 Case Report
Case Report
Ovary-Sparing Surgery for Ovarian Dermoid Cysts in Children: A Report of Two Cases and Literature Review
Volkan Sarper Erikci1* and Merve Üstün2
1Department of Pediatric Surgery, Sağlik Bilimleri University, İzmir Faculty of Medicine, Turkey
2Resident in Pediatric Surgery, Sağlik Bilimleri University, İzmir Faculty of Medicine, Turkey
Volkan Sarper Erikci, Department of Pediatric Surgery, Sağlik Bilimleri University, İzmir Faculty of Medicine, Turkey.
Received Date: March 11, 2023; Published Date: April 10, 2023
Abstract
Ovarian lesions during childhood and adolescence are rare and most of these are benign. Mature teratomas are frequently seen in these cases. The most common of these masses in children are the mature cystic teratoma which are also known as dermoid cysts. The management of children with ovarian dermoids has evolved over recent years in a manner of ovary preservation. In this review article two cases of ovarian dermoids are presented. The tumoral mass was totally excised in both of these cases preserving the effected ovary in an ovary sparing manner. The medical history of the patients, radiological and histopathological findings are also given together with a brief literature review on this issue.
Keywords:Ovarian-sparing surgery; children; ovarian dermoid
Introduction
Ovarian lesions in pediatric population are relatively rare and can be categorized as functional or neoplastic. According to their cell of origin these benign and malignant lesions can be subdivided an epithelial, germ cell, sex cord-stromal or metastatic [1]. Approximately one-fourth of all ovarian neoplasms are germ cell derived tumors and the majority of these are benign teratomas or dermoid cysts [2]. In this review article two children with ovarian dermoids are presented and it is aimed in this study to present the presentation, diagnosis and management of ovarian dermoid cysts in children with special regard to ovarian sparing surgery (OSS). The medical history of the patients, radiological and histopathological findings are also given and the topic is discussed under the light of relevant literature.
Case Reports
Case 1
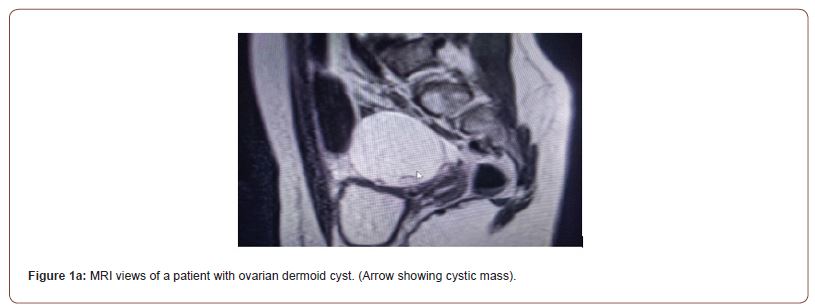
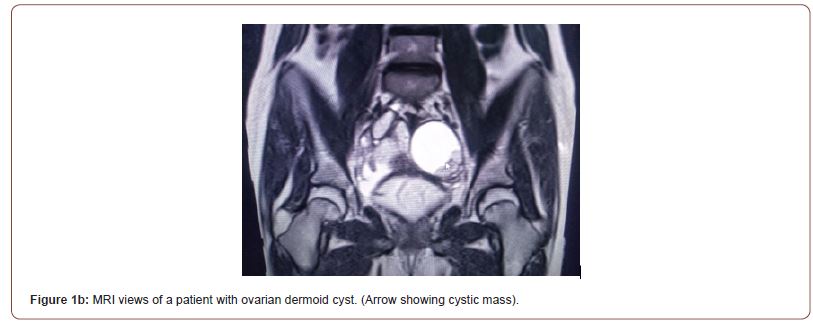
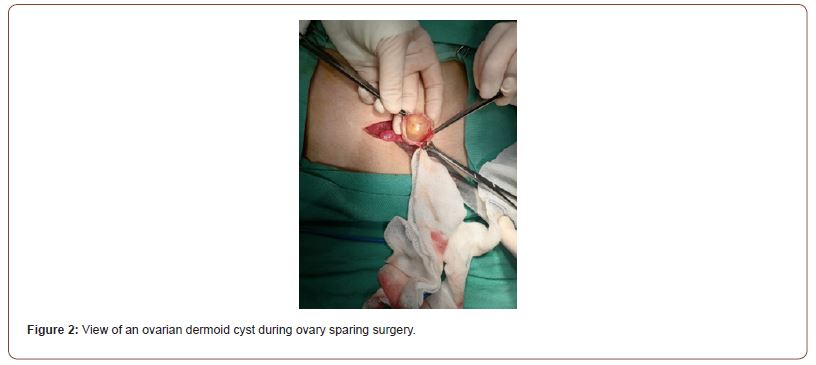
16-year-old girl was presented with intermittent abdominal pain for 1 year before admission to our hospital. Physical examination revealed no pathological findings. Ultrasonography (US) showed a septated cystic mass adjacent to the right ovary measuring 3.4x2.9 cm in size with no echogenicity. Magnetic resonance imaging (MRI) showed similar findings (Figure 1). The tumor markes including beta-HCG, AFP, CEA, CA-125, CA 19.9 and LDH levels were within normal ranges with respect to patient age. After consultation with pediatric oncology surgical treatment was planned. With an ovary sparing manner, total excision of the mass was per formed via open surgical approach (Figure2). She was discharged 24 hours after surgery without complications. After 1 month of follow up physical examination and scrotal USG were negative for recurrence of the disease.
Case 2
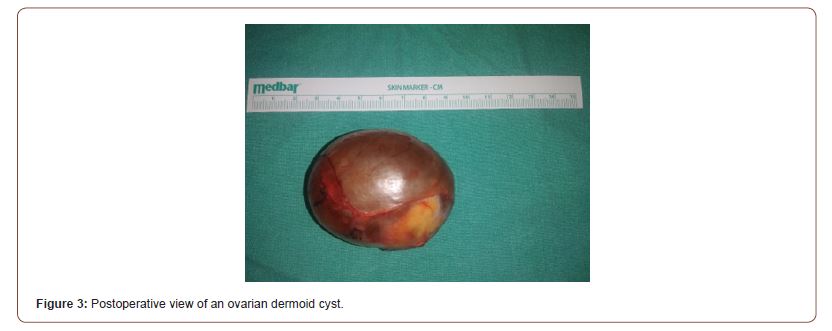
A 14-year-old female presented with abdominal pain. Physical examination was otherwise normal. Ultrasonography (US) showed a cystic mass located in the left ovary measuring 5.6x4.3x4.6 cm in size with no echogenicity. Doppler interrogation showed no vascularity in that cystic mass. Magnetic resonance imaging (MRI) showed similar findings and tumor markes including beta-HCG, AFP, CEA, CA-125, CA 19.9 and LDH levels were normal with respect to age of the patient. After consultation with pediatric oncology surgical treatment was planned. With an open surgical approach via pfannenstiel incision using an ovary sparing surgery, total excision of the mass was performed (Figure 3). She was discharged 24 hours after surgery without complications. After 2 months of follow up physical examination and scrotal USG were negative for recurrence of the disease.
Discussion
In contrast to adults, the majority of ovarian neoplasms in children are benign and it has been reported that malignancy occurs in approximately 10-20% of ovarian neoplasms in children [3-5]. Ovarian teratomas are the most frequent type of ovarian mass during childhood and adolescents [6]. With an incidence of 2.6 /100.000, about 75% of them are benign pathology [7]. These tumors are embryonal neoplasms and include two or three germ layers [8]. According to World Health Organization classification these tumors are divided into mature and immature teratomas and the most common teratomas in children are the mature cystic which are also named as dermoid cysts [9].
The evaluation of children with ovarian lesions includes patient history, physical examination, laboratory tests and imaging findings. These tumors can be diagnosed incidentally during examination for menstrual abnormalities or hydronephrosis [6]. Clinical presentation may include abdomino-pelvic pain together with palpable pelvic mass [10]. These patients may also be diagnosed as acute abdomen and signs of peritonitis due to ovarian torsion or hemorrhage [11].
Preoperative investigations include ultrasound, computed tomography or magnetic resonance imaging. In addition, tumor markers including alpha fetoprotein (AFP), human chorionic gonadotropin (HCG), lactic dehydrogenase (LDH), CA-125, CA-19.9, CEA should be obtained. Based on imaging findings ovarian neoplasms can be subclassified as cystic, complex or solid [12]. Although tumor markers are generally found to be elevated in malign ovarian lesions, it should be kept in mind that 20% of pediatric benign ovarian neoplasms can be associated with increased levels of tumor markers [13]. Tumor markers in both of our cases presented in this study were found to be within normal limits with respect to patient ages.
After the evaluation of these children with ovarian masses with the history, physical examination, imaging studies and tumor markers, preoperative risk stratification and patient selection for OSS can be performed. Traditional surgical management of ovarian dermoids has been oophorectomy via laparotomy. Potential negative effects of oophorectomy include an increased risk for early menapause, premature ovarian failure, impaired sexual growth, low bone density, neurological and cardiac disease in adulthood, and decreased potential for future fertility [14-17]. Because of these negative effects OSS is now considered standard surgical approach for benign ovarian lesions and includes removal of the tumor only preserving the surrounding normal ovary in place. This procedure can be done via laparoscopic approach or with an open laparotomy. In adults laparoscopy has become the accepted approach, however in childhood the preferred surgical approach remains controversial. Advantages of laparoscopic approach include reduced intraoperative blood loss, shorter hospital stay, reduced analgesic requirement, earlier return to daily activities, and improved cosmesis [18-26]. Disadvantages of laparoscopy include increased risk of intraoperative cyst rupture, spillage of cyst contents into abdominal cavity, increased adhesions, chemical peritonitis, and possible upstaging of malignant neoplasms. No matter which kind of surgical intervention either open surgery or laparoscopy is performed, in the case of cyst rupture saline lavage of the abdominal cavity has been shown to be effective in reducing the inflammation and adhesion formation in a rabbit model [27]. Neither of our cases did not face cyst rupture during surgical intervention and OSS was performed without any peroperative complications including cyst rupture or bleeding. Another concern regarding OSS for ovarian dermoids is the possibility of increased risk of recurrence. In a study 4.2% of patients treated laparoscopically revealed recurrence of ovarian dermoids as compared to none in 150 laparotomy cases [24]. It has been suggested that the increased dermoid recurrence rate following laparoscopic cystectomy may be due to incomplete excision of the cysts [24]. Despite rather short follow-up of our patients neither of them has recurrence of dermoid cyst and are symptom-free.
In conclusion, OSS should be the first choice of surgical management in children with ovarian dermoids not only for avoiding risks for early menapause, premature ovarian failure, impaired sexual growth, low bone density, neurological and cardiac disease in adulthood but also to preserve future fertility of these children. But careful assessment for malignant features and after triaging and selecting appropriate patients meticulous surgical technique via either laparoscopy or open surgery should be performed to avoid rupture of the cyst during surgical intervention. In case of rupture saline irrigation of the abdomino-pelvic cavity should be preferred to avoid future adhesions.
Acknowledgments
None.
Conflict of Interest
None.
References
- Savasi I, Lacy JA, Gerstle JT, Stephens D, Kives S, et al. (2009) Management of ovarian dermoid cysts in the pediatric and adolescent population. J Pediatr Adolsec Gynecol 22: 360-364.
- Berek JS, Natarajan S (2007) Ovarian and Fallopian tube cancer. In: Berek & Novak’s Gynecology. Philadelphia, Lippincott Williams & Wilkins Pg No:1457-1547.
- Depoers C, Martin FA, Nyangoh TK, Morcet J, Proisy M, et al. (2019) A preoperative scoring system for adnexal mass in children and adolescents to preserve their future fertility. J Pediatr Adolsec Gynecol 32: 57-63.
- Renaud EJ, Somme S, Islam S, Cameron DB, Gates RL, et al. (2019) Ovarian masses in the child and adolescent: an American Pediatric Surgical Association outcomes and evidence-based practice commitee systematic review. J Pediatr Surg 54: 369-377.
- Zhang M, Jiang W, Li G, Xu C (2014) Ovarian masses in children and adolescents- an analysis of 521 clinical cases. J Pediatr Adolsec Gynecol 27: e73-e77.
- Luczak J, Baglaj M (2018) Ovarian teratoma in children: A plea for collaborative study. J Ovarian Res 11: 75.
- Martelli H, Patte C (2003) Gonadal tumors in children. Arch Pediatr 10: 246-50.
- Heo SH, Kim JW, Shin SS, Jeong SI, Lim HS, et al. (2014) Review of ovarian tumors in children and adolsecents: Radiologic-pathologic correlation. Radiogr Rev Publ Radiol Soc N Am Inc 34: 2039-2055.
- Outwater EK, Siegelman ES, Hunt JL (2011) Ovarian teratomas: tumor types and imaging characteristics. Radiogr Rev Publ Radiol Soc N Am Inc 21: 475-490.
- Al Jama FE, Al Ghamdi AA, Gasim T, Al Dakhiel SA, Rahman J, et al. (2011) Ovarian tumors in children and adolescents-a clinical study of 52 patients in a university hospital. J Pediatr Adolsec Gynecol 24: 25-28.
- Spinelli C, Pucci V, Strambi S, Piccolo RL, Martin A, et al. (2015) Treatment of ovarian lesions in children and adolescents: a retrospective study of 130 cases. Peadiatr Hematol Oncol 32: 199-206.
- Perera DS, Prabhakar HB (2015) Imaging of the adnexal mass. Clin Obstet Gynecol 58: 28-46.
- Spinelli C, Pucci V, Buti I, Liserre J, Messineo A, et al. (2012) The role of tumor markers in the surgical approach of ovarian masses in pediatric age: a 10-year study and a literature review. Ann Surg Oncol 19: 1766-1773.
- Rivera CM, Grossardt BR, Rhodes DJ, Brown RD, Roger VL, et al. (2009) Increased cardiovascular mortality following early bilateral oophorectomy. Menapause (New York, NY)16: 15.
- Rocca WA, Bower J, Maraganore D, Ahlskog JE, Grossardt BR, et al. (2007) Increased risk of cognitive impairment or dementia in women who underwent oophorectomy before menopause. Neurology 69: 1074-1083.
- Yasui T, Hayashi K, Mizunuma H, Kubota T, Aso T, et al. (2012) Factors associated with premature ovarian failure, early menopause and earlier onset of menopause in Japanese women. Maturitas 72: 249-255.
- Lind T, Holte J, Olofsson JI,Hadziosmanovic N, Gudmundsson J, et al. (2018) Reduced live-birth rates after IVF/ICSI in women with previous unilateral oophorectomy: results of a multicentre cohort study. Hum Reprod 33: 238-247.
- Morgante G, Ditto A, la Marca A, Trotta V, De Leo V (1998) Surgical treatment of ovarian dermoid cysts. Eur J Obstet Gynecol Reprod Biol 81: 47-50.
- Templeman CL, Hertweck SP, Scheetz JP, Perlman SE, Fallat ME (2000) The management of mature cystic teratomas in children and adolescents: a retrospective analysis. Hum Reprod 15: 2669-2672.
- Cohen Z, Shinhar D, Kopernik G, Mares AJ (1996) The laparoscopic approach to uterine adnexal torsion in childhood. J Pediatr Surg 31: 1557-1559.
- Howard FM (1995) Surgical of management of benign cystic teratoma. Laparoscopy vs. laparotomy. J Reprod Med 40: 495-499.
- Lin P, Falcone T, Tulandi T (1995) Excision of ovarian dermoid cyst by laparoscopy and by laparotomy. Am J Obstet Gynecol 173: 769-771.
- Zanetta G, Ferrari L, Mignini-Renzini M, Vignali M, Fadini R (1999) Laparoscopic excision of ovarian dermoid cysts with controlled intraoperative spillage. Safety and effectiveness. J reprod Med 44: 815-820.
- Laberge PY, Levesque S (2006) Short-term morbidity and long-term recurrence rate of ovarian dermoid cysts treated by laparoscopy versus laparotomy. J Obstet Gynaecol Can 28: 789-93.
- Medeiros LRF, Rosa DD, Bozzetti MC, Fachel JMG, Furness S, et al. (2005) Laparoscopy versus laparotomy for benign ovarian tumors. Cochrane Database Syst Rev: CD004751.
- Nitke S, Goldman GA, Fisch B, kaplan B, Ovadia J (1996) The management of dermoid cysts-a comparative study of laparoscopy and laparotomy. Isr J Med Sci 32: 1177-1179.
- Fielder EP, Guzick DS, Guido R, Kanbour-Shakir A, Krasnow JS (1996) Adhesion formation from release of dermoid contents in the peritoneal cavity and effect of copious lavage: a prospective, randomized, blinded, controlled study in a rabbit model. Fertil Steril 65: 852-859.
-
Volkan Sarper Erikci* and Merve Üstün. Ovary-Sparing Surgery for Ovarian Dermoid Cysts in Children: A Report of Two Cases and Literature Review. Anaest & Sur Open Access J. 4(1): 2023. ASOAJ.MS.ID.000578.
-
Surgery, abdominal pain, cyst, analgesic, tumor, inflammation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






