 Case Report
Case Report
Nephrectomy in Children: A Single Center Experience
Chukwubuike Kevin Emeka*, Eze Thaddeus Chikaodili and Anijunsi Livinus Patrick
Department of Surgery, Enugu State University Teaching Hospital, Nigeria
Chukwubuike Kevin Emeka, Department of Surgery, Enugu State University Teaching Hospital, Nigeria.
Received Date: June 16, 2022; Published Date:June 29, 2022
Abstract
Background: The surgical removal of the kidney, nephrectomy, is not a minor surgical procedure. It is a major endeavor. Indications for nephrectomy range from benign to malignant pathological conditions.
Materials and Methods: This was a retrospective study of children aged 15 years and below who had nephrectomy between January 2016 and December 2020 at the pediatric surgery unit of a teaching hospital in Enugu, Nigeria. The information extracted included the age of the patient at presentation, gender, predominant presenting symptom and the pathology (indication), duration of symptoms before presentation to the hospital, time interval between presentation and nephrectomy, operative procedure performed, complications of treatment, duration of hospital stay and outcome of treatment.
Results: Eighteen (18) pediatric nephrectomies were performed during the study period. There were 14 (77.8%) males and 4 (22.2%) females. The mean age of the patients was 6 years with a range of 3 years to 9 years. Nephroblastoma was the most common indication (pathology) for nephrectomy. Nephrectomies were performed more on the left side than on the right. Simple nephrectomy was performed in all the patients. However, children with nephroblastoma had nephroureterectomy. Surgical site infection was the most common post-operative complication. About one-quarter of the patients expired due to tumor metastasis.
Conclusion: Nephrectomy is the optimal procedure for neoplasm of the kidney or non-functional kidney. Malignant kidney tumour (nephroblastoma) was the most common indication for nephrectomy in the present study.
Keywords:Children; Experience; Nephrectomy; Nephroblastoma; Single center
Introduction
The surgical removal of the kidney, nephrectomy, is not a minor surgical procedure. It is a major endeavor. Reasons for nephrectomy could be a spectrum ranging from benign to malignant pathological conditions. On one end of the spectrum is a benign condition such as posterior urethral valve that may cause unilateral kidney damage as in VURD syndrome (posterior urethral valve, unilateral reflux, ipsilateral renal dysplasia). At other end of the spectrum is malignant condition of the kidneys such as nephroblastoma. Recurrent urinary tract infections, hypertension and abdominal pain resulting from non-functional nephroureteral units may be an indication for nephrectomy [1]. The non-malignant pathological conditions that may necessitate nephrectomy in children may include congenital dysplasia, chronic destructive infective processes, chronic obstructive uropathy/nephropathy and severe kidney trauma [2]. Globally, there are variations in the frequency of the indications for nephrectomy in children: These variations are seen in geographical location, age groups and gender [3, 4]. Pediatric urology is dependent on advances in radiographic imaging as the genitourinary tract is internally located and the decision to perform nephrectomy is mainly based on these clinical and radiographic findings [3, 5]. It’s been recognized that pediatric kidney has a remarkable ability to recover its function after reconstructive surgery and this has led to a more conservative approach in the treatment of kidney disorders which may have reduced the incidence of nephrectomy in children [6]. Although nephrectomy is the standard treatment for renal malignancy with a normal contralateral kidney, there is a growing interest in nephron sparing surgery for selected group of children [7, 8]. The aim of this study was to evaluate our experience in the management of children with nephrectomy in terms of indications, complications and treatment outcome.
Materials and Methods
This was a retrospective study of children aged 15 years and below who had nephrectomy between January 2016 and December 2020 at the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) Enugu, Nigeria. Patients who have had nephrectomy at a peripheral hospital before referral to ESUTH for further management were also recruited into study. Patients who are older than 15 years of age were excluded from the study. ESUTH is a tertiary hospital located in Enugu, Southeast Nigeria. The hospital serves the whole of Enugu State, which according to the 2016 estimates of the National Population Commission and Nigerian National Bureau of Statistics, has a population of about 4 million people and a population density of 616.0/km2. The hospital also receives referrals from its neighboring states. Information was extracted from the case notes, operation notes, operation register and admission-discharge records. The information extracted included the age of the patient at presentation, gender, predominant presenting symptom and the pathology (indication), duration of symptoms before presentation to the hospital, time interval between presentation and nephrectomy, operative procedure performed, complications of treatment, duration of hospital stay and outcome of treatment. Indications for nephrectomy were based on clinical, laboratory and imaging parameters. The followup period was 12 months. Ethical approval was obtained from the ethics and research committee of ESUTH. Informed consent from the patients’ caregivers was not required due to the retrospective nature of the study. Statistical Package for Social Science (SPSS) version 21 (manufactured by IBM Corporation Chicago Illinois) was used for data entry and analysis. Data were expressed as percentages, median, mean, and range.
Results
Patients’ demographics
Eighteen (18) pediatric nephrectomies were performed during the study period. There were 14 (77.8%) males and 4 (22.2%) females. The mean age of the patients was 6 years with a range of 3 years to 9 years. The median duration of symptoms prior to presentation to the hospital and the mean duration from presentation to nephrectomy were 8 months and 4 months respectively. The mean duration of hospital stay was 18 days (range: 10-26 days).
Predominant presenting symptom and pathology (indication) involved
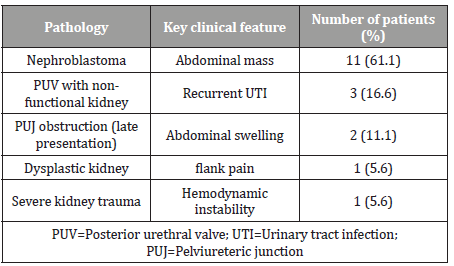
The presenting symptoms depended on the pathology. Table 1 shows the pathology necessitating nephrectomy and their predominant clinical features.
Table 1:Pathology and their clinical features.
Site of the nephrectomy
Left nephrectomy was performed in 10 (55.6%) while 8 (44.4%) patients had right nephrectomy.
Definitive operative procedure performed
All the patients had unilateral simple nephrectomy. However, in patients with nephroblastoma nephroureterectomy was performed.
Complications of treatment
Surgical site infection was reported in 2 (11.1%) patients, one (5.6%) patient each had chest infection and stitch related complications.
Treatment outcome
Thirteen (72.2%) patients achieved full recovery and were discharged home. Five (27.8%) patients expired. All the 5 patients died from malignant tumour recurrence and tumour metastasis.
Discussion
Historically, the first planned nephrectomy on a living human being was performed on August 2, 1869. Eighteen years later in 1887, the first nephrectomy for removal of renal tumor was performed [9]. In ancient times, nephrectomy was performed for renal stones and ureterovaginal fistula. As time went by, nephrectomies were mainly carried out for renal tumors [10]. However, at present the number of nephrectomies has decreased due to the benefits of nephron sparing procedures [10]. In developed countries, current nephrectomies are mostly performed for organ donation and may be significant indication in future [10].
In the present study, there were more nephrectomies in males than in females. Other series on pediatric nephrectomy also reported this male predominance [2, 11]. However, other studies documented more nephrectomies in females [7, 12]. The exact reason for the gender disparity is not known. One study from Enugu, Nigeria reported that non-malignant indications for nephrectomy were more in females [2]. Our patients’ mean age of 6 years is consistent with the report of Bouhafs et al. but at variance with the report of Sammond et al. [13, 14]. The different indications for nephrectomies in the patients may determine the mean age of the patients. For instance, Ekenze et al. reported that the age range for children who had nephrectomy for nephroblastoma was 2 years to 5 years [15]. The median duration of symptoms prior to presentation to the hospital of 8 months may be attributed to the high level of poverty and low level of parental awareness found in low-income countries. Time was required for detailed evaluation, investigation and optimization of the patients. This explains the 4 months interval between presentation and surgery (nephrectomy). Howbeit, in severe kidney trauma with hemodynamic instability, nephrectomy was performed as an emergency. The duration of hospitalization of the patients was dependent on the indications for the nephrectomy and the post-operative course.
Nephroblastoma was the most common indication for nephrectomy in the index study and these nephroblastoma presented as painless abdominal masses. A similar study on pediatric nephrectomy also reported nephroblastoma as the most common indication for nephrectomy [2]. Nephroblastoma is an embryonal type of renal cancer and is one of the most common solid malignant neoplasms in children [16]. One study from Saudi Arabia, however, reported non-functioning kidney from vesicoureteric reflux as the most common indication for nephrectomy [11]. The reason for this finding is difficult to explain but the cohort of patients recruited into the different studies may explain it. Unlike in pediatric population, in adults, non-malignant indications are the most common indications [17]. Among the non-malignant indications in the present study, posterior urethral valve accounted for most indications. Posterior urethral valve is a persistent membrane of the urethra, which causes obstruction in the urogenital tract in males [18]. It is the most common cause of bladder outlet obstruction and renal insufficiency in male children. The finding of posterior urethral valve as the most common benign indication for nephrectomy is at variance with the report of other researchers [1, 11]. Late presentation of children who have posterior urethral valve, with the consequential pathologies may explain this high incidence.
In the index study, more left nephrectomies were performed. This is in line with the report of a study from southeastern Nigeria [2]. However, Menon et al. reported equal number of nephrectomies on the right amd left sides [1]. Alhaidari et al. reported bilateral nephrectomy in a single patient [11]. The location of the pathology determines the site where nephrectomy is performed. Simple nephrectomy was performed in the patients. Only children with nephroblastoma had nephroureterectomy. Other studies also reported simple nephrectomies [2, 11]. In renal neoplasm, radical nephrectomy may also be performed [11]. Partial and nephron sparing nephrectomy was not performed in any of the patients: The fact that the pathologies were not bilateral in any of the patients may be responsible for this.
Surgical site infection was the most common post-operative complication. Other authors also documented wound infections following nephrectomy [19]. Even in minimal access surgeries for nephrectomy, surgical site infection has been reported [20]. Overall, the outcome of nephrectomy is good. Mortalities seen in the present study resulted from malignant kidney tumours due to recurrence and metastasis. Delayed presentation of the patients with attendant tumor spread may be responsible.
Conclusion
Nephrectomy is the optimal procedure for neoplasm of the kidney or non-functional kidney. Malignant kidney tumour (nephroblastoma) was the most common indication in the present study. Future studies will evaluate the predictive factors that influence the outcome of nephrectomy in children.
Conflict of Interest
None.
Acknowledgements
None.
References
- Menon P, Handu AT, Rao KL, Arora S (2014) Laparoscopic nephrectomy in children for behign conditions: indications and outcome. J Ihdian Assoc Pediatr Surg 19(1): 22-27.
- Ezomike UO, Modekwe VI, Ekenxe SO (2018) Paediatric nephrectomy: Patterns, indications and outcome in a developing country. Malawi Med J 30(2): 94-98.
- Daradika T (2012) Indications for nephrectomy in children: A report of 119 cases. Saudi J Kidney Dis Transpl 23(6): 1221-1229.
- 4. Eke N, Echem RC (2003) Nephrectomy at the University of Port Harcourt Teaching Hospital: a ten-year experience. Afr J Med Med Sci 32(2): 173-177.
- Wagna M, Mayr J, Hacker FM (2008) Improvement of split function in hydronephrosis with less than 10% function. Eur J Pediatr Surg 18(3): 156-159.
- Diniz G (1985) A regional panorama of non-tumoral nephrectomy reasons in childhood. Turk Patholo 1(1): 90-97.
- Rafique M (2007) Nephrectomy: Indications, Complications and mortality in 154 consecutive patients. J Pak Med Assoc 57(6): 308-311.
- Ehrlich PF, Shanberg AM, Asch MJ, Kogan B, Kaplan L (1986) Bilateral Nephrectomy for Wilms’ Tumor. The Journal of Urology 136(1): 308-311.
- Herr HW (2008) Surgical management of renal tumors: a historical perspective. Urol Clin North Am 35(4): 543-549.
- Poletajew S, Antoniewicz AA, Borowka A (2010) Kidney removal: the past, presence, and perspectives: a historical review. Urol J (4): 215-223.
- Alhaidari OI, Moazin MS, Alhussein RM, Alghaith AA, Almoaiqelm FA, et al. (2019) Indications for pediatric nephrectomy: a retrospective hospital-based study on Saudi population. International Journal of Medicine in Developing Countries 3(4): 348-352.
- Hamilton BD, Gatti JM, Cartwright PC, Snow BW (2000) Comparison of laparoscopic versus open nephrectomy in the pediatric population. I Urol 163(3): 937-939.
- Bouhafs A, Dendane A, Azzouzi D, Belkacem R, Barahioui M (2001) Total nephrectomy in children: 11 years of experience in 80 cases. Ann Urol 37(2): 43-46.
- Sammon JD, Zhu G, Sood A, Sukumar S, Kim SP, et al. (2014) Pediatric nephrectomy: Incidence, Indications and use of minimally invasive techniques. The Journal of Urology 191(3): 764-770.
- Ekenze SO, Agugua-Obianyo NE, Odetunde OA (2006) The challenges of nephroblastoma in a developing country. Ann Oncol 17(10): 1598-1600.
- Szychot E Apps J, Pritchard-Jones K (2014) Wilms’ tumor: biology, diagnosis and treatment. Transl Pediatr 3(1): 12-24.
- Takagi T Mir MC, Sharma N (2014) Compensatory hypertrophy after partial and radical nephrectomy in adults. J Urol 192: 1612-1618.
- Pakkasjarvi N, Holtta V, Heikkila J, Taskinen S (2021) Posterior urethral valve and the risk of neurodevelopmental disorders in two FINNISH cohorts. J Pediatr Urol 17(4): 514.e1-514.e5
- Kohlberg WI, Tellis VA, Bhat DJ (1980) Wound infection after transplant nephrectomy. Arch Surg 115(5): 645-646.
- De Vermandois JAR, Cochetti G, Zingaro MD, Santoro A, Panciarola M, et al. (2019) Evaluation of surgical site infection in mini-invasive urological surgery. Open Med 15(14): 711-718.
-
Chukwubuike Kevin Emeka, Eze Thaddeus Chikaodili, Anijunsi Livinus Patrick. Nephrectomy in Children: A Single Center Experience. Anaest & Sur Open Access J. 3(3): 2022. ASOAJ.MS.ID.000564.
-
Pathology, Trauma, Renal tumor, Surgery, Congenital dysplasia, Chronic destructive.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






