 Research Article
Research Article
Groin Dissection: A Comprehensive Analysis of Risk Factors and Postoperative Complications
Kristian Bugeja*, Tara Grima, Emma Mercieca, Katrina Bonnici and Duncan Aquilina
MSc Craniofacial Trauma Reconstruction, Queen Mary University, London
Kristian Bugeja, MSc Craniofacial Trauma Reconstruction, Queen Mary University, London
Received Date: October 30, 2024; Published Date: November 20, 2024
Abstract
Background: Groin dissection is a vital surgical intervention for managing metastatic lymph node involvement in melanoma and non-melanoma malignancies. Despite its importance in disease control, this procedure carries significant postoperative risks, particularly in patients with comorbidities or a history of smoking. This study evaluates the incidence of complications and related risk factors over a ten-year period.
Methods: A retrospective analysis was performed on 25 patients who underwent groin dissection at MDH between March 2014 and March 2024. Patient demographics, smoking status, co-morbidities, and surgical outcomes such as infection, seroma, and wound dehiscence were assessed.
Results: The majority of patients (88%) underwent delayed surgery, with melanoma being the most common primary diagnosis (40%). The average hospital stay was 15.08 days (range 1–53 days). Patients with a history of smoking and co-morbidities exhibited trends toward higher complication rates. Overall, 50% of patients experienced complications, including cellulitis (16%), seroma (8%), and wound dehiscence (4%).
Conclusion: Postoperative complications remain common after groin dissection, especially in patients with smoking history or co-morbidities. Further studies with larger cohorts are needed to better define these risk factors and improve patient outcomes.
Keywords: MDH: Mater Dei Hospital; ILND: Ingunial lymph node dissection; HTN: Hypertension; DM: Diabetes Mellitus; GORD: Gastro- Oesophageal Reflux Disease; IHD: Ischaemic Heart Disease; COPD: Chronic Obstructive Pulmonary Disease; BMI: Body Mass Index; SD: Standard Deviation
Introduction
Groin dissection is a crucial surgical intervention performed to manage metastatic lymph node involvement in patients with melanoma and non-melanoma malignancies. This procedure, while essential for disease control, is associated with a significant risk of postoperative complications, particularly in patients with complex co-morbidities or those with a history of smoking. At MDH, groin dissections are carried out for patients with a variety of primary cancers, including melanoma, squamous cell carcinoma, and rarer malignancies. This study aims to analyze the risk factors contributing to postoperative complications in patients undergoing groin dissection over a ten-year period, from March 2014 to March 2024. The primary focus is on the influence of patient demographics, smoking status, co-morbidities, and surgical outcomes such as infection rates, seromas, and wound dehiscence.
Objective
The objective of this study is to evaluate the prevalence and outcomes of complications in patients who underwent groin dissection at MDH over a ten-year period. The study specifically examines the impact of smoking status, co-morbidities, patient demographics, and surgical factors on the incidence of postoperative complications. This study also analyzes the clinical features and risk factors of complications associated with inguinal LN dissection (ILND).
Methods
This study involves a retrospective analysis of patients who underwent groin dissection at MDH between March 2014 and March 2024. Data collected includes patient age, gender, smoking status, co-morbidities, type of malignancy, length of hospital stay, and postoperative outcomes. The analysis focuses on identifying associations between these variables and the occurrence of complications, such as seromas, wound infections, lymphoedema, and wound dehiscence.
Results
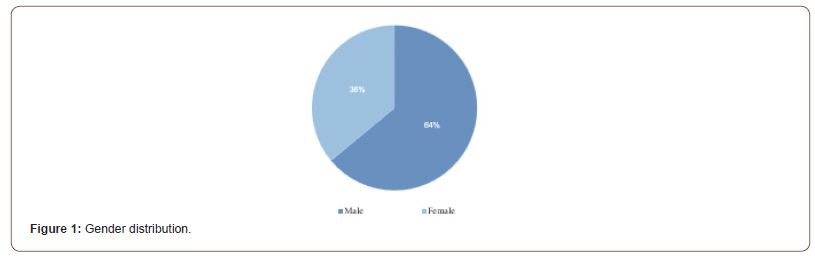
A total of 25 patients were included in this study, with an average age of 64 years (SD = 10.55). The age range of patients spanned from 45 to 80 years, indicating a wide variability in the age of patients undergoing groin dissection. In terms of gender distribution, 64% of the patients (16 individuals) were male, while 36% (9 individuals) were female, showing a male predominance in the patient population.
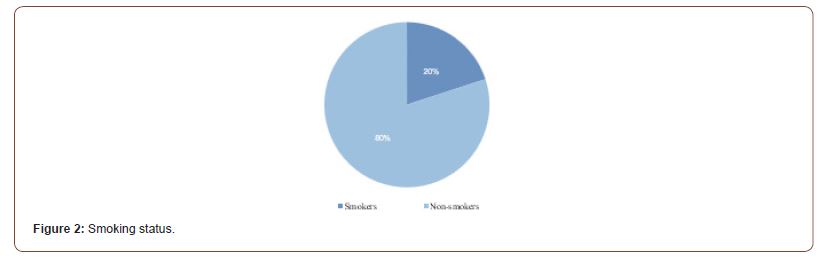
The majority of patients (80%, 20 patients) were non-smokers, while 20% (5 patients) reported being smokers. This data is important when considering postoperative complications, as smoking has been shown to negatively affect wound healing and increase infection risk.
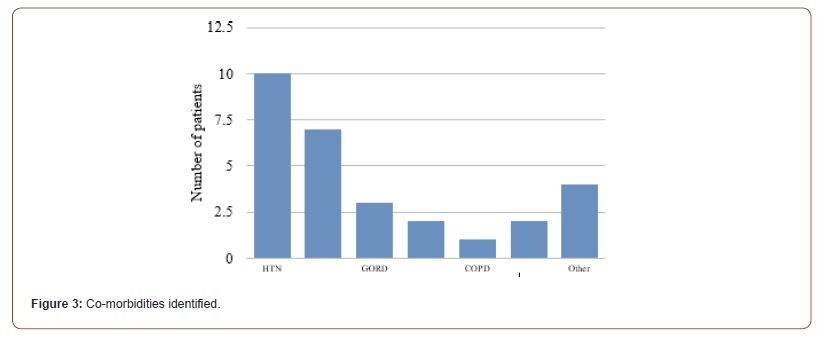
In this study, 28% (7 patients) had no reported co-morbidities. However, the majority of patients presented with at least one comorbidity. The most common co-morbidity was hypertension (HTN), affecting 40% (10 patients). Diabetes mellitus (DM) was present in 28% (7 patients), while gastro-oesophageal reflux disease (GORD) was observed in 12% (3 patients). Other notable co-morbidities included ischaemic heart disease (IHD) in 8% (2 patients) and chronic obstructive pulmonary disease (COPD) in 4% (1 patient). Additionally, 8% (2 patients) had hypothyroidism. Other co-morbidities included schizophrenia (4%), dyslipidaemia (8%), fibromyalgia (4%), osteoarthritis (4%), lichen sclerosis (4%), and sarcoidosis (4%).
The average length of hospital stay was 15.08 days, with a significant range from 1 to 53 days. In this study, the majority of patients (88%, 22 patients) had delayed surgery whilst only 8% of patients (2 patients) underwent both procedures concurrently.
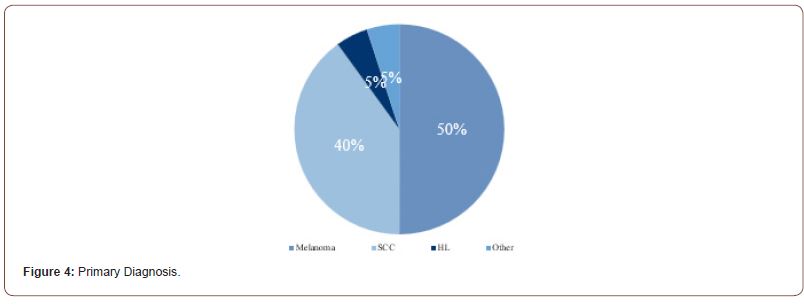
Melanoma was the most common primary diagnosis, observed in 40% of patients (10 patients). Squamous cell carcinoma was the second most frequent, accounting for 32% of cases (8 patients). These squamous cell carcinomas occurred in various anatomical areas, including the penile and vulval regions. Hodgkin’s lymphoma was identified in 4% of the patients (1 patient), while other rare malignancies, such as leiomyosarcoma and apocrine adenocarcinoma, were present in 4% of cases (1 patient).
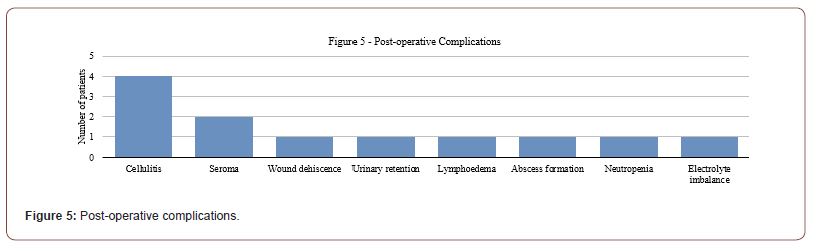
Complications following groin dissection were observed in 50% of the patients, while the remaining 50% had no recorded complications. The most frequent complication was cellulitis, which occurred in 16% (4 patients) of the cohort. Seroma was noted in 8% (2 patients), and wound dehiscence occurred in 4% (1 patient). Other complications, each affecting 4% of patients (1 patient each), included urinary retention, lymphoedema, abscess, neutropenia, and electrolyte imbalance.
Out of the 20 non-smokers, 12 patients (48%) had no postoperative complications, while 8 patients (32%) developed complications. Among the 5 smokers, only 1 patient (4%) did not experience complications, whereas 4 patients (16%) developed complications. Although there appears to be a higher proportion of complications in smokers, a Chi-square test yielded a p-value of 0.27, indicating that this difference is not statistically significant within this sample.
Among patients without any co-morbidities, 3 patients (12%) had no complications, and 4 patients (16%) developed complications. For patients with one or more co-morbidities, 10 patients (40%) had no complications, while 9 patients (36%) experienced complications. Despite the presence of co-morbidities showing a trend toward a higher complication rate, the Chi-square test produced a p-value of 1.0, suggesting no statistically significant association between co-morbidities and complications in this cohort.
The analysis of specific co-morbidities in relation to postoperative complications showed minimal associations in our study. Hypertension demonstrated a very weak correlation with complications (r = 0.03), suggesting that its presence did not notably impact complication rates within this group. Ischaemic heart disease (IHD) also showed an extremely weak correlation with complications (r = 0.01), indicating no significant relationship between IHD and postoperative outcomes. Diabetes mellitus (DM) exhibited a slightly stronger but still weak correlation (r = 0.11), implying only a minor association with an increased risk of complications. These findings indicate that, in this particular cohort, hypertension, IHD, and diabetes did not serve as substantial predictors of postoperative complications following groin dissection.
While it is commonly expected that advancing age may increase the risk of postoperative complications, the data from this study did not support this trend. Analysis revealed a weak negative correlation (r = -0.11) between age and the occurrence of complications, indicating that older patients were not more likely to experience complications than their younger counterparts. This outcome suggests that, in this cohort, age alone was not a significant factor influencing postoperative complications.
Discussion
This study sheds light on the complications associated with groin dissection, particularly in relation to smoking status and comorbidities. Although the statistical analysis did not find significant associations between these factors and complication rates (p-values of 0.27 for smoking and 1.0 for co-morbidities), trends indicate that smokers (16%) and patients with co-morbidities (36%) had higher rates of complications compared to non-smokers and those without co-morbidities. These findings align with Stuiver et al. (2014), who identified age and co-morbidities as risk factors for complications in melanoma patients, despite not finding a direct correlation with smoking [1]. Additionally, in line with Chang et al. (2010), our study showed minimal correlation between comorbidities such as hypertension, ischaemic heart disease, and diabetes and complication rates. However, Chang’s work does suggest that factors like diabetes could play a more significant role in postoperative outcomes when examined in larger cohorts, which may explain the lack of a strong association in our study.
Wound infections, seromas, and wound dehiscence were the most common complications in this cohort, consistent with findings in studies by Meguerditchian et al. (2022) and Chang et al. (2010), which also reported high rates of wound complications following groin dissection [2,3]. Meguerditchian’s study, for instance, highlighted that 56.1% of their patient cohort experienced complications within 30 days of surgery, particularly wound infections and seromas [2]. Similarly, Chang’s prospective study observed a 77.4% complication rate, identifying obesity as a significant risk factor for poor postoperative outcomes [3]. Although obesity was not specifically evaluated in our cohort, existing literature indicates that patients with a BMI ≥30 are at higher risk, as Chang’s multivariate analysis demonstrated that obese patients were 11 times more likely to experience complications [3].
This study also highlights that a large proportion of patients underwent delayed surgery (84.6%), which has been associated with worse outcomes in several studies. Meguerditchian et al. noted that surgeries for recurrent disease often result in more complications and poorer outcomes [2]. Furthermore, the use of prophylactic antibiotics, while applied in our cohort, remains an area for further investigation to fully understand its impact on infection reduction [4]. Additional strategies such as smoking cessation, effective management of co-morbidities, and prehabilitation may be beneficial in reducing complication rates among high-risk patients.
The financial and resource burden of complications underscores the need to minimise postoperative issues. Chang et al. reported that complications following groin dissection lead to significantly higher hospitalization costs [3], emphasizing the broader impact on healthcare systems and the importance of targeted intervention strategies.
The rate of inguinal lymphadenectomy has decreased according to evolving guidelines in the management of melanoma it is still the operation of choice in other malignancies eg SCC and in particular melanoma cases. These advances have deferred ILND to much more aggressive, clinically palpable disease or subsequent relapse. Worldwide this has resulted in fewer opportunities to achieve adequate training for these complex procedures and optimizing surgical outcomes have also decreased substantially. The advent of effective systemic therapy further reinforces the need for a reassessment of the impact of these surgeries as postoperative complications inevitably delay access to treatment.
It is considered to be a complex procedure and is known to be associated with a high risk of substantial postoperative morbidity even when meticulous technique is used, which affects both quality of life and survival. This surgery carries high risk of complications and so meticulous patient selection, preoperative planning, and patient optimization, in addition to presurgical systemic treatment to downstage the disease burden, may help to minimize the morbidity of ILND [5].
Studies show Asian patients have lower rates of surgical complications than Caucasian patients due to lower rates of diseases including obesity and diabetes [6].
Limitations
This study has several limitations. It is a prospective study and so data collection was limited to the data documented in medical records where certain patient information (eg BMI) was missing so we could not identify the correlation of obesity to the complication rate. The infrequency of the procedure and that the data was collected from a single centre resulted in a relatively small sample size. Despite these limitations, we have shown that the rate of complications after groin lymphadenectomy remains high. To improve on these future studies should use collaborative research to achieve greater numbers with prospective data.
Conclusion
In summary, this study highlights the trends observed between smoking status, co-morbidities, and complication rates in patients undergoing groin dissection. Although no statistically significant associations were found, the data suggest that smokers and patients with co-morbidities tend to experience higher complication rates. The findings reinforce the need for further research with larger sample sizes to clarify these associations. Additionally, targeted interventions such as smoking cessation, enhanced perioperative care, and managing co-morbidities may help improve outcomes in future groin dissection procedures.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Peel S, Eggbeer D, Sugar A, Evans PL (2016) Post-traumatic zygomatic osteotomy and orbital floor reconstruction. Rapid Prototyp J 22(6): 878-886.
- Marwan H, Sawatari Y, Peleg M (2020) Management of Post-Traumatic Orbital Zygomaticomaxillary Deformities and Secondary Reconstruction. In: Management of Orbito-zygomaticomaxillary Fractures. Springer, Cham. 2020:107-112.
- Mian SH, Umer U, Alkhalefah H, Ahmed F, Hashmi FH (2023) Design, analysis, and 3D printing of a patient-specific polyetheretherketone implant for the reconstruction of zygomatic deformities. Polymers 15(4): 886.
- Chepurnyi Y, Chernogorskyi D, Kopchak A, Petrenko O (2010) Clinical efficacy of PEEK patient-specific implants in orbital reconstruction. J Oral Biol Craniofac Res 10(2): 49-53.
-
Kristian Bugeja*, Tara Grima, Emma Mercieca, Katrina Bonnici and Duncan Aquilina. Groin Dissection: A Comprehensive Analysis of Risk Factors and Postoperative Complications. Anaest & Sur Open Access J. 5(5): 2024. ASOAJ.MS.ID.000621.
-
Mater Dei Hospital, Hypertension, Diabetes Mellitus, Gastro-Oesophageal Reflux Disease, Ischaemic Heart Disease, Chronic Obstructive Pulmonary Disease, Body Mass Index, Standard Deviation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






