 Research Article
Research Article
Respiratory Support Adjustments in Ventilated Patients Performing Early Mobilisation A Pilot Observational Service Evaluation
Kalsi S1, Pertou A2 and Thomas AJ3*
1The Royal London Hospital, Barts Health NHS Trust, Whitechapel, London, UK
2Newham University Hospital, Barts Health NHS Trust, Newham, London, UK
3Critical Care Outreach, The Royal London Hospital, Barts Health NHS Trust, Whitechapel, London, UK
Thomas AJ, Critical Care Outreach, The Royal London Hospital, Barts Health NHS Trust, Whitechapel, London, UK.
Received Date: October 01, 2022; Published Date:October 14, 2022
Introduction
Early mobilisation in the critical care unit is an accepted intervention to prevent the physical and non-physical morbidity associated with bed rest, mechanical ventilation, and critical illness. When early mobilisation is performed with patients who remain mechanically ventilated, the anticipated increase in exercise induced ventilatory demand (or work of breathing) can be offset by adjusting select mechanical ventilation variables for the duration of the exercise/mobilisation task. Gonzalez-Seguel and colleagues (2021) recently published a scoping review to explore the nature of “respiratory support adjustments” during early mobilisation of ventilated patients which identified limited published reports and no English language guidelines to describe the practice. In the scoping review, seven published articles were identified that reported mechanical ventilator adjustments during early mobilisation of which three (3) detailed continuous arm or leg ergometry [1-3]. The remaining four (4) reports detailed progressive functional mobilisation consistent with the early mobilisation practice observed in most United Kingdom critical care units [4-7]. Ventilator adjustments in these later reports were described as either increases in pressure support or increases in FiO2, or a combination of these adjustments. The ventilation mode and settings in these reports were inconsistently described and the clinical reasoning underlying the adaptations never explored.
Aims
Since adjustments to mechanical ventilation settings are used by Physiotherapy teams completing early mobilisation of ventilated critically ill patients in our clinical setting, this pilot observational evaluation was designed to test the feasibility of exploring these ventilator adjustments. If the pilot evaluation demonstrates that the method and procedures are feasible in a clinical setting, a subsequent larger scale study will be pursued. Specifically, this pilot sought to: -
• Assess the potential for recruitment of ventilated critical care patients for whom ventilator adjustments were introduced during an activity intervention.
• Describe the characteristics of the ventilated critical care cohort for whom ventilator adjustments were introduced during an activity intervention.
• Describe the Physiotherapy clinical reasoning underlying the decision to adjust ventilation settings to complete an activity intervention.
• Describe the baseline ventilation settings from which adjustments were attempted.
• Describe the activity interventions associated with ventilator adjustments.
• Describe the frequency and type of adjustments made to ventilator settings.
• Describe any change in physiological parameters associated with the activity interventions supported by ventilator adjustments.
• Describe the temporal characteristics of ventilator adjustments in relation to the start and completion of activity.
It is hoped that exploring ventilator adjustments during activity interventions within our clinical setting (as a pilot) will increase understanding of how and why ventilator adjustments are utilised, the observed physiological outcomes and any unanticipated effects. Completing this pilot should support and inform the development of a future multicentre trial and quantitative analysis [8]. This may in turn lead to the development of standard operating procedures or guidelines for clinical practice.
Methods
Physiotherapy teams from two Barts Health NHS Trust Adult Critical Care Units (The Royal London Hospital and Newham University Hospital) participated in the data collection for this pilot over a 5-month period (January 2022 – May 2022). A nonrandomised convenience sample of ventilated patients receiving activity interventions (Monday to Friday) with ventilator support adjustments were included. A data collection tool was developed and trialled in consultation with the Barts Health Respiratory Physiotherapy Forum and included: -
• Anonymised patient demographics and airway type (ETT or Tracheostomy).
• Baseline, intervention, and post intervention ventilator characteristics including ventilator mode, pressure support (PS), positive end expiratory pressure (PEEP), tidal volume (TV), minute volume (MV), rapid shallow breathing index (RSBI) and the fraction of inspired oxygen (FiO2)
• Baseline, intervention, and post intervention physiological markers including arterial saturation (SaO2), respiratory rate (RR), heart rate (HR) and systolic blood pressure (SBP)
• The intervention delivered based was classified according to the internationally agreed ICU activity codes and definitions which were developed at the Fifth Annual International ICU Physical Medicine and Rehabilitation meeting in San Francisco [9].
• Clinical reasoning for adjusting the ventilator from a selection of three responses (known increase in work of breathing with intervention, anticipated increase in work of breathing with intervention or high baseline minute volume).
• The timing of ventilator adjustments prior to and at the cessation of the intervention from a selection of 4 time points (at the same time as activity start or end, within 1-2mins of activity start or end, 5mins before activity start or end, and 10mins before activity start or end).
data fields from each site were anonymised and combined to create a master data set which was stored electronically in a locked non-clinical area. The combined data was analysed using descriptive statistics and frequency histograms, rather than inferential statistics, since the goal of the pilot was not to test hypotheses. Similarly, since this was a pilot investigation, it was not deemed necessary to provide power analyses for the proposed sample size [10]. For the purposes of the pilot investigation, to accommodate data comparison and prevent data rejection from incomplete data fields, the total number of events from which descriptive statistics were derived was noted. This pilot evaluation was approved by the Barts Health Clinical Effectiveness Unit (Project 12311: Scoping Respiratory Support Adjustment during Physiotherapy Intervention).
Results
Demographics: Thirteen (13) ventilated patients with a mean age of 55 ± 16yrs were included in the sample. 46% of the sample had a diagnosis that included COVID-19 (6/13). 100% of these patients had received a tracheostomy during their critical care admission and were experiencing activity with a mean time from tracheostomy insertion of 12.5 ± 11 days (N = 13). The total number of ventilator adjustment events included in this pilot was 15 events. Three activity events were excluded from the analysis since patients were self-ventilating at baseline, in 2 events the patient was self-ventilating via a tracheostomy mask (TM) and in one event the patient was receiving High Flow Oxygen Therapy (HFOT) via a facemask.
Baseline: The mode of ventilation from which most activity events started was Pressure Support (PSV 61%), followed by Synchronised Intermittent Mandatory Ventilation (SIMV 11%), Pressure Control Ventilation (PCV 5.6%), and Pressure Regulated Volume Control (PRVC 5.6%) respectively (N = 15 events). Table 1 outlines the mean ventilator settings and physiological parameters recorded prior to the activity intervention.
Table 1:Baseline, intervention and post intervention ventilator settings and physiological parameters.
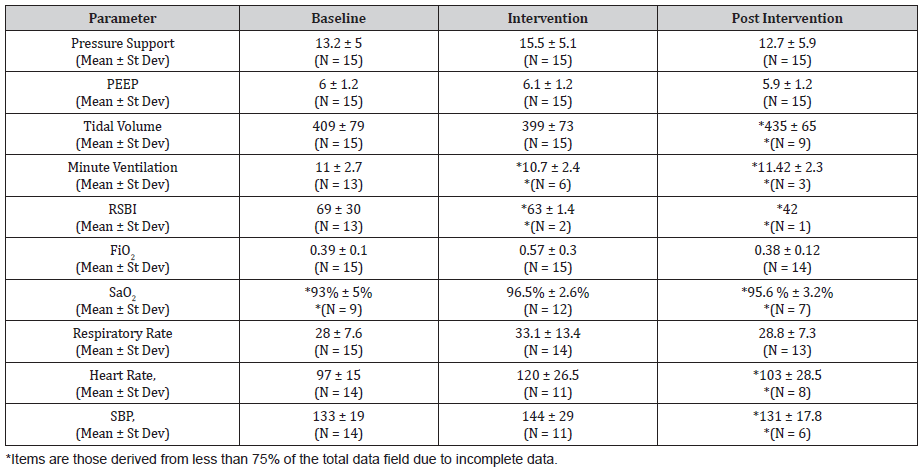
Intervention: The activity which occurred with the greatest frequency was “sitting on the edge of the bed” (SOEOB, Hodgson, 2012) representing 60% of all activities. Hoist transfers, limb exercises in the bed and standing practice each occurred with a frequency of 13.1% respectively. No walking interventions were reported (N = 15 events). The most common reason for adjusting the ventilator was an anticipated increase in the work of breathing (74%), while a known increase in the work of breathing with activity was reported in 13.3 % of cases. A high baseline minute volume was recorded as the reason for ventilator adjustments in the remaining 13.3% of events (N = 15 events). The adjustments that occurred with the greatest frequency were an increase in FiO2 alone (26.7%), and an increase in Pressure Support alone (26.7%). Increases in both the PS and FiO2 combined represented the 2nd most frequent change (20%) followed by providing a mandatory rate (13.3%). Changing the ventilator mode and increasing the PEEP and FiO2 together, both occurred with a frequency of 6.7% respectively (N = 15 events).
Adjusting the ventilator support 5mins prior to the activity occurred with the highest frequency (46.6%), followed by 1-2mins prior to the activity (33.4%), 10mins prior to the activity (13.3%) and at the same time as the activity (6.7%). (N = 15 events). Table 1 outlines the mean ventilator settings and physiological parameters recorded during the activity intervention. Post Intervention: Returning the ventilator to baseline settings following the activity intervention occurred in 73% of the events while in 27% of events, ventilation was adjusted to another level (N = 15). Reducing the ventilator support within 10mins of the activity occurred with the greatest frequency (40%). Ventilator adjustments within 5 mins, and immediately on cessation of activity occurred with the same frequency respectively (20 %), while reducing the ventilator support within 1-2mins of the activity cessation occurred in 13.3% of events. In one event (6.7%), the patient remained on the adjusted ventilator setting as their new mode of ventilation. (N = 15). Table 1 provides mean ventilator settings and physiological parameters recorded at the conclusion of the intervention.
For clarity, two case examples (case example 1 and 2) are provided demonstrating individual baseline, intervention and post intervention data associated with ventilator adjustment supported rehabilitation activity.
Case Example 1: A 71yr old male receiving pressure support ventilation (PS 13, Peep 5) via tracheostomy with an FiO2 0.25, respiratory rate 26 breathspmin-1 and heart rate of 107 bpmin-1 at rest. 10mins prior to a SOEOB intervention the pressure support was increased to 18 (Peep 5) while the FiO2 remained at 0.25. The pressure support was increased due to an anticipated increase in the work of breathing associated with the activity and achieved a tidal volume of 350mls during the activity with a respiratory rate of 21 breathspmin-1 and HR elevation to 111bpmin-1. Within 10mins of completion of the activity the pressure support was reduced to 12, Peep increased to 8 and FiO2 increased to 0.55.
Case Example 2: A 36yr old male was receiving pressure support ventilation (PS 13, Peep 7) via tracheostomy with an FiO2 0.45 yielding tidal volumes of 320mls. Baseline SaO2 was 85%, respiratory rate 25breathspmin-1, and HR 103bpmin-1. Five (5) minutes before starting “exercises in the bed” the FiO2 was increased to 0.60 due to the anticipation of desaturation with activity. During activity the patient had SaO2 of 94% a RR of 30breathspmin-1 and HR 110bpmin-1. On completion of the bed exercises the FiO2 was immediately returned to 0.40, 5% lower than prior to the activity, while the pressure support was able to be reduced to 8 yielding tidal volumes of 400mls.These settings resulted in saturations of 96%, a respiratory rate of 25 breathspmin-1 and HR 93 bpmin-1.
Discussion
The rationale for completing this pilot was to explore the feasibility of recording the characteristics of ventilation adjustments during rehabilitation interventions in a ventilated critical care cohort. Feasibility can be determined by exploring process issues (recruitment); resource issues (time to complete data capture); data management issues (human and data optimization); and scientific issues (safety of intervention and treatment effect estimation). Most of the specific aims of this pilot relate to how accurately the data collection form reflected the various characteristics in question. For example, the form captured demographics of the ventilated cohort including age, airway type, the time between tracheostomy insertion and activity and COVID-19 status. However, the sex of the cohort was not included and if the cohort were expanded in a larger trial, the “time between intubation and activity” may be instructive to include, since some participants may not have received a Tracheostomy at activity participation.
We were surprised by the low volume of data captured during this pilot, given that the sampling period spanned 5-months. The true frequency of ventilator adjustments during early mobilisation of critically ill patients in these hospitals could not be determined since the data collection was not designed to capture every example of the use of this technique. It is possible that ventilator adjustments were occurring during rehabilitation when data therapists were absent (e.g., on weekends). Since the total number of activity interventions performed across the 5-months was not captured, it is impossible to determine the volume of ventilator adjusted mobilisation in relation to the total activity interventions delivered during that time.
The volume and frequency of rehabilitation in mechanically ventilated patients in critical care has been previously reported as low. Thomas, et al. [11] reported low incidence of active rehabilitation techniques in patients receiving controlled ventilation (4%) or with an ETT (8%). In a one-day point prevalence survey in Germany [12], only 24% of 783 mechanically ventilated patients and 8% of patients with an ETT were mobilised out of their beds. A multi-centre prospective cohort study completed across 1,351 days in twelve ICU’s in Australia and New Zealand revealed that early mobilisation of mechanically ventilated patients was “uncommon” [13]. These results indicate the low prevalence of this rehabilitation practice when compared to activity occurring in non-ventilated or tracheostomised cohorts.
A post hoc count of rehabilitation interventions delivered to ventilated patients in one of the pilot centres (44 beds at the Royal London Hospital), revealed approximately 100 events in a month. Extrapolating this count to the frequency of activity events captured in this pilot demonstrates than only 3% of the total activity interventions included ventilator adjustments. If the frequency of ventilator adjusted activity is very low, data collection in a larger trial would need to extend beyond 5 months to achieve a sample size suitable for quantitative analysis. It is possible that data collecting therapists chose not to record every example of ventilator adjusted exercise due to data fatigue or the burden associated with the volume of data collected. We did not ask the data collectors their thoughts regarding the volume of data required for each event but recognise that 30% of data (see Table 1) is incomplete, particularly in the post intervention variables. Attention to rationalising data volume for the definitive trial is warranted, along with an indication of total activity interventions performed across the data collection period.
The clinical reasoning underlying the decision to adjust ventilation settings to complete an activity intervention was able to be reported, but only with respect to three defined options presented. The addition of a free text category may have revealed further clinical indications unknown to the investigation team. Our report of baseline ventilation settings from which adjustments were attempted is consistent with previous reports Gonzalez-Seguel, et al. [14] with pressure support ventilation (PSV) and SIMV being the most frequent baseline ventilation mode. We were surprised that pressure control ventilation (PCV) and pressure regulated volume control (PRVC) were reported since these modes are usually associated with high sedation levels perhaps incompatible with participatory rehabilitation. It would also be interesting to explore whether the controlled ventilation modes were associated with the lower intensity activity within a larger trial to confirm this assumption. There is also evidence that proportional ventilation modes (proportional assist ventilation, PAV and neutrally adjusted ventilatory assist, NAVA) may improve exercise performance and work efficiency in ventilated subjects [15]. The investigation team should ensure a wider range of ventilation mode options are able to be selected for the definitive trial.
The activity interventions associated with ventilator adjustments, type of ventilator adjustments and temporal characteristics of ventilator adjustments were able to be reported without difficulty. Expanding the response options within the ordinal scale temporal variables may improve the ability to apply parametric statistical testing within a larger trial and deserves some consideration [16]. Although we were able to report the time frames for post intervention ventilator adjustments, we were also aware that in 27% of our events, ventilation was adjusted to another level following activity completion. The short case series also demonstrate that the post activity ventilator adjustment was not always a reduction in ventilator support or oxygen requirement (see Case Study One). To explore this aspect of the technique further, a qualitative response option could be considered asking data collectors to rate the post activity ventilator setting as “greater than” or “less than” the baseline support, which may enhance determinations of safety and efficacy.
Conclusion
The overall purpose of this pilot study was to assess the feasibility of conducting a larger scale investigation exploring ventilator adjustments during activity interventions in ventilated critical ill patients. Based on the Thabane, et al. [8] criteria for determining pilot study success, we conclude it is feasible to pursue a larger scale study providing modifications to the data collection form are completed. We also conclude that given the low frequency of ventilator adjustments observed in this pilot, a multi-centre prospective trial should be pursued to generate sufficient data for realistic comparative analysis.
Acknowledgments
None.
Conflict of Interest
None.
References
- Akoumianaki E, Dousse N, Lyazidi A, Lefebvre J-C, Graf S, et al. (2017) Can proportional ventilation modes facilitate exercise in critically ill patients? A physiological cross-over study. Ann. Intensive Care 7: 64.
- Kho ME, Molloy AJ, Clarke FJ, Daana Ajami, Magda McCaughan, et al. (2016) Canadian Critical Care Trials Group: TryCYCLE: A prospective study of the safety and feasibility of early in-bed cycling in mechanically ventilated patients. PLoS One 11: e0167561.
- Chen YH, Lin HL, Hsiao HF, Ching-Tzu Huang, Kuo-Chin Kao, et al. (2015) Effects of an additional pressure support level on exercise duration in patients on prolonged mechanical ventilation. J Formos Med Assoc 114: 1204-1210.
- Black C, Grocott M, Singer M (2020) The oxygen cost of rehabilitation interventions in mechanically ventilated patients: An observational study. Physiotherapy 107: 169-175.
- Ko Y, Cho YH, Park YH, Hyun Lee, Gee Young Suh, et al. (2015) Feasibility and safety of early physical therapy and active mobilization for patients on extracorporeal membrane oxygenation. ASAIO J 61: 564-568.
- Mah JW, Staff I, Fichandler D (2013) Resource-efficient mobilization programs in the intensive care unit: Who stands to win? Am J Surg 206: 488-493.
- Bailey P, Thomsen GE, Spuhler VJ, Robert Blair, James Jewkes, et al. (2007) Early activity is feasible and safe in respiratory failure patients. Crit Care Med 35: 139-145.
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, et al. (2010) A Tutorial on pilot studies: the what, why and how. BMC Medical Research Methodology: 10(1).
- Hodgson C (2012) ICU Activity Codes and Definitions.
- Bell ML, Whitehead AL, Julious SA (2018) Guidance for using pilot studies to inform the design of intervention trials with continuous outcomes. Clinical Epidemiology 10: 153-157.
- Thomas AJ, Wright K, Mill L (2009) The incidence of physiotherapy and rehabilitation activities within a general intensive care unit. Journal of the ACPRC 41: 3-8.
- Nydahl P, Ruhl AP, Bartoszek G, Dubb R, Filipovic S, et al. (2014) Early mobilisation of mechanically ventilated patients: A 1-Day point prevalence study in Germany. Critical Care Medicine 42(5): 1178-1186.
- The Team Study Investigators (2015) Early mobilisation and recovery in mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Critical Care 19: 81.
- Gonzalez-Seguel F, Camus-Molina A, Jasmen A, Jorge Molina, Rodrigo Pérez-Araos, et al. (2021) Respiratory Support Adjustments and Monitoring of Mechanically Ventilated Patients performing early mobilisation: a scoping review. Critical Care Explorations: 3(4): e0407.
- Koumianaki E, Dousse N, Lyazidi A, Jean-Claude Lefebvre, Severine Graf, et al. (2017) Can proportional ventilation modes facilitate exercise in critically ill patients? A physiological cross-over study: Pressure support versus proportional ventilation during lower limb exercise in ventilated critically ill patients. Ann Intensive Care 7: 64.
- Wu, Huiping, Leung, Shing ON (2017) Can Likert Scales be Treated as Interval Scales?—A Simulation Study. Journal of Social Service Research: 1-6.
-
Kalsi S, Pertou A and Thomas AJ*. Respiratory Support Adjustments in Ventilated Patients Performing Early Mobilisation A Pilot Observational Service Evaluation. Anaest & Sur Open Access J. 3(4): 2022. ASOAJ.MS.ID.000569.
-
Critical care unit, Ventilator, Physiotherapy, Fraction of inspired oxygen (FiO2), Saturation (SaO2), Respiratory rate (RR), Heart rate (HR), Systolic blood pressure (SBP)
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






