 Research Article
Research Article
Endoscopic Endotracheal Intubation for ERCP In the Era of COVID: An Approach To Minimize Risk of Transmission of Infectious Diseases
Timothy Angelotti1*, Monique T Barakat2, Samer El Dika3 and Subhas Banerjee4
1Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA 94305, United States
2Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, CA 94305, United States
3Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, CA 94305, United States
4Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, CA 94305, United States
Timothy Angelotti, Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University, United States.
Received Date: September 26, 2023; Published Date:October 10, 2023
Abstract
Background and Aims: The close proximity between anesthesiologist and patient during endotracheal intubation are of major concern for potential infectious disease transmission. Development of intubation techniques with lower risks of infection transmission have led to a best practice recommendation of video laryngoscopy to minimize this distance. With ongoing infectious disease outbreaks, alternative intubation approaches to minimize risk of infection transmission still need to be established. Endoscopic intubation has not been widely considered, due to multiple concerns. However, it may be uniquely well-suited for patients undergoing endoscopic retrograde cholangiopancreatography (ERCP), due to the specific positioning and other requirements of the procedure.
Methods: We have previously studied the use of endoscopic rescue/elective asleep intubation in the semi-prone position during ERCP to enhance patient safety. We now report a series of patients who underwent ERCP following endoscopic intubation during our region’s initial COVID outbreak and highlight the features of this approach to reduce infectious disease transmission risk.
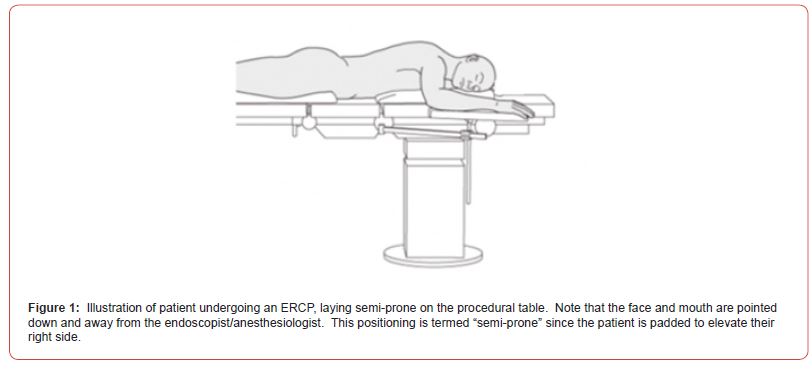
Results: We found endoscopic intubation to be quick (<1 minute) with minimal alterations to patients’ oxygen saturation or other vital signs. Endoscopic intubation maintained a minimum distance of four feet between the patient and anesthesiologist/endoscopist, with the patient oropharynx pointed down and away from both providers.
Conclusion: In this initial report and our prior studies, we have demonstrated the safety and efficiency of endoscopic intubation for ERCP. Therefore, we suggest that endoscopic intubation should be considered for lower risk, yet efficient, endotracheal intubation in the era of COVID and other infectious diseases.
Keywords:Endoscopic Retrograde Cholangiopancreatography (ERCP); Endotracheal Intubation; Monitored Anesthesia Care; General Anesthesia; COVID-19; Endoscopy; Fiberoptic Bronchoscopy
Abbreviations:ASA: American Society of Anesthesiologists; BMI: Body Mass Index; ERCP: Endoscopic Retrograde Cholangiopancreatography; ETT: Endotracheal Tube; MAC: Monitored Anesthesia Care
Introduction
Endotracheal intubation of patients infected with SARS-CoV-2 or other respiratory viruses represents a high-risk maneuver for disease transmission from patient to provider [1]. Given the close proximity between anesthesiologist and patient during intubation, infectious risks arise due to aerosolization of viruses, potentially accentuated by patient cough, Valsalva, or ventilation. Development of intubation approaches with the lowest risk of infectious disease transmission has become a focus within anesthesiology. During the initial COVID pandemic, initial reports suggested that establishment of dedicated airway response teams and video laryngoscopy represented a “best practice” for emergency endotracheal intubation [1, 2]. However, it still requires the anesthesiologist to be within inches of the patient’s mouth and airway.
As discussed by Gowd et. al., airway management for gastrointestinal endoscopic procedures is an area of concern for patient safety, to prevent hypoxic injury and aspiration events [3]. At our academic medical center endoscopy unit, we have studied urgent endoscopic endotracheal tube (ETT) placement in safely accomplishing rescue intubation during endoscopic retrograde cholangiopancreatography (ERCP) procedures that failed Monitored Anesthesia Care (MAC). We further confirmed the safety and utility of elective asleep endoscopic intubation for patients undergoing ERCP under general anesthesia with the patient positioned semiprone, demonstrating enhanced patient safety and endoscopy unit efficiency [4, 5]. Standard laryngoscopic intubation still requires the ERCP patient to be positioned semi-prone for the procedure, requiring the assistance of several care providers and disconnection of the patient from the ventilator circuit, increasing the risk of infectious disease transmission.
The semi-prone positioning of patients for ERCP may offer an opportunity to develop a best intubation practice utilizing endoscopic intubation to minimize patient-provider distance and infectious disease transmission, while safely accomplishing intubation. Given the longer length of a gastroscope compared to a laryngoscope, endoscopic intubation is readily accomplished, while maintaining a distance of up to 4 feet between the endoscopist/anesthesiologist and patient’s faces.
In this study we report a series of patients who underwent ERCP following endoscopic intubation during our region’s initial COVID outbreak. We highlight the features of this approach, which are favorable for intubation of patients undergoing gastrointestinal endoscopic procedures.
Methods
Data Collection and Statistical Analysis
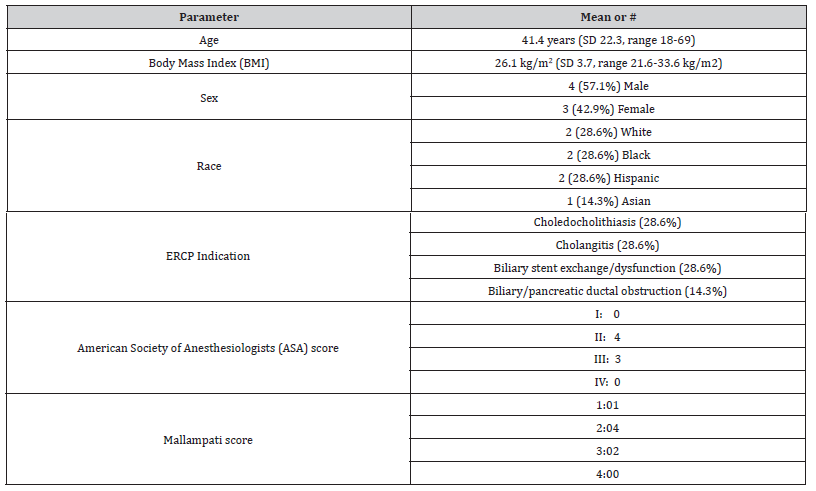
Demographic data (patient age, gender, co-morbidities, body mass index, ASA class and Mallampati score) were recorded. Anesthesia parameters, including intubation time, any challenges encountered during intubation and medications administered during intubation were documented. Potential procedure and anesthesia- associated adverse events were assessed immediately post-procedure. Standard descriptive statistical analyses were conducted. Given the limited number of patients included in this study, for normally distributed data (e.g., age, gender), mean and standard deviation (SD) were reported.
Technique
ERCPs during the study period were performed under general anesthesia in accordance with our prior studies [4, 5]. All patients who underwent intubation in this manner were administered standard- of-care anesthesia monitoring and induction medications (propofol, fentanyl, succinylcholine) and were pre-oxygenated for at least 5 minutes. Video-laryngoscopy and care team were available for urgent movement of the patient and standard intubation if needed.
Following induction of anesthesia, endoscopic intubation was accomplished by the endoscopist using an ETT backloaded onto an ultra-slim gastroscope (Evis Exerra III-Olympus America) to direct and advance the ETT into the trachea of the semi-prone patient, as described previously [4]. To limit the risk of transmission of infection to providers, it was decided that the endoscopist would perform the endotracheal intubation, with assistance from the anesthesiologist.
Results
Seven patients underwent endoscopic intubation for ERCP performed under general anesthesia at our tertiary care institution from April-June 2020 during the COVID-19 pandemic. Patient characteristics are listed in (Table 1). Patients positioned themselves in the semi-prone position on top of the ERCP fluorography table (Figure 1). They were padded for protection and to achieve the semiprone position; the patient is slightly tilted with their right shoulder elevated with a bolster. Endoscopic intubation was accomplished on the first attempt for each patient. Similar to our prior study of fifty patients, no emergent intubations were necessary [5].
Table 1:Patient Characteristics.
Duration from introduction of the gastroscope in the oropharynx to confirmation of endotracheal tube position was mean of 0.83 minutes (range 0.65 minutes – 1 minute), comparable to results from our prior larger study [5]. The lowest documented oxygen saturation during intubation for patients undergoing endoscopic intubation was 92% (mean 96.3%, range 92%-99%). There were no aspiration events, and no oropharyngeal trauma was evident during intubation for any of these patients, similar to our prior study [5]. The endoscopist and anesthesiologist remained up to 4 feet from the patient’s oropharynx during intubation of each patient.
All patients who underwent endoscopic intubation for this study were extubated immediately post-procedure. None of the patients reported oropharyngeal discomfort, or musculoskeletal symptoms. Lack of oropharyngeal/dental trauma was confirmed in all patients.
Discussion
With resurgence of COVID-19 variants and emergence of other infectious diseases (e.g., influenza A, respiratory syncytial virus), there is still a need for lower risk endotracheal intubation approaches for patients, where infectious disease status is not known. Traditionally, ERCP patients are intubated in the supine position and moved semi-prone for the procedure, further exposing healthcare team members to possible infectious disease transmission. Hence, there is an opportunity to develop endoscopic procedure-specific best intubation practices, that enhance patient safety [3].
But does endoscopic intubation have a role in the care of patients in an era when asymptomatic patients with unknown infectious disease status require intubation? Previous protocols do not include use of endoscopic/fiberoptic intubation for COVID-19 patients (unless a difficult airway was anticipated) [6, 7], due to theoretical concerns about the duration, complexity and aerosolization potential of this method, [8-10]. Thus, there is a need for identification of safe endotracheal intubation approaches that minimize risk of infection transmission and patient repositioning, while maintaining procedural efficiency.
Elective asleep endoscopic intubations have been utilized for procedures in patients without known difficult airways for multiple patient and procedure-specific reasons and we have examined the use of this approach in patients undergoing ERCP [5]. There is a need for improved airway management in endoscopic procedures and an endoscopic endotracheal intubation for ERCP procedures carries several advantages and may fulfil this need, as described previously [3, 11]. Intubation is accomplished briskly (<1 minute), the patient is anesthetized, muting the aerosol-generating cough reflex, the patient’s mouth is directed down and away from the intubating physician, and distance between patient and physician can be maintained at four feet during the entire intubation process [5].
This study was necessarily limited to non-COVID-19 patients due to our hospital protocol of COVID-19 screening and testing for infection prior to undergoing surgery or procedures; asymptomatic COVID-19 positive patients were not studied. However, we urge strong consideration for this approach in the care of COVID-19 positive patients as well. Through this initial report and our prior studies attesting to safety and efficiency of the technique, we introduce a potential approach which may be considered for lower risk endotracheal intubation, aside from just ERCPs.
Conclusion
With emerging infectious disease risks, endotracheal intubation techniques that minimize exposure of healthcare workers need to be developed. We propose that asleep endoscopic intubation of patients undergoing ERCP procedures can be safely performed, potentially reducing risk of transmission of infectious diseases to healthcare providers. Endoscopic intubation techniques should be considered and furthered explored in other procedural areas.
Author Contributions
Timothy Angelotti
Contribution: this author helped design the study, conduct the study, collect the data, analyze the data, and prepare the manuscript
Monique T Barakat
Contribution: this author helped design the study, conduct the study, collect the data, analyze the data, and prepare the manuscript
Samer El Dika
Contribution: this author helped design the study, conduct the study, collect the data, analyze the data, and prepare the manuscript
Subhas Banerjee
Contribution: this author helped design the study, conduct the study, collect the data, analyze the data, and prepare the manuscript
Authors’ Statement
This manuscript has been read and approved by all authors, requirements for authorship have been met, and each author believes that the manuscript represents honest work.
Acknowledgements
We appreciate the support of the Stanford Advanced Endoscopy Unit staff for assistance with this research project.
Conflict of Interest
No conflict of interest.
References
- Ferrando C, Colomina MJ, Errando CL, Llau JV (2020) Anesthesiology and the Anesthesiologists at COVID-19. Rev Esp Anestesiol Reanim 67: 289-291.
- Yao W, Wang T, Jiang B, Gao F, Wang L, et al. (2020) Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth 125(1): e28-e37.
- Gowd U, Bajwa SJS, Kurdi M, Sindwani G (2022) In pursuit of the right plan for airway management in gastrointestinal endoscopic procedures...the battle half won? Indian J Anaesth 66(10): 683-686.
- Barakat MT, Angelotti TP, Banerjee S (2021) Use of an Ultra-slim Gastroscope to Accomplish Endoscopist-Facilitated Rescue Intubation During ERCP: A Novel Approach to Enhance Patient and Staff Safety. Dig Dis Sci 66: 1285-1290.
- Barakat MT, Angelotti T, Ghosh S, Banerjee S (2023) Prospective Randomized Comparison of Endoscopist-facilitated Endotracheal Intubation and Standard Intubation for ERCP. Gastrointest Endosc 98(3): 441-447.
- Orser BA (2020) Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth Analg 130(5): 1109-1110.
- Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, et al. (2020) Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 75(6): 785-799.
- Sorbello M, Di Giacinto I, Corso RM, Cataldo R, Societa Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva Airway Management Research G (2020) Prevention is better than the cure, but the cure cannot be worse than the disease: fibreoptic tracheal intubation in COVID-19 patients. Br J Anaesth 125(1): e187-e188.
- Lyons C (2020) Fibreoptic tracheal intubation in COVID-19: not so fast. Br J Anaesth 125(1): e170-e171.
- Wu CN, Xia LZ, Li KH, Ma WH, Yu DN, et al. (2020) High-flow nasal-oxygenation-assisted fibreoptic tracheal intubation in critically ill patients with COVID-19 pneumonia: a prospective randomised controlled trial. Br J Anaesth 125(1): e166-e8.
- Janik LS, Stamper S, Vender JS, Troianos CA (2022) Pro-Con Debate: Monitored Anesthesia Care Versus General Endotracheal Anesthesia for Endoscopic Retrograde Cholangiopancreatography. Anesth Analg 134(6): 1192-1200.
-
Timothy Angelotti*, Monique T Barakat, Samer El Dika and Subhas Banerjee. Endoscopic Endotracheal Intubation for ERCP In the Era of COVID: An Approach To Minimize Risk of Transmission of Infectious Diseases. Anaest & Sur Open Access J. 4(3): 2023. ASOAJ.MS.ID.000588.
-
Anesthesiologist, Endoscopic intubation, Infectious diseases, Gastroscope, Oropharyngeal trauma, Musculoskeletal symptoms, Dental trauma, Respiratory syncytial virus
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






