 Opinion Article
Opinion Article
COVID-19 Pandemic: The Causative Agent is New, The Problem is Old
Igor Klepikov, Department of General and Pediatric Surgeon, MD, professor, retired, Washington, USA.
Received Date: May 05, 2021; Published Date:June 07, 2021
Introduction
The development of the SARS-CoV-2 pandemic has not only significantly changed the usual routine of life, but also contributed to the spread of feelings of anxiety and uncertainty. Today, no one can hope for a quick recovery and a favorable outcome in the case of COVID-19, even in the most advanced health systems. On the contrary, many developed countries, such as the United States, Great Britain, France, Italy and others, with excellent medical resources by modern standards, are among the leaders in the list of morbidity and mortality from coronavirus infection. The main cause of the negative consequences of SARS-COV-2 is viral pneumonia, and it is quite natural that one of the main tasks facing medicine today is to find effective ways to treat COVID-19 pneumonia.
The beginning of the pandemic and its subsequent development clearly showed that modern medicine is not ready for such a challenge and cannot provide adequate and effective assistance to a huge flow of patients. The problem of treating patients with COVID-19 pneumonia, strange as it may sound, began to form during the period of predominance of bacterial forms of the disease long before the development of the pandemic. The long-standing practice of treating completely incomparable diseases with a single antibiotic as the main remedy has completely distorted the understanding of the nature and mechanisms of the acute inflammatory process in the lung tissue.
The causative agent of inflammatory processes, which, as a rule, was a representative of the symbionts of the body, turned into the main cause of the development of acute pneumonia (AP), leaving many cardinal features of the disease without attention. AP, although not a contagious disease, was classified as an infectious disease many years before the current pandemic. In recent years, the main focus in the treatment of patients with AP is mainly on attempts to identify and suppress the bacterial factor, leaving aside the inflammatory process itself and its effect on the body’s functions.
As the effectiveness of antibiotics decreased, the resistance of microflora increased, and the proportion of viral forms of lung diseases increased, antimicrobial therapy no longer had the same effect as in the first years of its use. The need for additional care products that were used in patients with AP based on experience and analogies in the treatment of other inflammatory processes has steadily increased. It is surprising and perplexing that the functional features of the lungs, with their unique localization and the role of one of the most important regulators of the circulatory system, do not appear in the interpretation of the mechanisms and manifestations of AP.
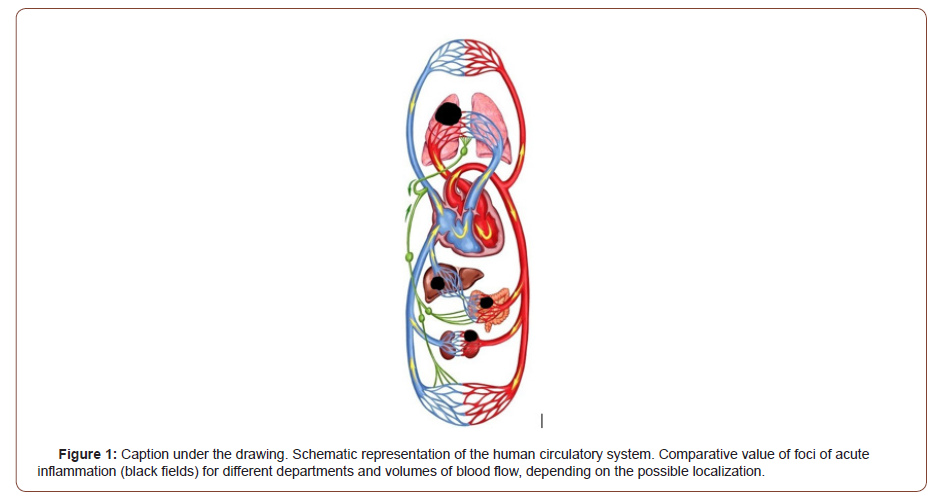
A comparative idea of how important a particular vascular segment is for the overall blood flow in the case of inflammatory transformation of various localizations is given by the schematic image [Figure 1]. This scheme allows only a visual and simplified assessment of the significance of the focus of inflammation in the lung for the general circulatory system, in contrast to similar processes in other internal organs. The schematic representation of the circulatory system of the body does not give an idea of the pathophysiological mechanisms of AP, but it gives a figurative idea that the effect on the general blood flow is an inevitable consequence of the inflammatory transformation of the lung tissue, regardless of the type of pathogen. This important feature of AP has not yet been taken into account, since for many years attempts to solve all the problematic issues of this disease were carried out through the prism of its pathogen.
The circumstances and factors listed above, and most importantly, the inconsistencies of theoretical concepts with the realities of practice, have long required a serious and radical revision of the strategic solution to the problem. However, the main attention was still paid to the causative agents of the disease, so regular changes in the etiology of AP against the background of taking antibiotics were accompanied only by periodic correction of tactical drugs. It is not surprising that the results of treatment continued to decline, and this negative trend did not find a reasoned explanation.
The slow but steady increase in AP deaths, despite the general concern about this fact, has come to be perceived as a natural phenomenon. The peak of mortality in intensive care units (ICU) among patients with community-acquired pneumonia in recent years has reached 30-50% [1-5]. These figures indicate that every second or third patient with this disease, getting into the intensive care unit, does not leave there. But even such grim statistics did not shake the prevailing stereotypes of a narrow etiotropic solution to the problem.
The system of views on AP and the resulting principles of medical care that have developed over the past decades automatically formed the basis of the COVID-19 pneumonia treatment strategy. The sudden loss of the role of antibiotics as the leading treatment for acute inflammation of the lung tissue required urgent and adequate replacement, so during the entire period of the pandemic, there is an intensive search for drugs to suppress the coronavirus.
Despite previous epidemics (SARS, MERS), medicine does not have specific means to combat the coronavirus. The resulting gap was tried to eliminate antiviral drugs that were used for other diseases. A huge number of publications on the results of the use of such drugs have shown that in the case of SARS-СOV-2, they do not give the expected effect. The final result of this work, based on the analysis of materials from 405 hospitals from 30 countries, was summarized and published under the auspices of WHO, which convincingly confirmed the absence of any therapeutic effect of such drugs in patients with COVID-19 and demonstrated the futility of searching in this direction [6].
If it is possible to create a drug against coronavirus, which many expect as a future salvation from this infection, then first you should look back at the previous experience of etiotropic treatment of AP and not deceive yourself with excessive hopes. Viruses, unlike bacteria, penetrate into cells, which makes it difficult to directly affect them with drugs and makes it difficult to obtain the effect of etiotropic therapy. In addition, antiviral drugs, like antibiotics, are designed against the causative agent of diseases, without directly affecting the inflammatory process itself. Stopping and completely eliminating inflammation remains the task of the body, the success of which adaptation depends on the speed of development of this process.
The term “pneumonia” is quite logically used in patients with COVID-19. With a coronavirus infection of the lung tissue, the structure and function of the same organ components as in the bacterial form of AP are disrupted. In this regard, the basis of the manifestation of the disease is identical, since we are talking about one nosology, and the severity of its manifestations also depends on the speed of development of the process and the volume of the lesion. Looking at the diagram above, it is easy to understand that a lesion in the lung, depending on its size, is able to block the main direction of blood flow, while inflammation of other internal organs affects regional blood circulation. However, this is a purely physical representation of one of the links in the complex pathogenesis of AP, which includes a sequential chain of a number of other mechanisms, factors and catalysts of the process.
AP is a dynamic process that is represented by a number of constantly changing and interrelated mechanisms. Each new stage of the disease is a consequence and derivative of the previous one and has its own distinctive feature and leading cause. From the initial phase of the disease to the development of its complications and terminal states, there are a number of phenomena that follow each other. In this regard, a detailed understanding of the causeand- effect relationships of AP is fundamental to the choice of adequate medical care. Unfortunately, today this leading feature of the disease is not properly considered. The pathogen and its properties remain in the spotlight.
The deceptiveness of the usual ideas about the nature of AP can now be seen in the example of mono infection with coronavirus. Despite the rapid spread of this formidable pathogen, its presence in the body does not necessarily mean disease. In many cases, the fact of infection can only be confirmed with the help of special tests. This well-known information indicates that for the development of the disease, as with bacterial forms of inflammation, additional factors and conditions are necessary. If the disease has not occurred, then, regardless of the strain of the pathogen and its virulence, there are no signs of its presence.
The overall picture changes dramatically with the onset of the inflammatory process, when the body begins to receive signals about damage to its own tissues and respond to this circumstance. Inflammatory transformation of the lung tissue is inevitably accompanied by a violation of its functions. This process has individual characteristics, but the faster it develops, the more difficult it is for the body to adapt to new conditions. The clinic of the disease is determined by the localization of the affected area, and not by the nature of its pathogen. Even one type of pathogen will give a completely incomparable picture when different organs are affected, right? Damage to lung structures, regardless of the etiology of inflammation, leads to equivalent functional disorders. This indisputable fact explains the extreme difficulty of differential diagnosis of bacterial and viral forms of pneumonia [7,8].
This information is the basis for assessing the current inflammation in terms of cause-and-effect relationships and paying special attention to the role and significance of the lesion in the lung. In practice, during this period of the disease, all the patient’s problems continue to be considered as a direct influence of the pathogen, and the attending physicians are concerned about neutralizing this cause. The further development of circulatory disorders in patients with AP is explained by septic shock, despite the fact that the pathogen in the blood is detected in individual observations and does not exceed the frequency of this positive test in the uncomplicated course of the disease [9-11]. Currently, by analogy with the previous concept, the severity of the condition of patients with COVID-19 pneumonia is explained by the development of viral shock [12,13]. But these are assumptions and analogies, and where is the objective evidence?
The AP concept has for many years interpreted the nature of the disease as infectious, regardless of its causative agent. The role of the pathogen in the dynamics of the disease became so absolute that the diagnosis of septic shock was determined on the basis of clinical and laboratory parameters, regardless of the results of bacteriological blood tests [14]. Currently, the methods by which attempts are made to eliminate the factors considered to be the result of viral aggression are coming to the fore. The set of such methods includes various inhibitors and blockers of biologically active substances, immunomodulatory drugs, hormonal and antiinflammatory therapy [15-23].
Such selective therapy of COVID-19 does not bring encouraging results and cannot count on great success. Each remedy is used against individual manifestations of the disease and acts on the effect, not on the cause of their occurrence. The chain of development of the inflammatory process and its consequences remains aloof from the choice of treatment methods. The idea of the course of the disease is focused on the activity of the pathogen at the cellular and molecular level, without explaining the global mechanisms of the dynamics of the process. For example, cytokines are markers of inflammatory damage to body tissues [24], but their neutralization will not affect the dynamics of inflammation. When a patient with inflammation and hyperthermia uses means to normalize the temperature, the inflammatory process does not stop there, does it? The same result should be expected from the neutralization of already circulating cytokines, and not from the cause of their production.
Today, the general trend of searching for the main causes of the disease and applied therapeutic efforts in AP in general and in COVID-19, in particular, has focused on the virtual-microscopic level, while the main object of this problem, a patient with a violation of his vital functions, receives palliative care and hopes for a better future. The situation resembles the reasoning of one of the heroes of the O ‘Henry novels, who asks: “Why the wind?” and he answers himself: “Because the trees are swaying!”
The patient reaches the critical stages of AP not because the virus has entered the cells of his body and led to the development of inflammation. This condition is mandatory only for the onset of the disease, but the symptoms and severity of the process depend on the individual reaction of the body to this contact with the infection, which determines the rate of development and the degree of damage. The whole picture of the disease will be significantly different if 10% or 80% of the lung tissue is eventually affected, right?
The desire to stop the “swaying of the trees” instead of building a barrier to the “wind” is observed throughout the entire period of the pandemic. The futility of continuing such attempts is confirmed by the absence of any positive results for a sufficiently long period on a huge material of observations. You can object and even take offense at this conclusion, but the axiom of medicine at all times was the fact that if the treatment does not bring the proper effect, then such help does not correspond to this disease, because today no one can say that he has made significant progress in the treatment of this category of patients.
The problem under discussion inevitably includes a number of fundamental provisions of medical science, which today undeservedly remain without due attention. These biological rules have worked and continue to determine the dynamics of the inflammatory process in the lungs, regardless of our perception. The importance of this information for the selection and justification of effective medical care for patients with AP has been proven on the basis of clinical application [25]. A detailed description of the materials of this work is now more important than at the time of its implementation, since over the past period this problem has become much more acute and has become an undoubted supertask for medicine. For its correct solution, it is necessary first of all to change the existing views on the essence of the disease, since without this complex step it is impossible to meaningfully and purposefully apply the necessary complex of specific medical care.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- A Liapikou E, Rosales Mayor, A Torres (2014) The management of severe community acquired pneumonia in the ICU. Expert Review of Respiratory Medicine 8(3): 293-303.
- J W Kim, J Kim, H J Yang (2015) The Prognostic Factors of Pneumonia with Septic Shock in Patients Presenting to the Emergency Department. Korean Journal of Critical Care Medicine 30(4): 258-264.
- P Jason, N C Dean, Q Guo (2016) Severe community-acquired pneumonia: timely management measures in the first 24 hours. Critical Care 20: 237.
- A Vidal, L Santos (2017) Comorbidities impact on the prognosis of severe acute community-acquired pneumonia. Porto Biomedical Journal 2(2): 247-346.
- A Ceccato, A Torres (2018) Sepsis and community-acquired pneumonia. Ann Res Hosp 2: 7.
- WHO Solidarity Trial Consortium, Pan H, Peto R, Henao Restrepo AM (2021) Repurposed Antiviral Drugs for Covid-19 - Interim WHO Solidarity Trial Results. N Engl J Med 384(6): 497-511.
- C Heneghan, A Pluddemann, K R Mahtani (2020) Differentiating viral from bacterial pneumonia. The Centre for Evidence-Based Medicine. Evidence Service to support the COVID-19 response. University of Oxford.
- Kamat IS, Ramachandran V, Eswaran H, Guffey D, Musher DM (2020) Procalcitonin to Distinguish Viral From Bacterial Pneumonia: A Systematic Review and Meta-analysis. Clin Infect Dis 70(3): 538-542.
- AJ Morgan, AJ Glossop (2016) Severe community-acquired pneumonia. BJA Education 16(5): 167-172.
- Garcia-Vidal C, Ardanuy C, Tubau F (2010) Pneumococcal pneumonia presenting with septic shock: host- and pathogen-related factors and outcomes. Thorax 65: 77-81.
- Hadil A. Al Otair, Mohammed A. Hussein, Mohamed A, et al. (2015) Severe pneumonia requiring ICU admission: Revisited. Journal of Taibah University Medical Sciences 10(3): 293-299.
- Alhazzani W (2020) Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med 46(5): 854-887.
- Prescott HC, Girard TD (2020) Recovery From Severe COVID-19: Leveraging the Lessons of Survival From Sepsis. JAMA 324(8): 739-740.
- Singer M, Deutschman CS, Seymour CW (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8): 801-810.
- M K Bohn, A Hall, L Sepiashvili (2020) Pathophysiology of COVID-19: Mechanisms Underlying Disease Severity and Progression. Physiology 35(5): 288-301.
- Attaway A H, Scheraga R G, Bhimraj A, Biehl M, Hatipoaylu U (2021) Severe covid-19 pneumonia: pathogenesis and clinical management. BMJ 372: n436.
- Loo J, Spittle DA, Newnham M (2021) COVID-19, immunothrombosis and venous thromboembolism: biological mechanisms. Thorax 76: 412-420.
- Christiansen CF, Pottegard A, Heide Jorgensen U (2021) SARS-CoV-2 infection and adverse outcomes in users of ACE inhibitors and angiotensin-receptor blockers: a nationwide case-control and cohort analysis. Thorax 76: 370-379.
- ACTIV-3/TICO LY-CoV555 Study Group (2021) A Neutralizing Monoclonal Antibody for Hospitalized Patients with Covid-19. N Engl J Med 384: 905-914.
- Ahmed I Siddiqi (2020) Cytokine flames of COVID-19. J Archives of Medical Case Reports and Case Study: 3(2).
- Farah H (2020) Potential Anti-Inflammatory Approaches for the Management of SARS-CoV-2 Infections. J Pulmon Respir Sci 5(S1): 000S1-001.
- To the Editor (2021) Cytokine Storm. N Engl J Med: 384: e59.
- Kory P, Kanne JP (2020) SARS-CoV-2 organising pneumonia: Has there been a widespread failure to identify and treat this prevalent condition in COVID-19?. BMJ Open Respiratory Research 7: e000724.
- https://en.wikipedia.org/wiki/Cytokine
- Igor Klepikov (2020) Acute pneumonia. New doctrine and first treatment results. Lambert Academic Publishing.
-
Igor Klepikov. COVID-19 Pandemic: The Causative Agent is New, The Problem is Old. Anaest & Sur Open Access J. 2(4): 2020. ASOAJ.MS.ID.000545.
-
COVID-19 Pneumonia, SARS-CoV-2, Acute pneumonia, Infectious disease, Acute inflammation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






