic appearance of intrathyroid ectopic thymus in children. J Clin Ultrasound 40(5): 266-271.
- Kabaalioğlu A, Öztek MA, Kesimal U, Çeken K, Durmaz E, et al. (2017) Intrathyroidal ectopic thymus in children: a sonographic survey. Med Ultrason 19(2): 179-184.
- Fukushima T, Suzuki S, Ohira T, Hiroki Shimura, Sanae Midorikawa, et al. (2015) Prevalence of ectopic intrathyroidal thymus in japan: the fukushima health management survey. Thyroid 25(5): 534-537.
- Escobar FA, Pantanowitz L, Picarsic JL, Craig FE, Simons JP, et al. (2018) Cytomorphology and sonographic features of ectopic thymic tissue diagnosed in pediatric FNA biopsies. Cytopathology 29(3): 241-246.
- Stasiak M, Adamczewski Z, Stawerska R, Krawczyk T, Tomaszewska M, et al. (2019) Sonographic and Elastographic Features of Extra- and Intrathyroidal Ectopic Thymus Mimicking Malignancy: Differential Diagnosis in Children. Front Endocrinol (Lausanne) 10: 223.
- Tokiko Ishida, Hirokazu Kotani, Masashi Miyao, Hitoshi Abiru, Chihiro Kawai, et al. (2013) Ectopic cervical thymus associated with infant death: 2 case reports and literature review. Int J Pediatr Otorhinolaryngol 77(9): 1609-1612.
- Smita Manchanda, Ashu S Bhalla, Manisha Jana, Arun K Gupta (2017) Imaging of the pediatric thymus: Clinicoradiologic approach. World J Clin Pediatr 6(1): 10-23.
- Bychkov A (2015) Thymic tissue. PathologyOutlines.com.
- Chu WCW, Metreweli C (2002) Ectopic thymic tissue in the paediatric age group. Acta Radiol 43(2): 144-146.
-
Elham A Elgabaly Moustafa Ahmed, Amani Hilal Al Ysar, Manal Ali Alraeesi. Thymus is the Joker of the Neck in Children. Anaest & Sur Open Access J. 2(4): 2020. ASOAJ.MS.ID.000541.
-
Thymus gland, Organ, Thymus tissue, Neck, Ectopic thymus, Pediatric patients, Embryogenesis, Diagnosis
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






