 Case Report
Case Report
Hemodynamic Pattern by Swan-Ganz Catheter in Patients with Septic Shock Due to Severe Sars-Cov-2- Related Pneumonia: Case Report
Edgar Xavier Martínez Guerrero1*, Felipe de Jesús Montelongo2 , Giovanni Morales Sánchez1, Luis Eduardo Segura Medina1, Jonathan Galindo Ayala1, Rafael Tapia Velasco1, María Magdalena Reyes Pérez1, Blanca Estela Herrera Morales3, Viviana Román Simón1, Jesús Román Sanvicente Sánchez1, Laura Livia Alarcón Sánchez1, Wenceslao Medrano Espinosa1 and Aurea Carmona Domínguez1
1Medical Specialist in Critical Care, attending physician in the Neurointensive and Intensive Care Unit, Hospital General “Las Américas,” Instituto de Salud del Estado de México, Mexico
2Critical Care Specialist, Chief and Professor of the Critical Care Specialty, Hospital General “Las Américas,” Instituto de Salud del Estado de México, Mexico
3MS in Clinical Research, Health Education and Research Coordinator, HGZ 196, IMSS, México
Edgar Xavier Martínez Guerrero, Medical Specialist in Critical Care, Instituto de Salud del Estado de México, Mexico.
Received Date: January 26, 2022; Published Date:February 09, 2022
Abstract
the end of 2019, a new species of coronavirus spread rapidly in Hubei, China, where several patients presented pneumonia of unknown origin. This infectious outbreak caused an epidemic in China that grew rapidly evolving into a pandemic. Consequently, in February 2020, the World Health Organization named Coronavirus Disease 2019 (COVID-19) to the disease caused by the SARS-CoV-2 virus. During the evolution of COVID-19 to a severe disease, hemodynamic deterioration sometimes occurs with the development of a sepsis-induced shock state. Therefore, hemodynamic monitoring is highly important during the diagnosis and treatment of critically ill patients with multisystem dysfunction. Until now, hemodynamic monitoring in patients with severe COVID-19 has not been described in the literature using the gold standard, which is the Swan-Ganz (SG) catheter. For this reason, we consider this description of the utmost importance.
Keywords:COVID-19; Swan-Ganz catheter; Pneumonia; Hemodynamics
Introduction
At the onset of the disease, symptoms such as fever, cough, general malaise, and myalgia are present; however, the disease can evolve to cause organic dysfunction characterized mainly by acute respiratory distress syndrome, myocardial and renal injury, and death. During the evolution of severe COVID-19, shock status is associated with sepsis, so cardiovascular monitoring is important since, in selected cases, an invasive approach through the SGtype pulmonary artery catheter is imperative to know their true hemodynamic status [1-3]. In 1970, the SG catheter was introduced as a diagnostic tool that can be used at the patient’s bedside and its use spread worldwide in intensive care units; it provides hemodynamic data of the pulmonary intravascular territory and the right ventricle with greater diagnostic sensitivity than clinical data or non-invasive methods. Likewise, it presents greater precision in estimating preload than central venous pressure in patients with ventricular systolic dysfunction. All these data plus the constant assessment and point-of-care decision-making of the critically ill patient positively influence treatment [4-6].
Clinical Cases
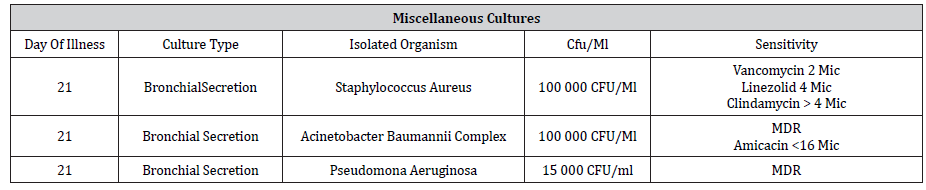
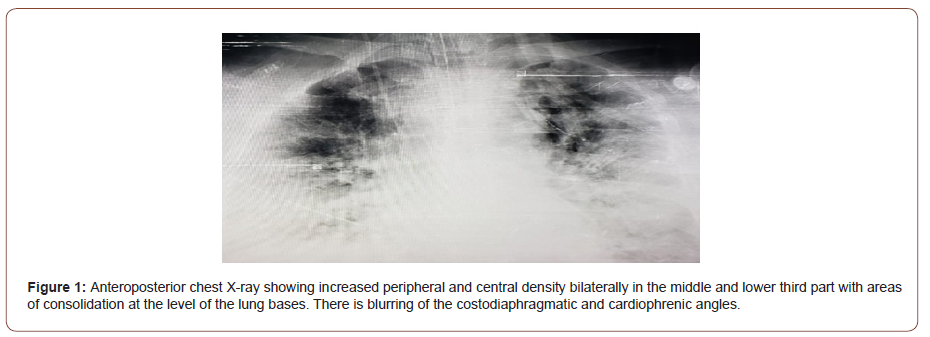
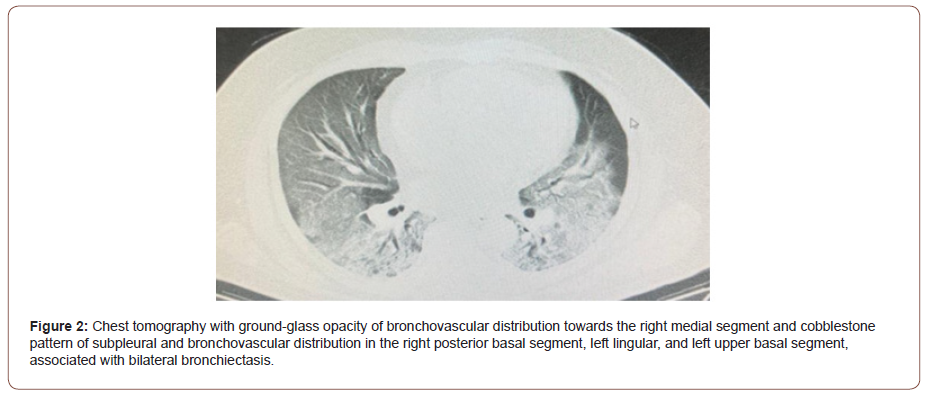
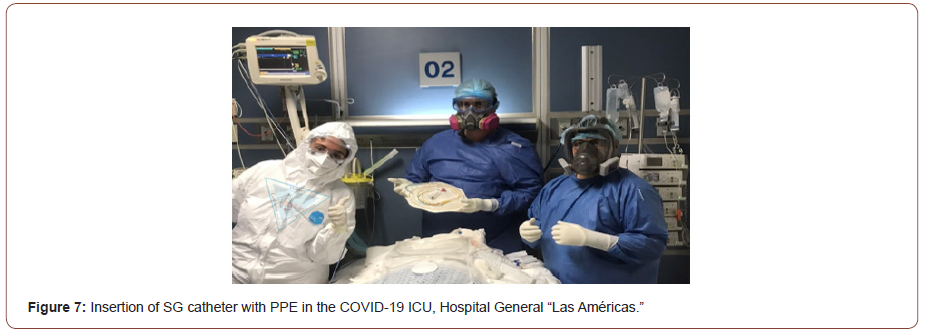
Patient 1: A 68-year-old male with a chronic degenerative history of type 2 diabetes mellitus (6 years in treatment with metformin/glibenclamide) and systemic arterial hypertension (5- year diagnosis in treatment with captopril), in regular metabolic control. On day 1 of the disease, he presented asthenia, adynamia, fever, and cough with expectoration, for which he consulted a private physician who started treatment based on ciprofloxacin, ambroxol, salbutamol, ipratropium bromide, and acetaminophen, with no improvement. On day 11, medium-effort dyspnea and a up to 60% saturation by pulse oximetry occurred, so he went to the Emergency Department of the Hospital General de Ecatepec “Las Américas” of the Health Institute of the State of Mexico (ISEM). There, chest X-ray (Rx) and chest Tomography (TACT) were taken (Figure1 and Figure 2) and he was directly admitted to the Intensive Care Unit (ICU). Later, he had a positive result for COVID-19 by PCR on day 17. Upon admission to the ICU with no vasopressor support and the presence of elevated glycemia, acute renal injury (*), heart rate (HR) of 122 beats per minute, blood pressure (BP) of 124/72 mmHg, respiratory rate (RR) of 22 r/min, non-invasive ventilatory management with continuous positive airway pressure (CPAP) was initiated. In addition to the onset of prone decubital position, with a Roth score of 5 seconds, a ROX index of 5, and progressive deterioration of respiratory function, orotracheal intubation, and mechanical ventilatory support are performed at day 13, and initiation of sedation with RASS scale of -5, with initial static compliance of 38 ml/cmH2O, in volumecontrolled mode with FIO2 of 50%, current volume (Vt) 490 ml, FR 29 x min, PEEP of 10 cmH20, with the presence of peak pressure of 27 cm/H20, plateau pressure of 25 cm/H2O, driving pressure (DP) of 15 cm/H2O, mechanical power (PM) of 27 j/min, static compliance of 33 ml/cmH2O, with a PAFI index of 112 mmHg and a saturation of 91%. The patient presented febrile peaks of up to 38.5 °C on day 17, with the development of septic shock, for which norepinephrine was started at 0.1 ug/kg/min. In addition, antibiotic therapy was started, and cultures were taken. An SG catheter with a hemostasis introducer (IH) is placed on day 19, after putting personal protective equipment (PPE) and performing the asepsis and antisepsis protocol [7], thus obtaining an initial hemodynamic pattern of sepsis-induced distributive shock in a hyperdynamic state with no cardiac depression and low pulmonary arterial wedge pressure (PAWP), so adjustments in fluid and vasopressor therapy are made. Subsequently, the patient shows a mixed-shock (septic and cardiogenic) state with low cardiac output (CO) and low cardiac index (CI) in his hemodynamic pattern, which places him in group II of the Frank-Starling curve of moderate cardiac depression with a drop in the left ventricular stroke work index (LVSWI), which justified the initiation of dobutamine inotropic therapy, as well as impaired oxygen supply (O2RI) and oxygen consumption (VO2I) with a tendency to a hypodynamic phase (Table 1, Figure 3). In this way, an infection due to multidrug-resistant (MDR) ventilatorassociated pneumonia (VAP) is confirmed (Table 2). Antibiotic therapy was adjusted according to sensitivity, with continuous deterioration of ventilatory status and refractory septic shock with no response to fluids and vasopressors. He died on day 21.
Table 1:SG hemodynamic parameters.
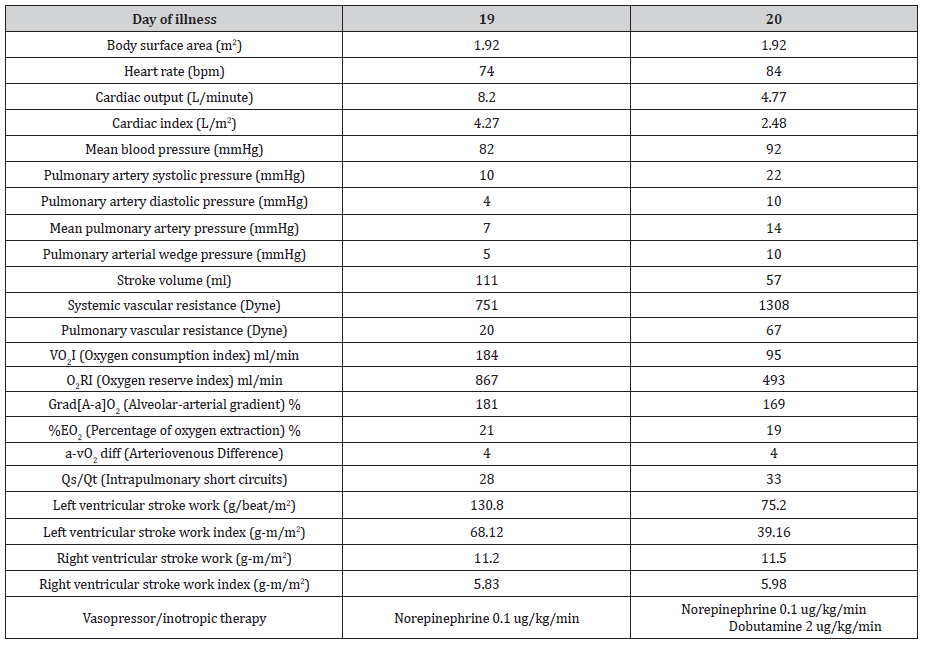
Table 2:Results of diverse cultures.
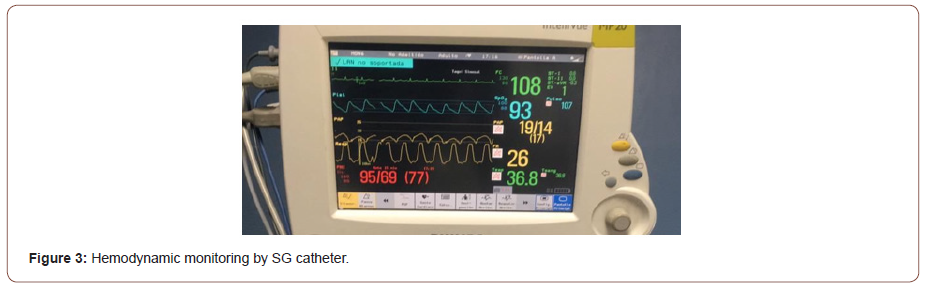
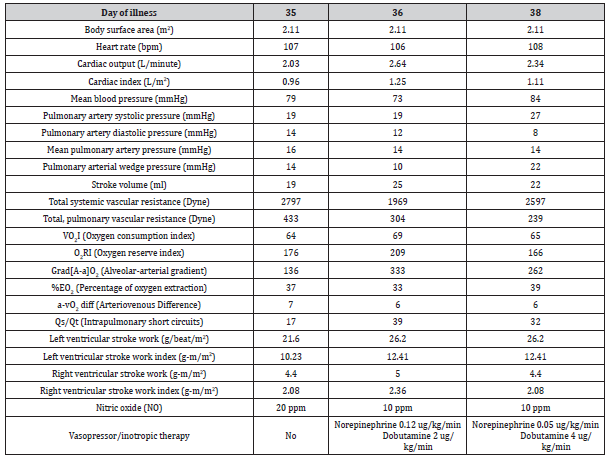
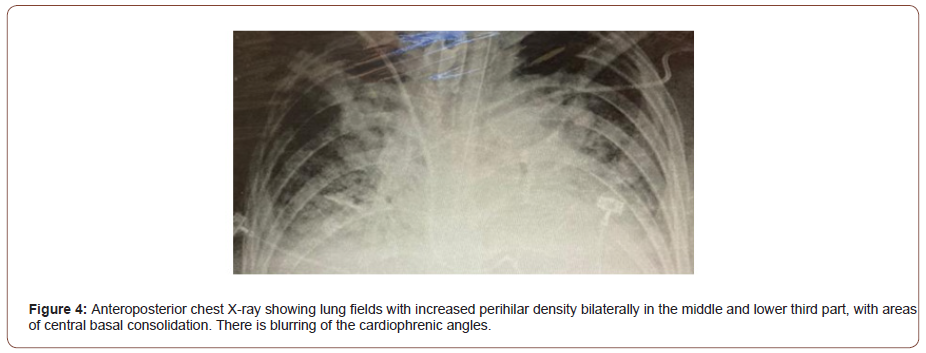
Patient 2: A 43-year-old female, overweight, with no other relevant history, who on day 1 reported headache, fever, myalgias, arthralgias, and dry cough. She underwent a rapid test for COVID-19 with a positive result on day 7. Outpatient management was started with ivermectin, azithromycin, acetaminophen, dexamethasone, enoxaparin, and oseltamivir without specifying the dose. The symptoms increased by day 16 and a decrease in saturation by pulse oximetry was added, reaching 63%, for which supplemental oxygen administration was started at home through nasal prongs at 2 liters/ minute, which increased saturation up to 83%. No improvement was achieved, so she was admitted to a hospital in Mexico City on day 17, where she was admitted to the COVID-19 area, and oxygen therapy was started with a mask/reservoir up to 15 liters/minute without an adequate response, and an Rx and TACT was performed where pulmonary compromise of >70% is evidenced, CO-RADS 6 (Figure 4 and Figure 5). Orotracheal intubation was performed on day 21 and she was transferred to the Hospital “Las Américas,” ISEM, on day 26, entering the ICU directly, with central venous access in the left subclavian vein with saturation by pulse oximetry of 83%, static distensibility 12.6 ml/cmH20, under sedation with a RASS scale of -5, without vasopressor support; volume-controlled mechanical ventilation is indicated with Vt 280 ml, RR 30 r/min, PEEP 9, FI02 100%, with the presence of peak pressure of 32 cmH20, plateau pressure of 29 cmH2O, DP of 20 cmH20, PM of 18.1 j/min, static compliance of 14 ml/cmH20, PAFI index of 71 mmHg, and prone position was started. The patient presented torpid evolution at the respiratory level from the beginning, with refractory hypoxemia, not responding to PEEP, with saturation by pulse oximetry of 85%. Therefore, on day 27, the administration of nitric oxide (NO) with the INOvent® system is started in the inhalation branch of the mechanical ventilator at 20 parts per million (ppm) (Figure 6), with an improvement in oxygenation of 94 %. On day 28, she presented feverish peaks of up to 38.4 °C and the onset of shock requiring a vasopressor. A urine culture result is obtained on day 29 (Table 3) and the antibiotic scheme was adjusted according to sensitivity. The patient continues to get worse and new cultures are performed, the results of which are obtained on day 34 and they show evidence of infection in the lower airway, classified as VAP with MDR, for which a new adjustment of the antibiotic scheme is made. A SG catheter with an HI is inserted after placement of PPE and asepsis and antisepsis protocol on day 34 (Figure 7). A hemodynamic pattern of mixed shock (septic and cardiogenic) was obtained with high vascular resistance, a relatively low PAWP with low CO and CI, so it could be classified as a profile with a tendency to hypodynamia, which persisted with decreased oxygen delivery and consumption. She also presented group III cardiac depression due to a severely diminished LVSWI from the first determination of hemodynamic parameters, for which dobutamine-type inotropes were started, showing a discreet response (Table 4). Despite fluid, vasopressor, and inotropic adjustments, the patient did not recover from severe cardiac depression. A Jackson-type tracheostomy was performed on day 34, maintaining high doses of vasopressor and NO therapy at 10 ppm. The patient died on day 38.
Table 3:Results of diverse cultures.
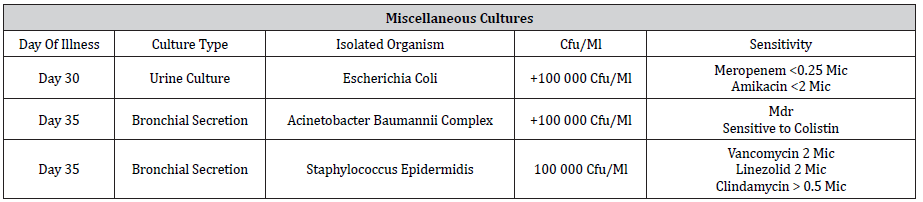
Table 4:SG hemodynamic parameters.

Discussion
In the first case, the shock pattern identified was clearly distributive due to sepsis in the hyperdynamic phase that was maintained despite the fall in LVSWI, outside the ventricular depression groups. In this case, it was associated with VAP with isolated germ, Acinetobacter baumannii complex/Staphylococcus aureus, and adding Pseudomonas aeruginosa, which was the cause of septic shock. Thus, at the beginning the patient had a normal CI and a decreased SVR; later this CI decreased with an increase in SVR and a final hemodynamic trend towards a hypodynamic phase.
The second case shows a patient who was admitted to the service almost 30 days after the disease had progressed, presented severe and refractory respiratory compromise, and started NO therapy, with a good response on oxygenation [8,9]. The hemodynamic pattern that the patient showed was a mixed shock, which is characteristic of the hypodynamic phase, depressed CO, and HF, so it can be understood that the septic shock caused pump failure to the point of developing cardiogenic shock. In the context of COVID-19, it is considered that the presence of cardiac dysfunction is caused by sepsis with marked depression of the left ventricle, as shown by LVSWI. This translates into contractility dysfunction of the functional unit of the myocardial fiber sarcomere, in addition to a VAP superinfection with an isolated germ (Acinetobacter baumannii complex/Staphylococcus epidermidis) that did not respond despite receiving antibiotic therapy directed by culture sensitivity. The patient did not present NO-associated renal dysfunction (*).
It should be noted that we did not find pulmonary arterial hypertension in the afore mentioned patients with severe COVID-19. The diagnosis was made by right heart catheterization, which is the most sensitive tool for detecting pulmonary hypertension (PH). This pulmonary vascular alteration has been described in publications such as Deng et al., Li et al., Zamanian et al., and Buja et al. [8], but none have approached it through pulmonary artery catheterization. The diagnostic criterion for PH was taken with a PmAP of >20 mmHg [9]. Likewise, it should be clarified that treatment with NO was indicated as therapy for refractory hypoxemia as part of the unit’s management algorithm.
Monitoring with the SG catheter is a tool for rapid decisionmaking at the patient’s bedside level. Although it is not a common pattern, such as accentuated myocardial depression in sepsis, COVID-19 has allowed us to learn from the evidence. The SG pulmonary artery catheter continues to be used in this COVID-19 pandemic; its use is practical and functional when it comes to distinguishing the cause of the shock state, considering the technical difficulty presented by using PPE. Being able to determine the cause of the hemodynamic deterioration of the critically ill patient helps to adjust vasopressors or inotropes if the patient’s cardiac depression justifies it. Therefore, it is an especially useful tool in decision-making [5].
Conclusions
The SG catheter is the gold-standard hemodynamic monitoring method, and it is used at the point-of-care patient’s bedside. Its use in critically ill patients and with severe COVID-19 patients has been extremely useful and practical for interpreting and adjusting treatment, which allows therapeutic dynamic modification. The hemodynamic profile that we evidenced by the SG catheter’s parameters in these patients with COVID-19 in the ICU is described for the first time during the pandemic.
Material and Data Availability
The database and additional material are avaible, previous request to the authors.
(*) Supplementary material

Participation Consent and Ethics
Confidentiality and personal data of patients are respected. They were approved with the prior informed consent signed by the patients and relative.
Publication Consent
All authors authorize this papers publication.
Conflict of Interests
We declare that we have no conflict of interest.
Funding
The study was funded by the authors and the hospital.
Authors Contribution
FJM and EXMG contributed to the concept and design. GMS, LESM, JGA, RTV, MMRP, VRS, JRSS, LLAS, WME and ACD contributed to procedures and patient selection. BEHM and FJM contributed to study´s methodological design.
Acknowledgments
We thank the hospital and our patients without whom it would have been impossible to carry out this study.
References
- Berlin D, Gulick R, Martinez F (2020) Severe Covid-19. n engl j med 383(25): 2451-2460.
- McIntosh K (2021) COVID – 19 clinical features. En: Up to Date, Post TW, (Ed) Up to Date. Waltham, MA: UpToDate Inc.
- Na Zhu, Dingyu Zhang, Wenling Wang, Xingwang Li, Bo Yang, et al. (2020) A Novel Coronavirus from Patients with Pneumonia in China, 2019. n engl j med 382(8): 727-733.
- José María CR, Giorgio André, José Luis S, Roberto Pedro PC, Anghella Fiorela VG, et al. (2021) Monitoreo hemodinámico invasivo por catéter de arteria pulmonar Swan-Ganz: conceptos yutilidad. Arch Peru Cardiol Cir Cardiovasc 2(3): 175-186.
- Carrillo A, Fiol M, Rodríguez A (2010) El papel del catéter de Swan-Ganz en la actualidad. Med Intensiva 34(3): 203-214.
- Maurizio Cecconi, Daniel De Backer, Massimo Antonelli, Richard Beale, Jan Bakker, et al. (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med 40(12): 1795-1815.
- Gentle Sunder Shrestha, Ninadini Shrestha, Ritesh Lamsal, Saurabh Pradhan, Anil Shrestha et al. (2021) Emergency Intubation in Covid-19. n engl j med 384(7): e20.
- Ajay Mishra, Amos Lal, Kamal Kant Sahu, Anu Anna George, Kevin Martin, et al. (2020) An Update on Pulmonary Hypertension in Coronavirus Disease-19 (COVID-19). Acta Biomed 91(4): e2020155.
- Gérald Simonneau, David Montani, David S Celermajer, Christopher P Denton, Michael A Gatzoulis, et al. (2019) Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 53(1): 1801913.
-
Edgar Xavier Martínez Guerrero, Felipe de Jesús Montelongo, Giovanni Morales Sánchez, Luis Eduardo Segura Medina. Hemodynamic Pattern by Swan-Ganz Catheter in Patients with Septic Shock Due to Severe Sars-Cov-2-Related Pneumonia: Case Report. Anaest & Sur Open Access J. 3(2): 2022. ASOAJ.MS.ID.000558.
-
COVID-19, Pneumonia, Antibiotic, Acute Respiratory Distress Syndrome, Myocardial, renal injury, Pulmonary Artery, Disease.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






