 Research Article
Research Article
Determine Possible Associations Between Epidural Analgesia, Maternal Fever and Neonatal Outcome in the Indian Population: Observational Study
Nagaraju Munagala1*, Girishkumar Modi2 and Vijay Kumar3
1Anesthesiologist, Tawam Hospital, UAE
2Anesthesiologist, FLTA, Tawam Hospital, UAE
3Anesthesiologist, ESAIC, IDCCM, FCAI, Tawam Hospital, UAE
Nagaraju Munagala, Anesthesiologist, Tawam Hospital, UAE.
Received Date: June 15, 2023; Published Date:July 06, 2023
Abstract
Introduction: Epidural analgesia was introduced in 1942 and since then has been regarded as a main-stay for labor pain relief. Epidural analgesia is not only safe and well tried in over millions of women across the world, but it also causes the most maternal satisfaction among different techniques of analgesia. Epidural anesthesia can effect thermoregulation through multiple mechanisms that, depending on the circumstances, can result in an increase in core temperature.
Objective: To determine possible associations between Epidural analgesia, maternal fever and neonatal outcome in the Indian population.
Materials and methods: This is a prospective study of women delivered over four month’s period from May 2011 to August 2011. All women who delivered in the hospital during this period are included in this trial. Elective LSCS patients are excluded. A dose of 0.125% bupivacaine 10 ml with 2mcg/ml of fentanyl was administered initially. After satisfactory block was obtained, a continuous infusion of 0.125% bupivacaine with 2 mcg/ ml fentanyl at the rate of 8 -10 ml/hour was started. The temperature changes in women who choose epidural analgesia and the women who do not take epidural analgesia for labor are recorded every hour. After the delivery neonatal APGAR score at one minute and five minutes of birth, is noted in the labor ward. Sepsis screening of the neonate if done was recorded.
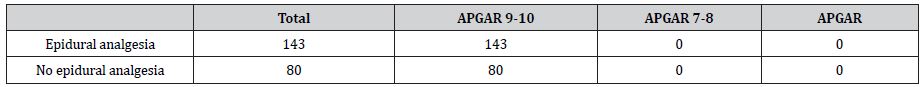
Result: Of the 223 women studied, 143(64.12%) received epidural analgesia during labor and 80(35.87%) did not received epidural analgesia. Of the 223 women 31.39% (n=70) developed fever compared to 68.61% (n=153) did not developed fever. Of the women who received epidural analgesia (143), 38.46% (n=55) developed fever>37.5°C during labor compared with 18.75 %(n=15) of women not receiving epidural analgesia (80). All the neonates born to either women with intrapartum fever or without intrapartum fever has 5-minute APGAR score of 9-10.
Conclusion: Epidural analgesia is found to be only incidental finding in parturient who developed clinical fever (temperature>37.5°C). So, Epidural analgesia should not be avoided based on the fear that analgesia induces fever or because of concerns about unnecessary neonatal evaluation for possible sepsis.
Keywords:Epidural analgesia; maternal fever; Neonatal outcome
Introduction
Epidural analgesia was introduced in 1942 and since then has been regarded as a main-stay for labor pain relief. Epidural analgesia is not only safe and well tried in over millions of women across the world, but it also causes the most maternal satisfaction among different techniques of analgesia [1].
A number of studies have been done on different methods of pain relief and it is clear that epidural analgesia gives the most maternal satisfaction with the least effects on the fetus. When epidural analgesia is given for pain relief during labor, many authors have noticed an association with a rise in maternal temperature.
Fusi and colleagues [2] first reported this association in 1989. This temperature rise is minimal, often in the range of 0.5-10C. Very rarely is this temperature over 380C. The precise mechanism of this temperature increase is unclear and may be due to altered thermoregulation (imbalance between heat production and heat dissipating mechanism), maternal-fetal infection or inflammation.
Labor was first associated with fever in the absence of infection [3] The activity of the uterus in labor contributes to core temperature and processes that interfere with heat dispersion can lead to fever.
Epidural anesthesia can effect thermoregulation through multiple mechanisms that, depending on the circumstances, can result in an increase in core temperature. Sympathectomy results in a redistribution of blood flow from the core to the periphery, initially leading to heat loss and a decrease in temperature. This effect is typically counterbalanced by intense shivering, resulting in heat production and negating the effect of redistribution of blood flow to the periphery [4]. In addition, sympathectomy can limit or even eliminate sweating, further contributing to heat retention. Furthermore, effective pain relief in labor can also decrease the hyperventilation often experienced by laboring women and can interfere with the ability to dissipate heat [5]. These processes in the setting of labor, a thermogenic event, can lead to a rise in temperature.
Though there have not been any major consequences of this rise in temperature, there has been an increase in neonatal sepsis evaluation. This is because one cannot ignore the fever in a mother and the likely consequences to the newborn. Though some studies have failed to demonstrate any change in temperature with epidural analgesia in labor, the majority of published literature has shown a rise in maternal temperature.
Materials and Methods
This is a prospective study of women delivered over four months period from May 2011 to August 2011. After IRB approval and informed consent, we recruited the patients delivering at private hospital, India.
Spontaneous or induced labor, term pregnancy and women who are in labor and have an emergency LSCS are included in the study.
Women who have Febrile illness at the onset of labor (Temperature> 37.5°C), Women who have used antibiotics in the last 5 days, Elective LSCS patients, Women whose WBC count is >11500 at the onset of labor are excluded from the study.
Epidural analgesia was administered upon patients request, usually early in the active phase of labor. A dose of 0.125% bupivacaine 10ml with 2 mcg/ml of fentanyl was administered initially. After satisfactory block was obtained, a continuous infusion of 0.125% bupivacaine with 2 mcg/ml fentanyl at the rate of 8-10 ml/ hour was started.
Paracetamol is given at the dosage of 10-15 mg/kg to a max of 1 gram total SOS whose temperature exceeds 38.0˚C and not to be repeated in next 6 hours. At our institute I.V fluids are started for all patients receiving epidural analgesia as background infusion of 2 ml/kg /hr. All patients are allowed to take clear oral fluids as required during intrapartum period.
Sample size at outset and power of study
Total number of patients studied are 223 out of which women who received epidural analgesia for labor are 143 and the women who did not received epidural analgesia for labor are 80.
Power of the study with this sample size with 5% alpha error level, and values derived from women with epidural analgesia- 38.46% have clinical fever and 61.54% has no clinical fever. Values derived from women without epidural analgesia-18.75% have clinical fever and 81.25% has no clinical fever has Statistical power of 88%.
Data collection Technique and tools
Epidural analgesia was administered upon patients request, usually early in the active phase of labor.
Fever was defined as tympanic temperature >37.5°C.
The clinical management of labor, including investigation for possible infection and the use of antibiotics and antipyretics such as paracetamol for fever, is at the discretion of the clinical team and according to unit protocol.
Simultaneous tympanic temperature (core body temperature) and room temperature are measured every hour throughout the labor.
Along with temperature the other parameters that are recorded are type of labor which is either spontaneous or induced and if induced the drugs used for induction.
Maternal vital data is recorded which included heart rate, blood pressure, and respiratory rate apart from temperature.
Duration of rupture of membranes, number of vaginal examinations, duration of labor and number of intravenous fluids used are also recorded.
After the delivery neonatal APGAR score at one minute and five minutes of birth, skin temperature of the neonate 30 minutes after birth, respiratory rate, presence of any retraction, flaring, grunting, weak cry, crepitations, excessive twitching, cyanosis and temperature are noted in the labor ward. Sepsis screening of the neonate if done was recorded.
Statistical significance P<0.05 was determined using student t test for comparison of continuous data, Chi square test, Mann– Whitney, logistic linear regression analysis with fever as a dependent variable was performed to adjust to potentially confounding factors.
Results
Total number of women studied is 223.
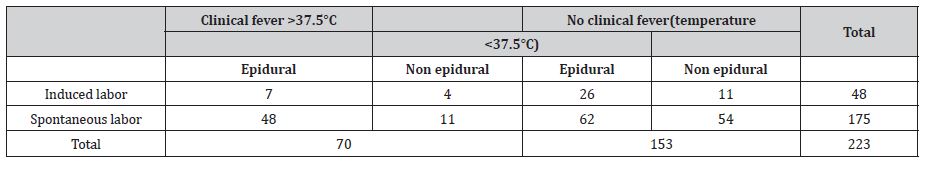
Of the 223 women studied, 143(64.12%) received epidural analgesia during labor and 80(35.87%) did not received epidural analgesia. Of the 223 women 31.39% (n=70) developed fever compared to 68.61 %(n=153) did not developed fever (Table 1). Of the women who received epidural analgesia (143), 38.46 %(n=55) developed fever>37.5°C during labor compared with 18.75 %(n=15) of women not receiving epidural analgesia (80) (Table 2). The mean age of the women who developed fever among epidural (27.38) and non-epidural groups (30.53) is higher than the women who has not developed fever with epidural (26.8) and without epidural (28.215) Of the 124 nulliparous women 40 developed fever and 80 did not. Of the 99 multiparous women 30 developed fever and 69 did not. Of the women who received epidural analgesia 43.2 %(n=35) nulliparous women developed fever compared with only 11.62 %(n=5) who did not received epidural analgesia (Table 1).
Among the group of women who received epidural analgesia, mean duration of labor (7.03 vs. 4.71), mean number of vaginal examinations (3.31 vs. 2.68) (Table 1).
Table 1:Maternal characteristics and demographics
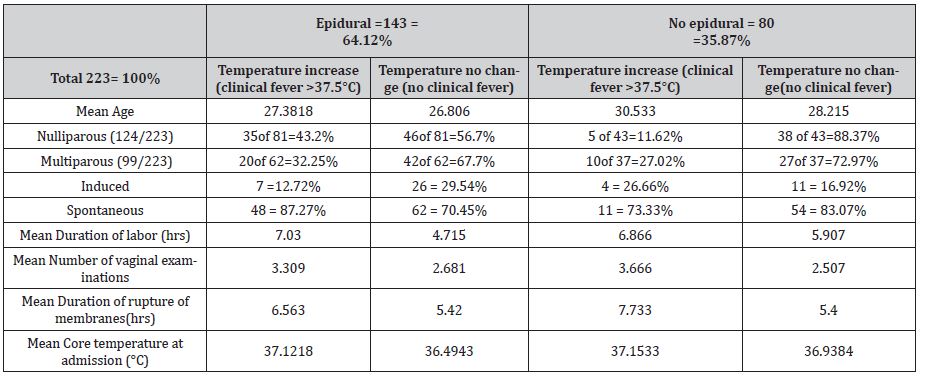
Table 2:Temperature change in relation to Type of labor and epidural and non-epidural groups.
Mean duration of rupture of membranes6.56 vs. 5.42), and core temperature of women at the start of labor (37.12 vs. 36.49) are higher in women who developed fever compared with women who did not.
The same is noticed in the group of women who did not received epidural analgesia. Mean duration of labor (6.86 vs. 5.91), Mean number of vaginal examinations (3.66 vs. 2.51), Mean duration of rupture of membranes (7.73 vs. 5.40), and core temperature of women at the start of labor (37.15 vs. 36.93). (Table 1)
When statistical analysis was done to determine statistical significance of p<0.05 among the groups of women who developed fever and the women who did not developed fever, Epidural analgesia (p=0.002), duration of labor (p<0.001), number of vaginal examinations (p<0.001), core temperature at admission (p<0.001) and duration of rupture of membranes (p=0.001) has got statistical significance. Age and type of labor has got no statistical significance.
When statistical analysis was done taking quantum change of temperature in consideration, linear regression analysis with dependent variable as quantum change of temperature was done epidural analgesia has got no statistical significance (p=0.106). Duration of labor, number of vaginal examinations, duration of rupture of membranes, and core temperature at start of labor has got statistical significance (p<0.001).
All the neonates born to either women with intrapartum fever or without intrapartum fever has 5 minute APGAR score of 9-10. All the neonates are discharged along with the mother on second day of delivery considering day of delivery as zero day. None of the neonates are sent for sepsis screening (Table 3, 4) (Figure 1, 2).
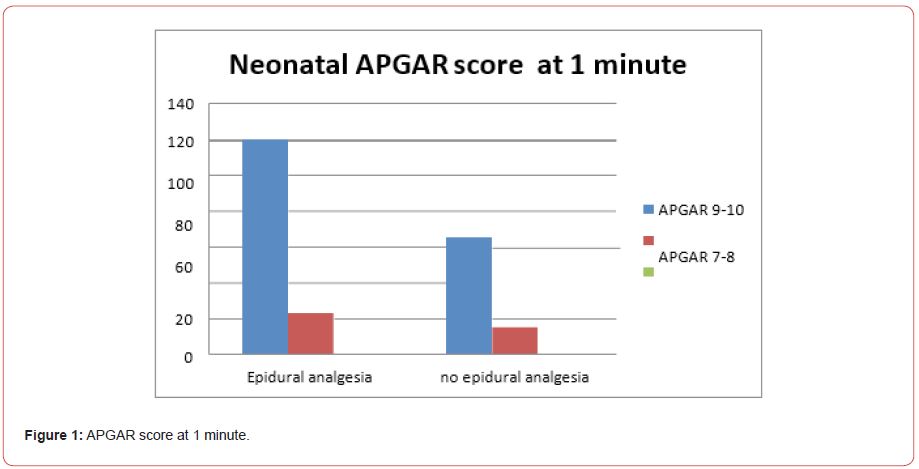
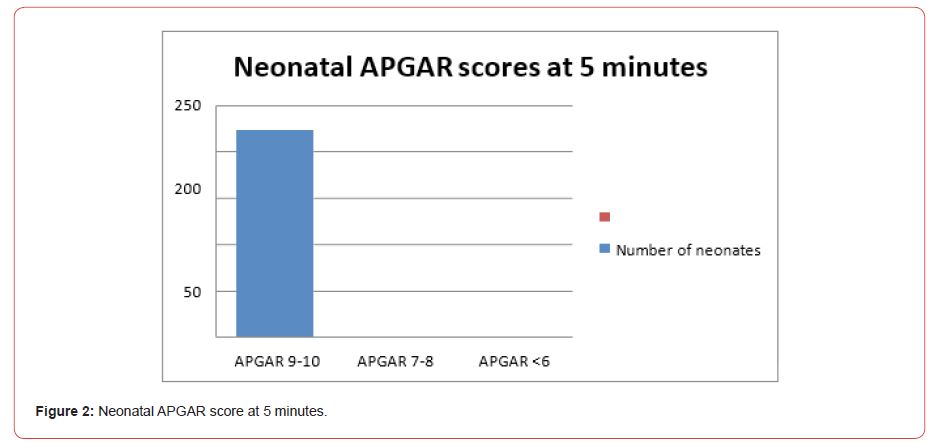
Table 3:APGAR scores of neonates at 1 minute.
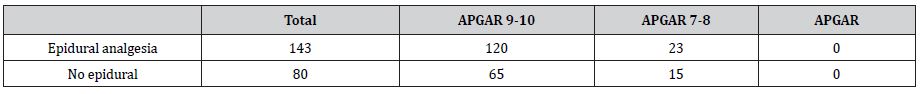
Table 4:APGAR scores neonates at 5 minutes.
Discussion
Many observational studies and Randomized control studies showed that epidural analgesia during labor is associated with maternal fever, although the nature of this fever is unclear. The consequences of maternal fever may include increased neonatal evaluations for sepsis, the increased use of antibiotics, and prolonged hospital stay.
Fusi and colleagues (2) presented the first evidence for the association between epidural analgesia and maternal fever. The precise mechanism of this temperature increase remains unclear.
In our observational study of (n=223) parturient, 143 women had epidural analgesia for labor and 80 do not have epidural analgesia.
In this study it is found that age (p = 0.168) of the parturient and the type of labor (p=0.155) has no significance in causation of fever.
In a observational study done by Ron Gonen, et al. [6]. when Age and Type of labor of the parturient is considered among Epidural and Non epidural groups, it has got a statistical significance of p=0.02 and p<0.001 respectively. These parameters are also studied among the women who received epidural analgesia with and without fever, only type of labor has got statistical significance (p=0.03).
In a Randomized control study done by John Phillip [7], it is shown that Epidural analgesia was associated with maternal fever (odds ratio 4.0, confidence interval 2.0 -7.7), as was nulliparity (0dds ratio=4.1 95% confidence interval=1.8-9.1)
In our study among women who received epidural analgesia and have clinical fever, more number of nulliparous women has clinical fever than multiparous women, but when linear regression analysis was done with dependent variable as temperature change parity has got no significance(p=0.752).
In our study duration of labor has got high clinical and statistical significance (p<0.001). It is also shown in many studies, observational study by Ron Gonen [6] (p<0.001), Randomized control trial by Goodlin RC and colleagues [8], Epidural analgesia was associated with maternal fever (odds ratio 4.0, confidence interval 2.0 -7.7), and labor longer than 12 hours (odds ratio 5.4, 95% confidence interval=2.9-9.9.
As the number of vaginal examinations and the duration of rupture of membranes increased, the incidence of clinical fever also increased. They have a statistical significance of p<0.001 and p=0.001 respectively with 95% confidence interval.
In the observational study by Ron gonen [6], mean duration of rupture of membranes has got no statistical significance p>0.05, and mean number of vaginal examinations has got a statistical significance of p<0.001.
In a study done by Lara Goetz, et al. [9] shown that labor epidural analgesia is not associated with fever, but it is a hyperthermia that is seen only in minority subset population which occurs immediately after exposure. Although most of the studies have shown noninfectious etiology of clinical fever during epidural analgesia, some studies have shown infectious etiology as a cause of fever during labor epidural analgesia. In a study done by Jode S. dashe [10], shown that epidural analgesia in labor is associated with fever, but only in the presence of placental inflammation.
When all the variables are studied on a linear regression analysis with dependent variable as quantum change of temperature, Epidural analgesia is found to be only incidental finding. It is seen that Core temperature at admission, duration of labor, number of vaginal examinations, and duration of rupture of membranes have got very high statistical significance (p values <0.000 and high tvalues).
Age, parity, type of labor and Epidural analgesia (p=0.106) has got no or weak statistical significance (p value >0.05 and low t values).
All the neonates born to either women with intrapartum fever or without intrapartum fever has 5-minute APGAR score of 9-10. All the neonates are discharged along with the mother on second day of delivery considering day of delivery as zero day. None of the neonates are sent for sepsis screening.
In a randomized control trial by Manth V.R.R [11] there were no differences in neonatal temperature or neonatal sepsis evaluation rate Epidural analgesia vs. No epidural analgesia 0/46 vs. 2/43, P = 0.45). Neonatal sepsis evaluation rates were similar in the two groups.
Conclusion
Epidural analgesia is found to be only incidental finding in parturients who developed clinical fever (temperature>37.5˚C). Increase in maternal temperature is mostly observed in women who have increased duration of labor, increased number of vaginal examinations, increased duration of rupture of membranes, higher core temperature at admission. Increase in maternal temperature during intrapartum period in normal healthy women without prior infection has got no clinical and statistical significance in our observation as all the women are discharged on the second day of delivery.
In our observation as all the babies born has 5min APGAR score of 9-10 and none of the babies required neonatal sepsis work up, furthermore all babies were healthy enough to be discharged within 48 hours. However keeping in mind the short duration of follow up of neonates as a limitation of this study, one cannot completely rule out any adverse neonatal outcome due to increased maternal temperature.
So, Epidural analgesia should not be avoided based on the fear that analgesia induces fever or because of concerns about unnecessary neonatal evaluation for possible sepsis.
Funding
None.
Acknowledgment
This study was mandatory thesis topic of author during anesthesia residency program. We are sincerely thankful to our PG teacher Dr. Subrahmanyam Maddirala for his support and guidance for this study.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- Braunwald E, Fauci AS, Kasper DL(2001) Harrison’s principles of internal medicine (15th edn,). New York: McGraw-Hill Companies.
- Fusi L, Steer PJ, Maresh MJ, Beard RW (1989) Maternal pyrexia associated with the use of epidural analgesia in labour. Lancet 1(8649): 1250-1252.
- Goodlin RC, Chapin JW (1982) Determinants of maternal temperature during labor. Am J Obstet Gynecol 143(1): 97-103.
- Hynson JM, Sessler DI, Glosten B (1991) Thermal balance and tremor patterns during epidural analgesia. Anesthesiology 74(4): 680-690.
- Marx GF, Green NM (1964) Maternal lactate, pyruvate, and excess lactate production during laborand delivery. Am J ObstetGynecol 90: 786-793.
- Ron Gonen, Roman Korobochka, Shimon Degani, Luis Gaitini (2000) Association between epidural analgesia and intrapartum fever. Americal journal of perinatology 17(3): 127-130.
- Philip J, Alexander JM, Sharma SK, Leveno KJ, McIntire DD, et al. (1999) Epidural analgesia during labor and maternal fever. Anesthesiology 90: 1271-1275.
- Goodlin RC, Chapin JW (1982) Determinants of maternal temperature during labor. Am J ObstetGynecol 143(1): 97-103.
- Goetzl L, Rivers J, Zighelboim I, Wali A, Badell M, et al. (2007) Intrapartum epidural analgesia and maternal temperature regulation. ObstetGynecol 109(3): 687-90.
- Dashe JS, Rogers BB, McIntire DD, Leveno KJ (1999) Epidural analgesia and intrapartum fever: placental findings. ObstetGynecol 93(3): 341-344.
- V R R Mantha, M C Vallejo, V Ramesh, A L Phelps, S Ramanathan (2008) The incidence of maternal fever during labor is less with intermittent than with continuous epidural analgesia: a randomized controlled trial. Int J Obstet Anesth 17(2): 123-129.
-
Nagaraju Munagala*, Girishkumar Modi and Vijay Kumar. Determine Possible Associations Between Epidural Analgesia, Maternal Fever and Neonatal Outcome in the Indian Population: Observational Study. Anaest & Sur Open Access J. 4(2): 2023. ASOAJ. MS.ID.000583.
-
Epidural analgesia, Clinical fever, Respiratory rate, Intrapartum period, Bupivacaine, Maternal-fetal infection, Labor pain relief, Maternal fever, Neonatal outcome
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






