 Research Article
Research Article
Improving Surgical Antibiotic Prophylaxis Compliance in Adults and Children Undergoing Surgery: a Quality Improvement Study
Mushira Enani1*, Fe Cobaldez Faustino1, Mahmoud Mukahal2, Mercy Evangelista3, Zubeda Mohammed4, Sharon Naidoo2, Shahed AlOtaiby5,Humariya Heena5,Mohammed Ibrahim3, Adnan AlMaghlouth5,6 and Ibrahim Nasir3
1Department of Medicine, Infectious Disease, Kingdom of Saudi Arabia
2Infection Control Administration, King Fahad Medical City, Kingdom of Saudi Arabia
3Department of Clinical Audit, King Fahad Medical City, Kingdom of Saudi Arabia
4Department of Quality Management, King Fahad Medical City, Kingdom of Saudi Arabia
5Research Center, King Fahad Medical City, Kingdom of Saudi Arabia
6Periodontics section, Dentistry Administration, King Fahad Medical City, Kingdom of Saudi Arabia
Mushira Enani, Department of Medicine, Infectious Disease, King Fahad Medical City, Riyadh, Kingdom of Saudi Arabia.
Received Date: February 22, 2021; Published Date:May 03, 2021
Abstract
Background: Surgical Antibiotic Prophylaxis (SAP) is the standard of care worldwide to prevent postoperative surgical site infection (SSI) and to minimize the risk of antibiotic‐related adverse events including but not limited to clostridium difficile-associated diarrhea and selective pressure leading to antibiotic resistance as a result of prolonged prophylaxis exceeding 24 hours. Overuse, under‐use, improper timing, and misuse of antibiotics occur in 25–50% of operations. This study aimed to develop a group of interventions that could be used to improve SAP at a tertiary care healthcare institute in Riyadh, Kingdom of Saudi Arabia (KSA).
Methods: A pre-post longitudinal quality improvement project was conducted from January 2016 until December 2019. A multidisciplinary team was assembled to identify and overcome the barriers that were responsible for patients receiving suboptimal antibiotic prophylaxis. Multiple educational campaigns and an open forum with anesthesia, surgical, nursing, and operating room staff were organized. Only the patients that had undergone surgery requiring SAP were included. Compliance with an appropriate antibiotic selection, timing, dosing, and duration was measured and year wise comparison was made.
Results: One reference quarter results from each year from 2017-2019 were used for final analysis. Five hundred surgical case files from 2017, 186 from 2018, and 229 from 2019 were reviewed. The cefazolin dose adjustment based on BMI was done only for 32, 13, 25% of the patients over consecutive years respectively. However, weight-based dosage showed improvement from 2017-2019 (70-75 %). All patients (100%) received antibiotic prophylaxis with average compliance of 89% for appropriate antibiotic selection, 95% for proper timing, 71% of patients received weightbased dosage as per guidelines, and only 68% discontinued prophylaxis within 24 hours of the surgery end time.
Conclusion: Our multidisciplinary quality improvement initiative successfully improved compliance to key performance indicators of surgical antibiotic prophylaxis for patients undergoing surgery requiring SAP.
Abbrevations:SAP: Surgical Antibiotic Prophylaxis; SSI: Surgical Site Infection; SSIs: Surgical Site Infections; KFMC: King Fahad Medical City; BMI: Body Mass Index; MH: Main Hospital; KSHC: King Salman Heart Center; CSH: Children Specialized Hospital; NNI: National Neuroscience Institute; WSH: Women Specialized Hospital
Background
Surgical Site Infection ranks second common among healthcareassociated infections. Systemic antibiotics administered before the surgical incision for a selected type of surgery is an important preventive strategy to reduce the incidence of surgical site infections (SSIs) and is known as surgical antibiotic prophylaxis (SAP) [1]. SAP has revolutionized the health care system by decreasing the mortality and morbidity rates for patients undergoing various types of surgeries [2]. In addition, SAP plays a major role in reducing hospital stay, the financial burden of health care cost, resulting in improved patient satisfaction and outcomes [2]. Surgical antibiotic prophylaxis has proved its effectiveness for surgical procedures as per several published studies [3-4]. A specific set of criteria should be met for using appropriate antibiotics in patients to reduce SSI; prescribing the right antibiotic choice with optimal dosage at the right time for the shortest effective duration [1-8]. The WHO recommendations were developed with a global perspective and they take into account the balance between benefits and harms, the evidence quality level, cost and resource use implications, and patient values and preferences [4].
Most of the studies stress administering the preventive antibiotic closely before the incision time, while several others disagree and urge the antibiotic administration to be slightly earlier to provide effective prevention against SSI [9-13]. On the other hand, a large randomized controlled clinical trial conducted in Switzerland could not reveal the ideal preoperative timing of SAP administration [14]. Recently, the Centers for Disease Control and Prevention updated evidence-based recommendations for the prevention of SSI among different types of surgeries for better patient safety [15].
This study aimed to demonstrate performance improvement in SAP in terms of selection, dosing, timing, and duration of prophylaxis in patients undergoing surgery.
Methods
Patients who underwent surgery and required SAP, between Jan 2016- Dec 2018 at tertiary care hospital in Riyadh, KSA were included in the study. An interdisciplinary team was created for better patient safety among patients undergoing different surgical procedures after identifying a gap in clinical practice in the hospital. Under infectious diseases, specialist leadership, physicians, nurses, and quality improvement staff, and subsequently surgeons came together and identified an opportunity to improve practice through optimizing the choice, timing, dosing, and duration of preoperative SAP.
This study was carried out in 3 hospitals and two centers that cater to surgical procedures in our institution. Five hundred surgical case files in 2017 (from two-quarter reports), 186 in 2018 (one-quarter report), and 229 (one-quarter report) that required antimicrobial prophylaxis were studied for the whole period of the audit by reviewing medical, anesthesiologist, and nursing records, along with medication administration charts. They administered antibiotics were compared to hospital guidelines on SSI prevention using the following audit measures: Selection of the type of the antibiotic prophylaxis as per guideline; weight-based dosage as per guideline and the adjustment of cefazolin to 3 grams in obese patients with body mass index (BMI)>35; timing of giving the antimicrobial prophylaxis (within 60 minutes before the incision); discontinuation of prophylaxis within 24 hours; and re-dosing of SAP in cases of prolonged procedures (more than 4 hours) or massive blood loss (more than 1.5 liters).
Data were presented as number (percentage) and p-value < 0.05 was considered significant. The Institutional Review Board approved this study at King Fahad medical city (KFMC), Riyadh, KSA.
Results
After reviewing the files over three years, the percentage compliance showed improvement in the right choice of SAP from 89% to 93%. However, there remains room for improving compliance with a dose adjustment of cefazolin (32, 13, 25 in 2017, 2018, 2019) and timing of antibiotic prophylaxis (95, 89, 91 in 2017, 2018, 2019) Figure 1 and Table 1. Re-dosing in case of prolonged procedures was improved from 80% compliance to 92 % in 2019 (Figure 1,2 &Table 1).
Table 1:Baseline compliance with SAP key performance indicators: proper selection, timing, dosage, and duration (2017).

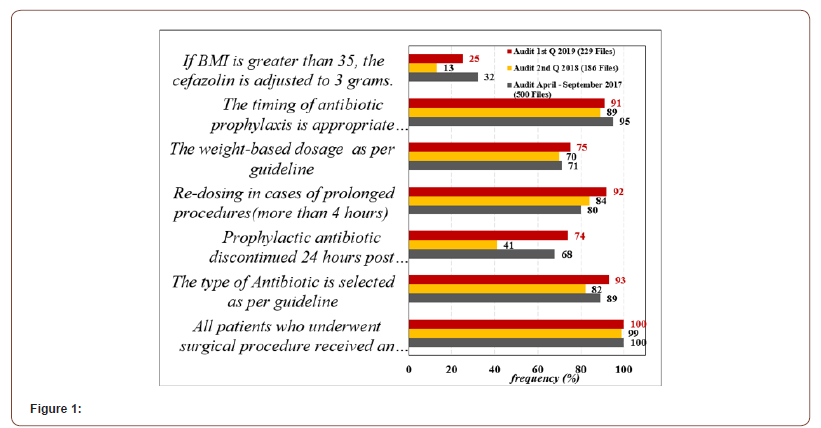
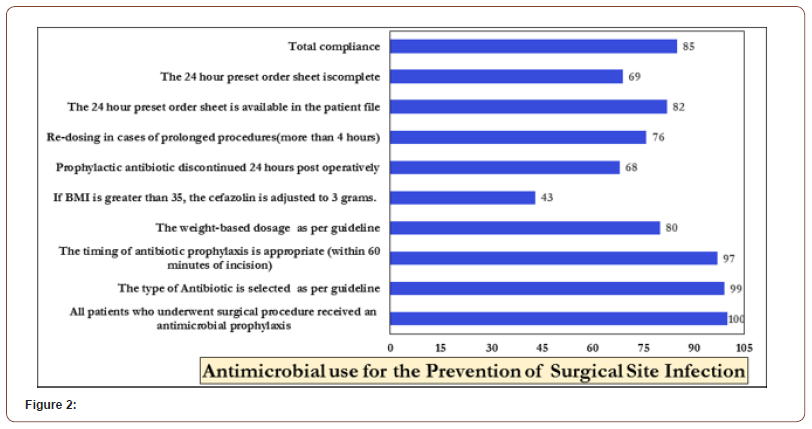
Table 1 shows compliance with SAP key performance indicators: proper selection, timing, dosage, and duration as per specialty in our hospital. Of the 500 cases that underwent surgery in 2017, 260 patient files were reviewed for general surgical specialties and 60 each for other specialties (Cardiac, neurosurgery, pediatric, and obstetrics, and gynecology). The least compliance was towards prophylactic antibiotic being discontinued 24 hours after surgery end time and weight-based dosage as per guideline (55% and 66% respectively) while among non-surgical specialties the compliance percentage was slightly higher. The overall dose adjustment of cefazolin to 3 grams in all surgical patients was 32% (25/78 patients). Table 2. Of the 500 reviewed cases that underwent surgery, 125 surgeries were prolonged for more than 4 hours, only in 100 (80%) patients, antibiotic prophylaxis was re-administered every 4 hours Table 3-5.
Table 2:Adjustment of SAP when BMI > 35 (2017).

Table 3:Re-dosing of SAP (2017).

Table 4:SAP Key Performance Indicators per Surgical Specialty.

Table 5:

Table 2 depicts the adjustment of SAP as per BMI. Only 33% of the records showed compliance with this parameter in all surgical specialties. Table 3 shows re-dosing of SAP in cases of prolonged procedures, re-dosing was compiled to 74% in MH surgical specialties while it was 78% was a cardiac specialty.
The above table shows compliance for surgical specialties. Urologic surgery showed the lowest compliance inappropriate antibiotic selection (28%) and weight-based dosage compliance (37%). The least KPI compliance overall was for cefazolin dose adjustment for high BMI.
Discussion
This study showed remarkable improvement in the right choice of SAP and compliance with appropriate timing achieved over the years through various improvement initiatives. However, there is still room to improve compliance and dose adjustment as per BMI. Effective communication between doctors, nurses, anesthesia staff, infection control, and clinical auditing team can result in behavioral change toward applying best practices in process KPIs related to SAP to reduce or prevent SSI.
This quality improvement study revealed that there was poor adherence to the surgical prophylaxis guidelines in the pre-intervention phase. This lack of adherence was attributed mainly to the absence of comprehensive institutional guidelines and a lack of awareness about the best practices related to SAP. Remarkable compliance with SAP was noted in the current study after the implementation of a quality improvement project by the hospital multidisciplinary team. The initiation of hospital-wide comprehensive guidelines and several educational sessions played a significant role in the improved compliance observed in the post-intervention phase. This may have been due to the presence of explicit instructions that outlined the appropriate antibiotics for common surgeries, along with increased knowledge among physicians and surgeons regarding institutional policies and procedures regarding the appropriate antibiotic choice, timing, dose, and duration. Previous studies using SAP for varied surgical procedures such as orthopedic, cardiac, and gastrointestinal highlighted the efficiency of teamwork with a defined role to enhance SAP compliance [16-25].
These pre-intervention findings are consistent with those reported by other studies at both local and international levels [26- 32]. A multidisciplinary quality improvement project in the current study, particularly with regards to the appropriateness and timing of antibiotic prophylaxis improved adherence to surgical prophylaxis guidelines by surgical staff which is reflected in the compliance percentage improvement over the years. The implementation of institutional policy and procedures for surgical prophylaxis and simplifying it in a comprehensive protocol plays a significant role in guiding surgeons to use the most appropriate antibiotic choice and dose based on evidence-based recommendations. These guidelines should be tailored to the needs of each institution based on the most common types of surgeries performed and the antibiotics available. In a study conducted by Willemsen et al., a standardized, comprehensive protocol for antibiotic prophylaxis was linked with enhancement in antibiotic dosing and timing [33].
Furthermore, Ozgun et al. demonstrated that education is essential to promote evidence-based practice, but insufficient alone to change the practice. The educational intervention resulted in the improvement of indications, choice, and dosage of surgical antimicrobial prophylaxis but not in improving prophylaxis or total compliance rate. The researchers recommended educational interventions within protocols and guidelines to improve overall adherence [34].
In the current study, the authors believe that strict implementation of SAP pre-printed order set will assist in reducing variation in the process and maintain the highest possible compliance. Continuous audit and feedback to prescribers with benchmarking among surgeons may further improve lowperforming surgeons.
Effective communication between doctors, nurses, anesthesia staff, Infection control, and clinical auditing team can result in behavioral change toward improving adherence to best practice processes related to SAP to achieve the goal of SSI prevention. In a recent study, the presence of a pharmacist in a surgical department was associated with a decrease in the number of patients receiving prophylactic antibiotics without justifiable indications, a reduction in the rate of prolonged duration of prophylaxis, and an increase in the number of patients receiving correct antibiotics [35]. A future direction towards such a measure will also prevent the overuse of antibiotics when not needed. Adoption of a comprehensive approach and continuous evaluation of that approach aiming to improve adherence to antimicrobial prophylaxis guidelines in Saudi Arabia at all major hospitals will improve health care and cut costs related to surgical procedures. Future studies are recommended to explore the effect of adherence to antimicrobial prophylaxis on the rate of postoperative surgical infections.
Conclusion
A multidisciplinary quality improvement intervention and implementation of a comprehensive institutional policy and procedures led to an improvement in the proper choice of antibiotic and timing of the antibiotic prophylaxis. The results of this study suggest that a focused multidisciplinary intervention can enhance adherence to institutional surgical antimicrobial prophylaxis guidelines and protocols.
Declarations
Ethics approval and consent to participate Ethics approval was obtained from the Institutional Review Board at King Fahad Medical City, Riyadh. The manuscript does not report on or involve the use of any animal or human data or tissue.
Consent to publish
Not applicable.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the policy of confidentiality from the institution but are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable
Authors’ Contributions
M E, I N, and MI generated the research question and protocol of the study, analyzed and interpreted the patient data. F F, M E, M M, Z M, S N performed the data collection, entry, and analysis. SA, HH has contributed to writing the manuscript, AA reviewed the final draft, M E edited the final draft. All authors read and approved the final manuscript.
Acknowledgments
We acknowledge Research Center at King Fahad Medical City for their writing services.
References
- Munckhof W (2005) Antibiotics for surgical prophylaxis. Aust Prescr 28: 38-40.
- Australian Commission on Safety and Quality in Health Care (2012) Healthcare associated infection action guide. In: ACSQHC, editor. Sydney: Australian Commission for Safety and Quality in Health Care.
- Antibiotic Expert Groups (2014) Therapeutic guidelines: antibiotic. 15. Melbourne: Therapeutic Guidelines Limited, Australia.
- Allegranzi B, Bischoff P, de Jonge S, Kubilay N, Zayed B, et al. (2016) New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 12: e276e87.
- Scottish Intercollegiate Guidelines Network (2014) Antibiotic prophylaxis in surgery. In: Healthcare Improvement Scotland, editor, Edinburgh, UK.
- Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, et al. (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 70(3): 195-283.
- Berrı´os-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8): 784-791.
- National Institute for Health and Clinical Excellence (2008) Surgical site infections: prevention and treatment clinical guideline. Excellence NIfHaC, editor. UK: National Institute for Health and Clinical Excellence.
- Gower EW, Lindsley K, Tulenko SE, Nanji AA, Leyngold I, et al. (2017) Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst Rev: 2.
- Voigt J, Mosier M, Darouiche R (2015) Systematic review and meta-analysis of randomized controlled trials of antibiotics and antiseptics for preventing infection in people receiving primary total hip and knee prostheses. Antimicrob Agents Chemother 59(11): 6696-6707.
- Weber WP, Mujagic E, ZwahlenM, Marcel Bundi, Henry Hoffmann, et al. (2017) Timing of surgical antimicrobial prophylaxis: A phase 3 randomised controlled trial. The Lancet Infectious Diseases 17(6): 605-614.
- de Jonge S, Gans S, Atema J, Joseph S Solomkin, Patchen E Dellinger, et al. (2017) Timing of preoperative antibiotic prophylaxis in 54,552 patients and the risk of surgical site infection. Medicine (Baltimore) 96(29): e6903.
- Weber WP, Marti WR, Zwahlen M, Heidi Misteli, Rachel Rosenthal, et al. (2008) The timing of surgical antimicrobial prophylaxis. Ann Surg 247(6): 918-926.
- Steinberg JP, Braun BI, Hellinger WC, Linda Kusek, Michele R Bozikis, et al. (2009) Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann Surg 250(1): 10-16.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, Brian Leas, Erin C, et al. (2017) Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg 152(8): 784-791.
- AlBuhairan B, Hind D, Hutchinson A (2008) Antibiotic prophylaxis for wound infections in total joint arthroplasty: a systematic review. J Bone Joint Surg Br 90(7): 915-919.
- Slobogean GP, Kennedy SA, Davidson D, O’Brien PJ (2008) Singleversus multiple-dose antibiotic prophylaxis in the surgical treatment of closed fractures: a meta-analysis. J Orthop Trauma 22(4): 264-269.
- Southwell-Keely JP, Russo RR, March L, Cumming R, Cameron I, et al. (2004) Antibiotic prophylaxis in hip fracture surgery: a meta-analysis. Clin OrthopRelat Res 1(419):179-184.
- Barker FG (2002) Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. Neurosurgery 51(2): 391-401.
- Saleh A, Khanna A, Chagin KM, Klika AK, Johnston D, et al. (2015) Glycopeptides versus b-Lactams for the prevention of surgical site infections in cardiovascular and orthopedic surgery: a meta-analysis. Ann Surg 261(1): 72-80.
- Lador A, Nasir H, Mansur N, Sharoni E, Biderman P, et al. (2012) Antibiotic prophylaxis in cardiac surgery: systematic review and meta-analysis. J Antimicrob Chemother 67(3): 541-550.
- Mertz D, Johnstone J, Loeb M (2011) Does duration of perioperative antibiotic prophylaxis matter in cardiac surgery? A systematic review and meta-analysis. Ann Surg 254(1): 48-54.
- Darouiche R, Mosier M, Voigt J (2012) Antibiotics and antiseptics to prevent infection in cardiac rhythm management device implantation surgery. Pacing Clin Electrophysiol 35(11): 1348-1360.
- Daskalakis K, Juhlin C, Pa˚hlman L (2014) The use of pre- or postoperative antibiotics in surgery for appendicitis: a systematic review. Scand J Surg 103(1): 14-20.
- Nelson RL, Gladman E, Barbateskovic M (2014) Antimicrobial prophylaxis for colorectal surgery. Cochrane Database Syst Rev: 5.
- Liang B, Dai M, Zou Z (2016) Safety and efficacy of antibiotic prophylaxis in patients undergoing elective laparoscopic cholecystectomy: a systematic review and meta-analysis. J Gastroenterol Hepatol 31(5): 921-928.
- Meijer W, Schmitz P, Jeekel J (1990) Meta-analysis of randomized, controlled clinical trials of antibiotic prophylaxis in biliary tract surgery. Br J Surg 77(3): 283-290.
- de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, et al. (2009) Surgical site infection: Incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37: 387-397.
- Weber WP, Zwahlen M, Reck S, Feder-Mengus C, Misteli H, et al. (2008) Economic burden of surgical site infections at a European university hospital. Infect Control Hosp Epidemiol 29: 623-629.
- Anderson DJ (2011) Surgical site infections. Infect Dis Clin North Am 25: 135-153.
- Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ (2002) The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: Adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 23: 183-189.
- Goede WJ, Lovely JK, Thompson RL, Cima RR (2013) Assessment of prophylactic antibiotic use in patients with surgical site infections. Hosp Pharm 48: 560–567.
- Willemsen I, van den Broek R, Bijsterveldt T, van Hattum P, Winters M, et al. (2007) A standardized protocol for perioperative antibiotic prophylaxis is associated with improvement of timing and reduction of costs. J Hosp Infect 67: 156-160.
- Ozgun H, Ertugrul BM, Soyder A, Ozturk B, Aydemir M (2010) Perioperative antibiotic prophylaxis: Adherence to guidelines and effects of educational intervention. Int J Surg 8: 159-163.
- Zhang HX, Li X, Huo HQ, Liang P, Zhang JP, et al. (2014) Pharmacist interventions for prophylactic antibiotic use in urological in patients undergoing clean or clean-contaminated operations in a Chinese hospital. PLoS One 9(2): e88971.
-
Mushira Enani, Fe Cobaldez Faustino, Mahmoud Mukahal,Mercy Evangelista. Improving Surgical Antibiotic Prophylaxis Compliance in Adults and Children Undergoing Surgery: a Quality Improvement Study. Anaest & Sur Open Access J. 2(4): 2020. ASOAJ. MS.ID.000544.
-
Surgical Antibiotic Prophylaxis (SAP), antibiotics, Healthcare, Surgery
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






