 Research Article
Research Article
Controlled Hypotension During Endoscopic Sinus Surgery: A Comparison of Propofol and Magnesium Sulfate
Hazem E Moawad, Mohamed Ezzat, Nabil A Mageed* and Maha Abo Zeid
Department of Anesthesia and Surgical Intensive Care, Faculty of Medicine, Mansoura University, Egypt
Nabil A Mageed, Professor of Cardiac Anesthesia, Department of Anesthesia and Surgical Intensive Care, Mansoura University, Egypt.
Received Date: September 26, 2020; Published Date: October 22, 2020
Abstract
Objective: Controlled hypotension is considered as an effective technique for reducing blood loss and optimizing the surgical field. This study was designed to compare intravenous infusion of propofol and magnesium sulfate for achieving controlled hypotension during elective endoscopic sinus surgery.
Methods: This randomized, double blinded, comparative study was conducted on fifty patients of either sex, aged between 18 and 45 years old underwent elective endoscopic sinus surgery. Patients were randomly categorized into two equal groups (25 patients each). Propofol group: patients were received intravenous infusion 75 mcg/kg/min of propofol for the first 15 minutes post induction and then a maintenance infusion of propofol (50 mcg/kg/min). Magnesium group: before induction of anesthesia, magnesium sulfate intravenous infusion was started at 40 mg/ kg in 100 ml saline over 10 minutes as a loading dose then magnesium sulfate infusion of 167 mcg/kg/min during surgery. Perioperative mean arterial blood pressure and heart rate were recorded. The intra-operative surgical field assessment and surgeon satisfaction score were assessed. The recovery profile was assessed by Ramsay sedation score and modified Aldrete score. Postoperative complications in the terms of postoperative nausea and vomiting and shivering were also recorded.
Results: The intraoperative mean arterial blood pressure was significantly decreased in propofol group at 15, 30, 45, 60 and 75 minutes after induction when compared to magnesium group. However, perioperative heart rate showed no significant changes between both studied groups. No statistical changes between the two studied groups as regard surgeon satisfaction and bleeding scores. Nitroglycerine doses were significantly higher in magnesium group than propofol group (P value<0.001). Postoperative Ramsay sedation scores were statistically significant higher, and the recovery time was significantly longer in magnesium group compared to propofol group (P value <0.001). Postoperatively shivering was significantly higher in propofol group compared to magnesium group while nausea and vomiting showed no significant changes between both groups.
Conclusion: This study concluded that intravenous infusion of propofol provided easily controlled hypotension, while intravenous infusion of magnesium sulfate was associated with a better recovery profile and reducing the incidence of postoperative shivering.
Keywords: Controlled hypotension; Magnesium sulfate; Propofol; Endoscopic sinus surgery
Introduction
Endoscopic Sinus Surgery (ESS) in which primary objective is the removal of pathology in the ostiomeatal complex has gained widespread acceptance in treatment of chronic sinus disease [1]. Endoscopic Sinus surgery usually associated with bleeding, despite using of local vasopressor injection [2], head up position [3], and tight control of the end-tidal carbon dioxide tension [4], controlled hypotension is generally used during endoscopic sinus surgery for control of this purpose. Different anesthetic techniques using different pharmacological agents have been used to induce controlled hypotension [5].
Propofol is a good agent for controlled hypotension by decreasing systemic vascular resistance due to arterial and venous vasodilation and a decrease in myocardial contractility with a dosedependent property [1]. Magnesium Sulfate also has been reported as an agent of hypotensive anesthesia by inhibition of the release of norepinephrine by blocking N-type calcium channel at the nerve ending beside acting as a vasodilator [6].
The pharmacodynamic effects of the intravenous infusion of propofol or magnesium sulfate may prove the advantage of this drugs in controlling intraoperative blood pressure and decrease the bleeding from surgical field. To the best of our knowledge, there have been no studies comparing controlled hypotension by propofol versus magnesium sulfate for endoscopic sinus surgery. So, the current study was designed to compare the efficacy of propofol and magnesium sulfate to control blood pressure during endoscopic sinus surgery and the resultant effects on the quality of the surgical field including bleeding and visibility. The primary outcome was the mean arterial blood pressure (MAP) after 15 minutes from the initiation of the intravenous infusion of the study drug. The secondary outcomes were the intraoperative heart rate (HR), total amount of intraoperative blood loss, need for blood transfusion and the consumed intraoperative amount of nitroglycerine, and ephedrine. Postoperative sedation scores, nausea, and vomiting (PONV), recovery time and surgical field assessment were also included.
Patients and methods
Study Design
This randomized, double blinded, comparative study was conducted at Mansoura University Hospitals. Fifty patients of either sex aged between 18 and 45 years old, American Society of Anesthesiologists physical status (ASA) I and II underwent elective endoscopic sinus surgery were included in this study from the first of September 2019 to the first of February 2020. After approval of the Institutional Research Board (IRB) of Mansoura University with a code number; MS/18.08.247 and Clinical Trials. gov registration number; NCT04078659, written informed consents were obtained from all patients. Exclusion criteria included patient refusal, patients with systemic hypertension, cerebrovascular insufficiency, or bleeding disorders, hemoglobin concentration<10gm/dl. Patients with any contraindication to controlled hypotension as cardiac diseases, increased intracranial pressure, patients with hypersensitivity to any drug used in the study including magnesium, propofol or isoflurane or patients on drugs known to have a significant interaction with the study drugs were also excluded. All patients were assessed preoperatively by history, physical examination, laboratory evaluation (complete blood picture, prothrombin time and International Normalized Ratio (INR), Alanine transaminase (ALT), Aspartate transaminase (AST), bilirubin, albumin, and creatinine).
Eligible patients were randomly allocated to one of two equal groups, each included 25 patients, by a computer-generated randomization table and concealed closed envelope method. The propofol group: patients were received intravenous infusion (IVI) of propofol, while the magnesium sulfate group: patients were received intravenous infusion of magnesium sulfate. The studied drug was prepared by wrapping its container and the line with opaque cover by the anesthetist who was not involved in the data collection. Over 10 minutes before induction, first 100 ml of normal saline was infused in propofol group, while in magnesium group 40mg/kg magnesium sulfate in 100 ml normal saline solution was administrated.
Anesthetic management
All patients were premedicated with intravenous midazolam (0.05 mg/kg) 20 minutes before anesthesia. On the patient’s arrival to the operating room, standard monitoring of electrocardiogram (ECG), noninvasive blood pressure and pulse oximetry were connected, and the basal values of HR and MAP were recorded. Two peripheral venous cannula 20 gauge were inserted. Anesthesia was induced by intravenous fentanyl 1 mcg/Kg, propofol 2 mg /kg and 0.6 mg /kg intravenous atracurium for endotracheal intubation. Then patients were mechanically ventilated to maintain the end tidal carbon dioxide tension (ETCO2) around 35 mmHg. Anesthesia was maintained by isoflurane 1.5% in 40% oxygen in air mixture. Immediately after general anesthesia induction, intravenous infusion of 75 mcg/kg/min of propofol was started for the first 15 minutes and then a maintenance infusion of 50 mcg/ kg/min during the surgery in propofol group. While in magnesium group, continuous intravenous infusion of 167 mcg/kg/min of magnesium sulfate was administrated. Patients were positioned at 20° head up tilt before starting the surgical procedure and 4ml of 1/100,000 adrenaline solution was injected in the nasal cavity as a topical vasoconstriction by the same surgeon in both groups. The intraoperative targeted MAP was between 50-70 mmHg. MAP less than 50 mmHg was considered as hypotension treated by 5 mg ephedrine and repeated till reaching the targeted MAP, but if MAP exceeding 70 mmHg, a bolus of intravenous nitroglycerine 30 mcg was administrated to reach the targeted MAP. Heart rate less than 50 beats /minute was considered as bradycardia and treated by 0.5 mg atropine. Propofol and magnesium sulfate infusions were stopped 5 minutes before the end of surgery at the stage of irrigating the field with saline and impaction of the nasal packs then isoflurane was stopped. Muscle relaxation was reversed by intravenous neostigmine 40 mcg/kg and atropine 20 mcg/kg.
Collecting Data
The MAP and HR were recorded before induction of anesthesia, intraoperatively immediately after induction, after Adrenaline local infiltration, then 5,15,30,45,60,75 and 90 minutes after general anesthesia induction, then immediately after anesthetics discontinuation and at the surgery end, and 15 minutes postoperatively.
Maximal allowable blood loss (MABL) was calculated using: where, MABL (mL): maximal allowable blood loss, H0: Hb start (gm/dl), H1: Hb target (gm/dl), EBV: expected blood volume (ml). EBV equals weight in kg x average 65 in adult female and 75 in adult male [7]. Hb start in gm/dl was the initial preoperative hemoglobin and Hb target was 8 gm/dl. Blood transfusion in the form of packed red blood cells (RBCs) was considered when the intraoperative blood loss exceeded the calculated MABL.
The intra-operative surgical field assessment was assessed by the same surgical team in terms of bleeding and visibility using a 6 point scale: 0 = no bleeding; 1 = minor bleeding, but no aspiration required; 2 = minor bleeding, aspiration required; 3 = minor bleeding, frequent aspiration required; 4 = moderate bleeding, visible only with aspiration; 5 = severe bleeding, continuous aspiration required [8]. Surgeon’s satisfaction with the operative field was rated using a 4-point scale at the end of surgery: 1= bad, 2 = moderate, 3 = good, and 4 =excellent.
The mathematical calculation of the intraoperative blood loss was calculated according to the formula stating: Estimated blood loss (ml) =expected blood volume (ml) x In (Hct1 / Hct2) Where: In is a calculator abbreviation refers to the natural logarithm of the current entry. Hct 1(%) is the initial preoperative hematocrit, Hct 2 (%) is the 1-hour postoperative hematocrit [9]. Hct was estimated one hour postoperatively. Ramsay sedation score was evaluated at 15, 30, 45 and 60 minutes post-extubation: 1=Anxious, agitated, restless, 2=Cooperative, oriented, tranquil. 3=Responsive to commands only, 4=brisk response to stimulus, 5-sluggish response to stimulus, 6-no response to stimulus [10]. Postoperative shivering was recorded while nausea and vomiting were assessed for the first postoperative 24 hours at 0-6, 6-12, 12-24 hour on scoring system; Absence of nausea or vomiting was = 0, nausea without vomiting = 1, vomiting one or two times-=2, and vomiting more than 2 times = grade 3 [11]. Time needed to reach a modified Aldrete score ≥ 9 was defined as the recovery time. The patients were discharged from the recovery room when they reached a modified Aldrete score of 10 (when they were able to move all extremities on response to a request, able to breathe deeply and cough freely, fully awake and had oxygen saturation >94% while breathing room air) [12]. The surgical duration in minutes and the total doses of intraoperative nitroglycerine, atropine and ephedrine were also calculated.
Sample size Calculation
Using a previous study [13], the mean ± standard deviation of the MAP at 15 minutes after induction of magnesium group was (76±6.9) assuming Þ error of 0.05; ß error of 10% (power 90%), 22 patients were needed in each group to detect a clinical decrease in the MAP 15 minutes post induction in propofol group. Allowing 10% drop out; 25 patients were included in each group to detect the difference between the two groups.
Statistical analysis
Statistical analyses were performed using SPSS version 24 (IBM, SPSS Inc., Chicago, IL, USA). The normality of data was tested using the Kolmogorov-Smirnov test. Continuous data of normal distribution are presented as mean ± standard deviation (SD) and were analyzed with the unpaired student’s t-test. Non-normally distributed data were analyzed with the Mann-Whitney U test and are presented as median [range]. Nominal data were analyzed with the chi-square test and are presented with number (percentage). Serial changes of MAP and HR over time were analyzed by repeated measures analysis of variance (ANOVA) using Greenhouse Geisser adjustment if the assumption of sphericity (assessed by Mauchly’s test) was violated. P was significant if P<0.05 at confidence interval 95%.
Results
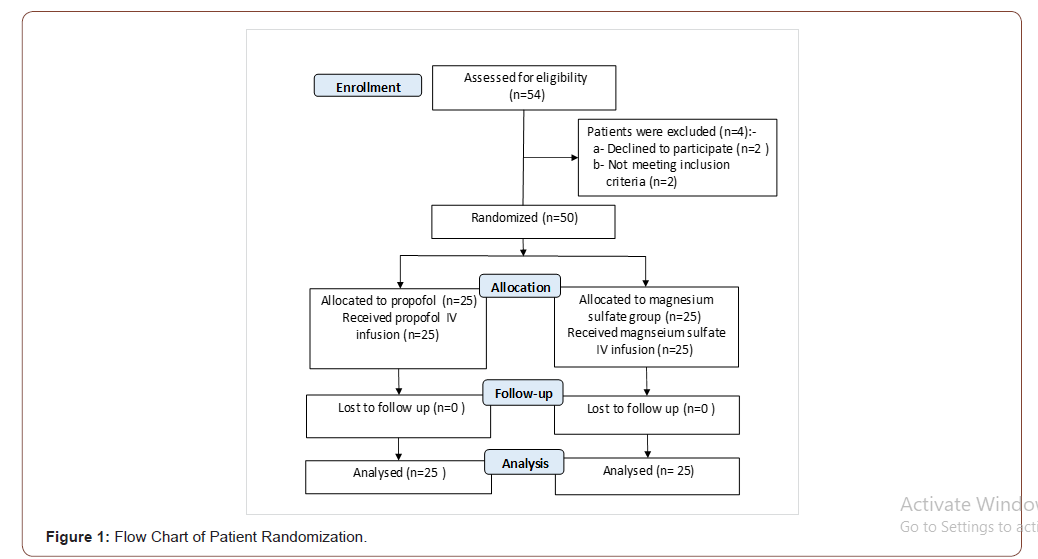
As shown in Figure 1, a total of fifty patients were included in this prospective, randomized, double blind, comparative study. 25 patients were analyzed in each group. The demographic characteristics and surgical duration of were summarized in Table 1. There were no significant differences as regard to patient age, sex, BMI, ASA class and surgical duration between the two studied groups.
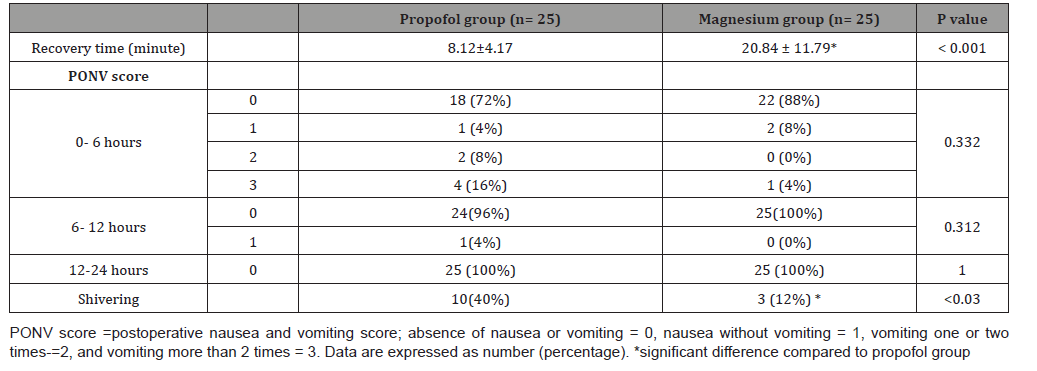
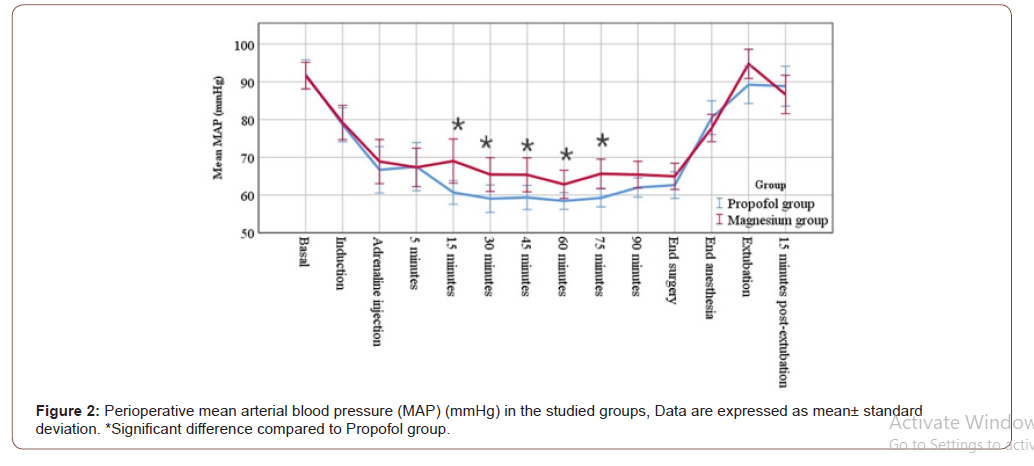
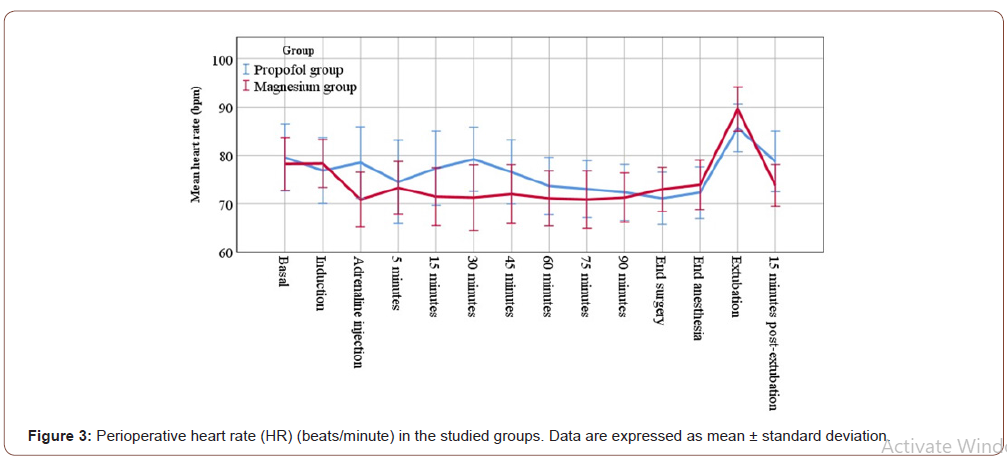
Concerning the primary outcome measure, the intraoperative MAP was significantly decreased in both groups compared to their baseline values (p value <0.001). However, the intraoperative MAP was significantly decreased in propofol group at 15, 30, 45, 60 and 75 minutes after induction when compared to magnesium group as illustrated in Figure 2 Postoperatively, the MAP should not significantly change between the two studied groups or in relation to the basal value of the same group (Figure 2). Both intra and postoperative readings of HR showed insignificant statistically changes either between the two groups or in relation to the basal value in the same group (Figure 3). There was not significantly changes between the two studied groups as regard the perioperative hematological data as shown in Table 2. Surgeon satisfaction and bleeding scores revealed insignificant statistical changes between the two studied groups (Table 3). Postoperative Ramsay sedation scores were significantly higher in magnesium group compared to propofol group at 15 and 30 minutes, while there was no significant change at 45 and 60 minutes in both groups (Table 4). The recovery time in magnesium group was significantly longer than in propofol group (P value <0.001) (Table 5). During the first postoperative hour, shivering was significantly lower in magnesium group than propofol group (Table 5). Post-operative 24 hours nausea and vomiting (PONV) score showed no significant changes between the both groups (Table 5). Nitroglycerine doses needed to maintain the targeted intraoperative MAP in magnesium group were significantly higher than propofol group (P value<0.001). However, ephedrine doses needed treat the intraoperative hypotension were significantly higher in propofol group when compared to magnesium group (P value=0.019). Also, the percentage of patients required intraoperative nitroglycerine/ ephedrine were 4 (16%) /10(40%) in propofol group versus 13(52%) /3(12%) in magnesium group, respectively. No significant difference in atropine doses needed in both studied groups.
Table 1:Demographic characteristics and surgical duration (minute) of the studied groups
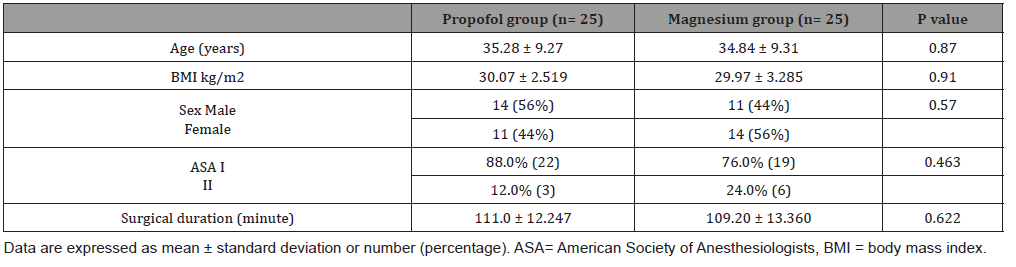
Table 2:Perioperative hematological data in the studied groups.
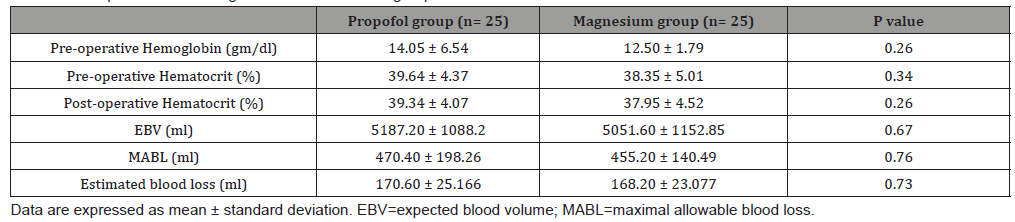
Table 3:Surgeon satisfaction and bleeding scores in the studied groups.
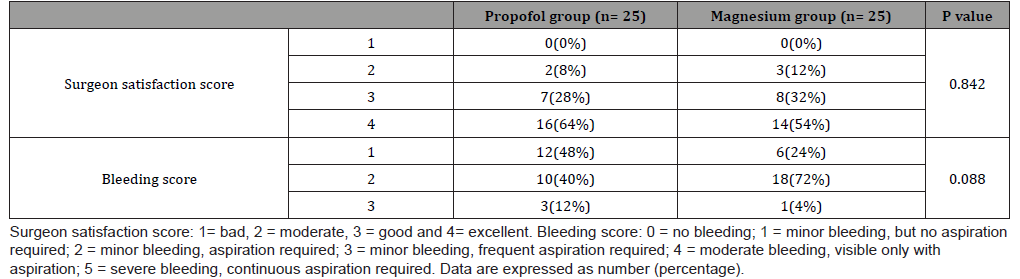
Table 4:postoperative Ramsay sedation score in the studied groups
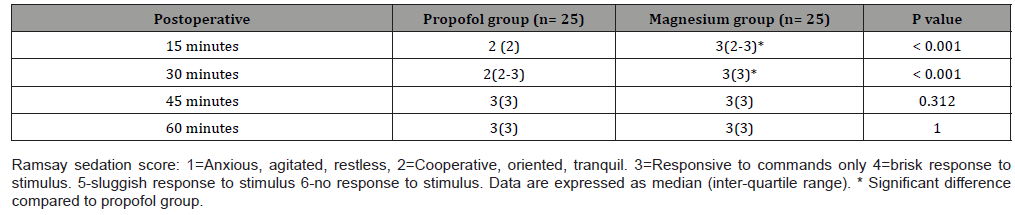
Table 5:Recovery time and post-operative complications in the studied groups.
Discussion
Controlled hypotension has a definitive role in ESS as it reduces bleeding during surgery and improves visibility of the surgical field; hence, it decreases the duration of surgery [7]. To best of our knowledge, this is one of the first randomized controlled trials comparing IVI of propofol and magnesium sulfate for controlled hypotension in ESS. In this study Propofol provided easily controlled hypotension. However, magnesium sulfate was found to be associated with a better recovery profile and reducing the incidence of postoperative shivering.
According to this study, MAP reduced significantly in propofol group than in magnesium group 15 minutes after induction suggesting more hypotensive effect of propofol in comparison to magnesium sulfate. The total number (percentage) of patients required intraoperative nitroglycerine/ ephedrine were 4 (16%) /10(40%) in propofol group versus 13(52%) /3(12%) in magnesium group which strongly confirm the more hypotensive effect of propofol. These results were consistent with Bayram A, et al. [14] who concluded that magnesium sulfate provided less controlled hypotension than dexmedetomidine in patients underwent ESS where ten patients in magnesium sulfate group needed intraoperative nitroglycerine versus only two patients in dexmedetomidine group.
In the current study, both groups showed a statistically significant decrease of all intraoperative MAP readings compared to their basal value. This greatest reduction explained by the combined effect of vasodilatation and myocardial depression of propofol [1,15] and calcium channel antagonism of magnesium sulfate with the production of vasodilator prostacyclin and nitric oxide [6,16]. This study demonstrated no statistically significant changes of all reading of the HR in both groups either between the two groups or in relation to the basal value in the same group which may be due to the balanced use of isoflurane inhalational anesthesia which has an additional vasodilatory effect associated with reflex tachycardia counteracting the possibility of propofol induce bradycardia [17]. While there was no associated tachycardia in magnesium group probably because of the association of magnesium sulfate infusion with angiotensin converting enzyme inhibition and slowing of sinoatrial node conduction [18]. On the contrary of our results, Ahn HJ, et al. [1] observed a significant bradycardia in propofol/ remifentanil total intravenous anesthesia group compared to sevoflurane/remifentanil group that is explained by the inhibitory effect of propofol on the baroreceptor reflex with more cardiac output suppression rather than sevoflurane. Elsharnouby NM and Elsharnouby MM [6], who studied the efficacy of magnesium sulfate as a technique of controlled hypotension during ESS, found a significant decrease of MAP, blood loss and duration of surgery without reflex tachycardia which support the results of the current study. By targeting intraoperative MAP between 50-70 mmHg, both groups reduced intraoperative blood loss irrespective to the study drug infusion. The calculated estimated blood loss in propofol group was (170.60±25.166) that did not significantly differ in magnesium group (168.20±23.077). Both did not exceed the MABL (470±198.26, 455.20±140.49, respectively). These results are in accordance with the study conducted by Bharathwaj and Kamath [19] who found that propofol infusion can reduce the intraoperative blood loss throughout the ESS by targeting intraoperative MAP between 60-70. However, Seruya M, et al. [20] concluded a negative correlation between the blood loss and controlled hypotension in ninety infants underwent fronto-orbital advancement for craniosynostosis.
The operative field and surgeon satisfaction assessed by Fromme GA, el al. [8], scale was similar in both the groups. All patients in both groups belonged to grade 1, 2 or 3 (for bleeding scale) and grade 2, 3, 4 (for satisfaction score) with no significant differences between both groups, which denotes highly acceptable surgical field as far as the same surgical team was concerned. The result of the current study is supported by Mathur and Nambiar [21] who reported that controlled hypotension by both dexmedetomidine/ isoflurane and fentanyl/propofol based anesthesia achieved an ideal surgical field during ESS in terms of high surgeon satisfaction and low bleeding scales. The present study showed higher Ramsay sedation score at 15, 30 minutes post-extubation and longer recovery time in magnesium group than propofol group (20.84±11.79, 8.12±4.17 respectively) which is explained by of N-methyl-d-aspartate receptors antagonism of magnesium sulfate with presynaptic competition with the calcium leading to reduction of the catecholamine release from the sympathetic nervous system thus enhancing the analgesic effect. Additionally, the action of magnesium sulfate at the neuromuscular junction leads to reduction of acetylcholine release from motor nerve terminals with reducing its depolarizing effect at the motor end plate thus potentiating the effect of the muscle relaxant [22]. Study conducted by Kalra N, et al. [23] who compared magnesium sulfate with clonidine in patients underwent laparoscopic cholecystectomy found that the duration until achieving a reply to verbal stimulus was longer in the magnesium sulfate group compared to the clonidine groups suggested by the depressant effects of magnesium sulfate on the central nervous system.
Despite of the high incidence of PONV after endoscopic sinus surgeries, both studied groups showed no significant changes in PONV score without the use of antiemetic drugs. These results may be due to the adjuvant effect of magnesium sulfate to produce periooperative analgesia by NMDA receptor antagonism [24], while the antiemetic effect of propofol may be due to the interaction with dopaminergic receptors in the chemoreceptor trigger zone thus limbic system inhibition affecting the cortical reflexes reaching the vomiting center [25].
In the current study, patients in magnesium group developed lower incidence of postoperative shivering (3 patients) than propofol group (10 patients) that explained by reducing the shivering threshold with subsequent smooth muscle relaxation in magnesium group [26]. These results are consistent with Ryu et al. [27] who concluded that both magnesium sulfate and remifentanil can induce adequate hypotensive anesthesia in patients undergoing middle ear surgery with reducing the incidence of shivering and PONV in magnesium group.
Study Limitations
limitations in this study was neither using of nerve stimulator nor bispectral index for neuromuscular block or anesthesia depth monitoring. Instead we depended on the recovery time and modified Aldrete score recording. Another limitation was postoperative non measurement of serum magnesium sulfate levels.
Conclusion: This study concluded that intravenous infusion of propofol provided easily controlled hypotension, while intravenous infusion of magnesium sulfate was associated with a better recovery profile and reducing the incidence of postoperative shivering.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Ahn HJ, Chung SK, Dhong HJ, Kim HY, Ahn JH, et al. (2008) Comparison of surgical conditions during propofol or sevoflurane anesthesia for endoscopic sinus surgery. Br J Anaesth 100(1): 50-54.
- Lee WC, Kapur TR, Ramsden WN (1997) Local and regional anesthesia for functional endoscopic sinus surgery. Ann Otol Rhinol Laryngol 106(9): 767-769.
- Cavalcante RC, Paola Fernanda Cotait de Lucas Corso, Guilherme dos Santos Trento, Fernando Antonini, Nelson Luis Barbosa Rebellato, et al (2018) Segmental orthognathic surgery for Bolton discrepancy correction. Oral and Maxillofacial Surgery Cases 4(3): 108-114.
- Kim YK (2017) Complications associated with orthognathic surgery. J Korean Assoc Oral Maxillofac Surg 43(1): 3-15.
- Cincikas D, Ivaskevicius J, Martinkėnas JL, Balseris S (2010) A role of anesthesiologist in reducing surgical bleeding in endoscopic sinus surgery. Medicina 46(11): 730-734.
- Elsharnouby NM, Elsharnouby MM (2006) Magnesium sulphate as a technique of hypotensive anesthesia. Br J Anesthesia 96(6): 727-731.
- Marzban S, Haddadi S, Mahmoodi H, Heidarzadeh A, Nemati S, et al. (2013) Comparison of Surgical Conditions During Propofol or Isoflurane Anesthesia for Endoscopic Sinus Surgery. Anesth Pain Med 3(2): 234-238.
- Fromme GA, Mac Kenzie RA, Gould AB, Lund BA, Offord KP (1986) Controlled Hypotension for Orthognathic Surgery. Anesth Analg 65(6): 683-686.
- Bourke DL, Smith TC (1974) Estimating Allowable Hemodilution. Anesthesiology 41(6): 609-612.
- Ramsay MAE, Savege TM, Simpson BRJ, Goodwin R (1974) Controlled Sedation with Alphaxalone-Alphadolone. Br Med J 2(5920): 656-659.
- Oh AY, Kim JH, Hwang JW, Do SH, Jeon YT (2010) Incidence of postoperative nausea and vomiting after pediatric strabismus surgery with sevoflurane or remifentanil-sevoflurane. British Journal of Anesthesia 104(6): 756-760.
- Aldrete AJ, Vazeery A (1989) Is Magnesium Sulfate an Anesthetic? Anesth Analg 68(2): 186-187.
- Rokhtabnak F, Djalali Motlagh S, Ghodraty M, Pournajafian A, Maleki Delarestaghi M, et al (2017) Controlled Hypotension During Rhinoplasty: A Comparison of Dexmedetomidine with Magnesium Sulfate. Anesth Pain Med 7(6): e64032.
- Bayram A, Ülgey A, Güneş I, Ketenci I, Çapar A, et al (2015) Comparison between magnesium sulfate and dexmedetomidine in controlled hypotension during functional endoscopic sinus surgery. Rev Bras Anestesiol 65(1): 61-67.
- Sahinovic MM, Struys MMRF, Absalom AR (2018) Clinical pharmacokinetics and pharmacodynamics of propofol. Clin Pharmacokinet 57(12): 1539-1558.
- Yogi A, Callera GE, Antunes TT, Tostes RC, Touyz RM (2010) Vascular biology of magnesium and its transporters in hypertension. Magnes Res 23(4): 207-215.
- Miller RD, Eriksson L, Fleisher LA, Wiener Kronish JP, Young WL (2010) Miller's anesthesia. Miller's anesthesia 2827-2827.
- Tangvoraphonkchai K, Davenport A (2018) Magnesium and Cardiovascular Disease. Advances in Chronic Kidney Disease 25(3): 251-260.
- Bharathwaj DK, Kamath SS (2019) Comparison of dexmedetomidine versus propofol-based anaesthesia for controlled hypotension in functional endoscopic sinus surgery. Southern African Journal of Anesthesia and Analgesia 37-40.
- Seruya M, Oh AK, Rogers GF, Boyajian MJ, Myseros JS, et al (2012) Controlled hypotension and blood loss during frontoorbital advancement. J Neurosurg Pediatr 9(5): 491-496.
- Mathur A, Nambiar PM (2014) Comparison of Dexmedetomidine-Isoflurane versus Fentanyl-Propofol based anesthesia for controlled hypotension in functional endoscopic sinus surgery. International Journal of Biomedical Research 5: 552.
- Dubé L, Granry JC (2003) The therapeutic use of magnesium in anesthesiology, intensive care, and emergency medicine: a review. Can J Anaesth 50(7): 732-746.
- Kalra N, Agarwal A, Verma A, Pandey HD (2011) Comparative study of intravenously administered clonidine and magnesium sulfate on hemodynamic responses during laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 27(3): 344-348.
- Al Shboul O, Mustafa A, Omar A, Al Dwairi A, Alqudah M, et al (2018) Effect of progesterone on nitric oxide/cyclic guanosine monophosphate signaling and contraction in gastric smooth muscle cells. Biomed Rep 9(6): 511-516.
- Thygesen MM, Rasmussen MM, Madsen JG, Pedersen M, Lauridsen H (2017) Propofol (2,6-diisopropylphenol) is an applicable immersion anesthetic in the axolotl with potential uses in hemodynamic and neurophysiological experiments. Regeneration 4(3): 124-131.
- Poblete R, Sung G (2017) Hypothermia for Acute Ischemic Stroke. Springer Series in Translational Stroke Research 477-499.
- Ryu JH, Sohn IS, Do SH (2009) Controlled hypotension for middle ear surgery: a comparison between remifentanil and magnesium sulphate. Br J Anaesth 103(4): 490-495.
-
Hazem E Moawad, Mohamed Ezzat, Nabil A Mageed, Maha Abo Zeid. Controlled Hypotension During Endoscopic Sinus Surgery: A Comparison of Propofol and Magnesium Sulfate. Anaest & Sur Open Access J. 2(3): 2020. ASOAJ.MS.ID.000536.
-
Controlled hypotension, Magnesium sulfate, Propofol, Endoscopic sinus surgery, Patients, Surgeon, Sedation, Nausea, Postoperative shivering
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






