 Research Article
Research Article
Comparative Efficacy of General and Regional Anesthesia in Total Hip Arthroplasty: A Comprehensive Review
Farhood Salehi*, Maamoon Mian and Cooper Phillips
Department of Anesthesiology, School of Medicine, Texas Tech University Health Sciences Center, Lubbock, Texas, USA
Farhood Salehi, Department of Anesthesiology, School of Medicine, Texas Tech University Health Sciences Center, Lubbock, Texas, USA
Received Date:June 03, 2024; Published Date:June 12, 2024
Abstract
Introduction: Total Hip Arthroplasty THA replaces a damaged hip joint to alleviate pain. Anesthesia, crucial for safety, is chosen in preoperative consultations. General anesthesia induces unconsciousness; regional anesthesia numbs the lower body in THA. Ongoing research on anesthesia modalities in THA remains inconclusive, warranting further study for efficacy and reliability.
Methods: This study explores postoperative outcomes associated with general and spinal anesthesia through a review, integrating findings from three Randomized Controlled Trials (RCTs) and one clinical trial. RCTs include evaluations of patients over 65, recovery profiles of 120 patients assessing hospital stay, nausea, and pain levels. Additionally, a comparison of general, spinal, and caudal anesthesia in 198 patients analyzes analgesic requirements, Beta amyloid expression, and postoperative pain and cognitive functions. The clinical trial examines pulmonary embolism incidence, transfusion requirements, and blood flow in 30 patients undergoing caudal or general anesthesia.
Results: Trial outcomes align with the meta-analysis, revealing minimal differences between regional and general anesthesia in postoperative complications. The need for more extensive research is emphasized. The first RCT, with 941 participants, showed comparable postoperative delirium rates, worst pain, hospitalization, mortality rates, episodes of nausea, vomiting, and hypotension. The second RCT, with 120 participants, demonstrated a slightly reduced hospital stay with general anesthesia, and lower pain levels after 6 hours. The third RCT, with 198 participants, indicated fewer perioperative adverse effects with regional anesthesia compared to general. In the clinical trial, with 30 participants, continuous epidural block exhibited a lower frequency of deep vein thrombosis (DVT) compared to general anesthesia.
Conclusion: This review emphasizes the need for ongoing research about anesthesia choice in THA. The evidence reveals subtle distinctions between various techniques. It is crucial to sustain research efforts to refine our understanding of the most suitable anesthesia for specific demographics with underlying conditions. Such insights will enable surgeons and anesthesiologists to make better decisions in selecting the appropriate technique for THA.
Keywords:Total Hip Arthroplasty; General Anesthesia; Regional Anesthesia
Objective:The purpose of this review is to provide a collection of information to better aid surgeons and anesthesiologists make more informed decisions regarding patients undergoing total hip arthroplasty. Additionally, this review serves as a point of emphasis for future research by highlighting the need for continued investigation.
Introduction
Total hip arthroplasty (THA) [1] remains a cornerstone in the management of debilitating hip joint conditions, significantly improving quality of life through pain relief and enhanced mobility. THA is a procedure in which the damaged joints, bones, and cartilage are removed and replaced by prosthetics. Components typically include: an acetabular component, a plastic liner, a femoral head, and a femoral stem (American College of Orthopaedic Surgeons). THA is recommended for patients with severe, end stage arthritis caused by a variety of complications including osteoarthritis, rheumatoid arthritis, inflammation, and infection, as well as rare conditions like osteonecrosis. THA is generally considered when non-surgical options fail. The procedure is completed by an orthopedic surgeon. THA is a relatively common procedure with roughly 544,000 surgeries performed annually in the United States (American College of Rheumatology). In fact, over the past decade, the number of THA procedures has increased exponentially. Between 2000 and 2019, the volume of THA surgeries increased by 117%, and projection models indicate a growth of 176% by the year 2040 [2]. The efficacy of THA heavily relies on anesthesia techniques, understanding their impacts on postoperative outcomes is critical. This review will leverage findings from several pivotal studies to explore the comparative effectiveness and safety of general and regional anesthesia in THA.
The RAGA Randomized Trial highlights that regional anesthesia may lower the incidence of postoperative delirium in older patients compared to general anesthesia, suggesting a potential advantage in cognitive outcomes [3]. Meanwhile, a controlled trial (2015) provides evidence that total intravenous general anesthesia might offer benefits in terms of shorter hospital stays and reduced postoperative pain, albeit within a specific patient demographic [4].
Further comparison of anesthesia modalities reveals subtle but significant differences in analgesic requirements and safety profiles, indicating that the choice of anesthesia should be tailored to individual patient needs [5]. Other contributions to this discourse reveal that epidural anesthesia may significantly reduce the risk of deep venous thrombosis and pulmonary embolism compared to general anesthesia, underscoring its potential benefits in thromboembolic prophylaxis [6].
In addition to clinical findings, surgical techniques such as the direct anterior approach for THA also interplay with anesthesia choice, affecting accessibility and potentially influencing postoperative results [7]. A Meta-Analysis, performed in 2019 synthesizes data across studies, confirming that while both anesthesia techniques are effective, the nuances in their impacts on specific outcomes warrant further investigation [8].
This review will set the stage for a detailed examination of how anesthesia choices influence the recovery trajectory and overall success of THA, guided by the current evidence base [9].
Methods
This study conducts a comprehensive review to evaluate the postoperative outcomes associated with general and spinal anesthesia in total hip arthroplasty (THA). By integrating and analyzing data from three randomized controlled trials (RCTs) and one clinical trial, this research aims to elucidate the relative efficacy and safety of these anesthesia modalities.
Randomized Controlled Trials (RCTs)
Patient Demographics and Recovery Outcomes:
The first RCT (Li et al., 2021) focuses on examining the differential use of general and regional anesthesia on post-operative complications. This study assesses a wide range of recovery outcomes, including the duration of hospital stay, frequency and severity of nausea, and pain levels post-surgery. They performed their trial in a randomized, multicenter clinical trial of 950 patients.
The inclusion criteria include:
a. Patients above the age of 65
b. Patients with or without existing dementia
c. A fragility hip fracture requiring repair
d. Participants enrolled between October 2014 and September 2018
The patients were then designated into two intervention groups: regional anesthesia n=476 (including Caudal Epidural and Spinal) and general anesthesia n=474.
Anesthesia Modalities Comparison:
The second RCT [4] examines a cohort of 198 patients and compares the effects of three different anesthesia techniques: general, spinal, and caudal anesthesia.
Inclusion criteria include:
1. Patients undergoing THA
2. Patients suitable for both general anesthesia and caudal epidural anesthesia
This trial evaluates key outcomes such as analgesic requirements post-surgery, the expression of Beta amyloid (which is often linked with cognitive functions), and overall postoperative pain management and cognitive outcomes.
Diverse Patient Profiles:
The third RCT [5] includes a diverse patient profile to assess a comprehensive range of recovery indicators across a sample of 120 patients.
Inclusion criteria include:
i. Patients with no history of nervous system surgery
ii. Patients with no history of cardiovascular surgery
iii. Patients with no defective vision
iv. Patients with no history of mental illness
v. Patients with no neurological disorders
This study provides a broader understanding of how different anesthesia approaches may impact patient recovery in a typical clinical setting.
Clinical Trial
This trial focuses on a smaller group of 30 patients to provide a detailed examination of more critical outcomes such as the incidence of pulmonary embolism, transfusion requirements, and blood flow metrics post-surgery.
Inclusion criteria include:
I. Patients undergoing THA
II. Patients suitable for both general anesthesia and caudal epidural anesthesia
III. Patients not receiving dextran or antithrombotic drug prophylaxis
Patients in this trial undergo either caudal or general anesthesia, allowing for a focused investigation into the safety profiles of these methods, particularly in the context of potentially life-threatening complications.
Data Integration and Analysis:
The findings from these RCTs and the clinical trial will be integrated using an analytical approach. This will involve a review of the collected data to identify patterns, discrepancies, and establish a comprehensive understanding of the impacts of anesthesia type on postoperative outcomes in THA. Statistical methods including repeated measures analysis, confidence interval and standard error analysis, and descriptive statistics will be employed to ensure that the integration of data from multiple sources is handled rigorously, providing robust conclusions that are representative of larger population trends.
Results
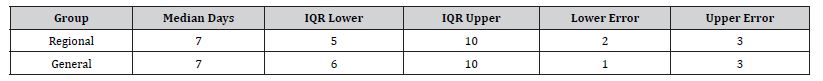
The results analyzed from all sources revealed interesting discrepancies in the measurement of post-operative outcomes in patients undergoing Total hip arthroplasty. The result of the first randomized controlled trial found results favoring general anesthesia. The analysis of postoperative outcomes revealed notable differences between regional and general anesthesia in total hip arthroplasty (THA) patients. The incidence of postoperative delirium was slightly higher in patients who received regional anesthesia at 6.2%, compared to 5.1% in those who underwent general anesthesia. Similarly, the rates of nausea and vomiting were significantly higher under regional anesthesia (44.3%) than under general anesthesia (33.3%). Hypotension was also more frequently observed in the regional group at 12.3%, compared to 9.3% in the general anesthesia group. Mortality rates were 1.7% for regional anesthesia and 0.9% for general anesthesia, indicating a slight increase in risk associated with regional anesthesia in this context (Figure 1, Table 1). The median length of hospital stay was identical for both groups, recorded at 7 days. However, the interquartile range (IQR) differed slightly, with regional anesthesia showing a range of 5 to 10 days, compared to 6 to 10 days for general anesthesia. The difference between the two groups was statistically non-significant, with a 95% confidence interval of 0 to 0, underscoring a similar duration of hospitalization regardless of the anesthesia type used (Figure 2, Table 2).
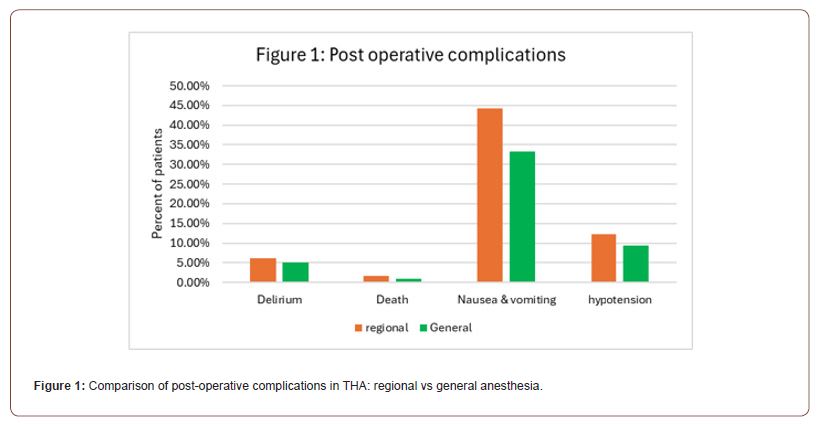
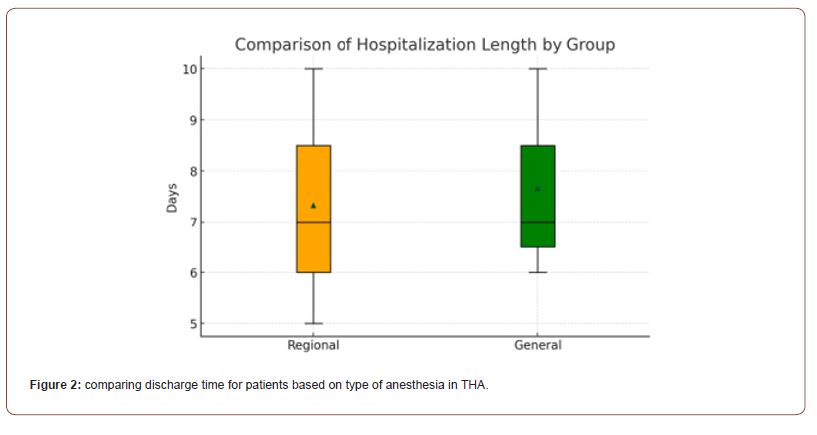
Table 1:Assessing the post-operative complications of THA involving regional vs general anesthesia.
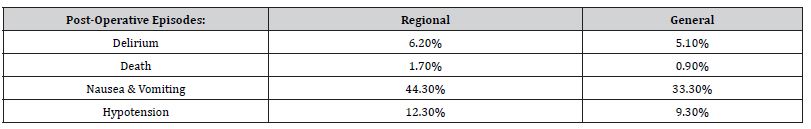
Table 2:Average discharge time for patients undergoing THA: general vs regional.
The results of the second randomized trial further supported general anesthesia as a technique for THA, however there were some caveats. In a comparative study of spinal and general anesthesia in total hip arthroplasty (THA) patients, the findings demonstrated specific advantages and disadvantages for each anesthesia type. Patients administered general anesthesia experienced shorter hospital stays, suggesting a quicker initial recovery. In contrast, those receiving spinal anesthesia were quicker to meet discharge criteria, indicating a potentially better quality of recovery in terms of readiness to leave the hospital, despite their longer stays. An evaluation of postoperative pain revealed that spinal anesthesia provided superior pain relief at 2 hours post-surgery, whereas general anesthesia was more effective at reducing pain 6 hours after surgery. This suggests that while spinal anesthesia offers immediate postoperative benefits, its analgesic effects diminish sooner than those of general anesthesia. Additionally, a higher proportion of patients who received general anesthesia expressed a preference for different anesthesia types for future procedures, hinting at lower satisfaction despite its advantages in reducing hospital stay and later postoperative pain. Furthermore, general anesthesia was associated with fewer complaints of nausea and dizziness, underscoring its efficacy in managing these side effects. These outcomes have been visually represented through bar graphs and line charts, highlighting the differences in recovery profiles and side effects between the two anesthesia types (Figure 3, Table 3).
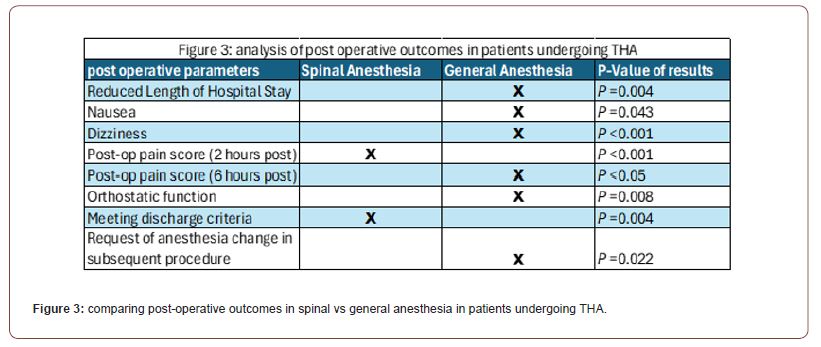
Table 3:Beta amyloid expression levels at different time points, pre and post THA.
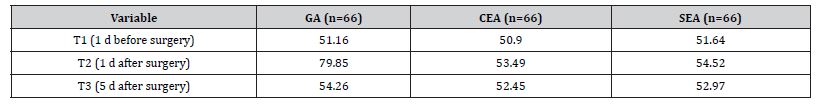
In contrast to the previous two studies, the third randomized controlled trial found general to be more detrimental after an extended period post-operation. study compared the effects of general anesthesia (GA) to two regional techniques: caudal epidural anesthesia (CEA) and spinal epidural anesthesia (SEA), in the context of total hip arthroplasty (THA). The study particularly focused on the expression levels of beta-amyloid (Aβ) as a potential biomarker associated with postoperative cognitive dysfunction, measured one day before surgery (T1), one day after surgery (T2), and five days after surgery (T3). The results indicated that the GA group showed a substantial increase in Aβ expression one day after surgery with a mean level of 79.85, which was significantly higher compared to the CEA and SEA groups, which presented mean levels of 53.49 and 54.52 respectively. This suggests a possible link between general anesthesia and a transient spike in Aβ expression, which could have implications for postoperative cognitive outcomes. However, five days after surgery (T3), the Aβ levels in the GA group had reduced to a mean level of 54.26, closely aligning with the levels observed in the CEA (52.45) and SEA (52.97) groups, suggesting a return to baseline expression akin to the regional anesthesia groups. At no point was a significant difference in Aβ expression observed between the CEA and SEA groups, indicating a potentially similar impact on cognitive markers when comparing these two regional anesthesia modalities (Figure 4, Table 4). In conjunction with evaluating beta-amyloid levels, the third RCT also focused on comparing pain levels among patients receiving general anesthesia (GA), caudal epidural anesthesia (CEA), and spinal epidural anesthesia (SEA) after total hip arthroplasty. Pain scores (0-10, 10 being worst pain) were systematically recorded at various intervals post-surgery: 3, 6, 9, 12, and 24 hours. Patients under GA reported higher pain scores consistently over the first 12 hours, with scores decreasing slightly by the 24-hour mark. Initially, at 3 hours post-surgery, the GA group’s pain score was the highest at 5.13, followed by SEA at 2.95, and CEA at 1.92, indicating that regional anesthesia techniques were more effective in managing immediate postoperative pain. This trend of regional anesthesia providing more effective pain control was consistent at the 6-hour mark, with CEA showing the lowest pain score of 1.2, SEA at 2.75, and GA remaining higher at 5.12. By the 9-hour interval, GA pain scores had marginally decreased to 4.91, while both regional methods, CEA and SEA, maintained lower scores at 1.13 and 1.49, respectively. At the 12-hour observation, GA continued to demonstrate the highest pain levels at 3.86, with SEA and CEA showing minimal pain scores of 1.34 and 1.16, respectively. At the 24-hour postoperative mark, all groups exhibited a slight increase in pain scores compared to the 12-hour mark, with GA at 4.38, SEA at 2.75, and CEA at 1.69. The data visually represented in a bar graph underscores that both CEA and SEA were more effective in controlling postoperative pain than GA, especially notable within the first 12 hours after surgery. Over time, while pain scores for patients under GA slightly improved, they remained higher compared to those who received regional anesthesia, suggesting a sustained advantage of regional techniques in managing postoperative pain in the acute phase following THA (Figure 5, Table 5).
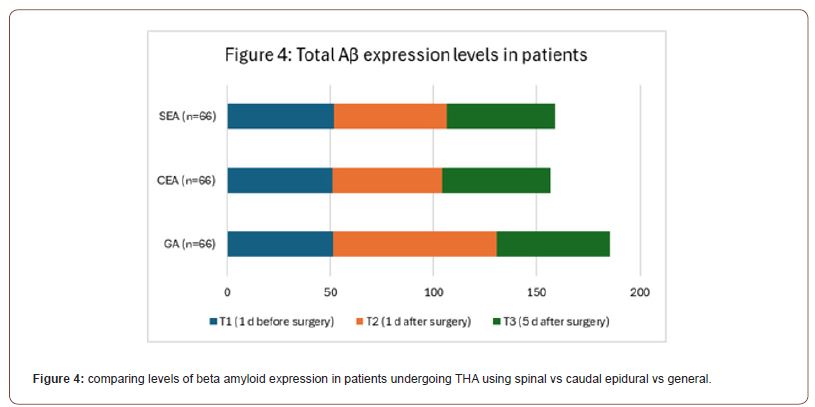
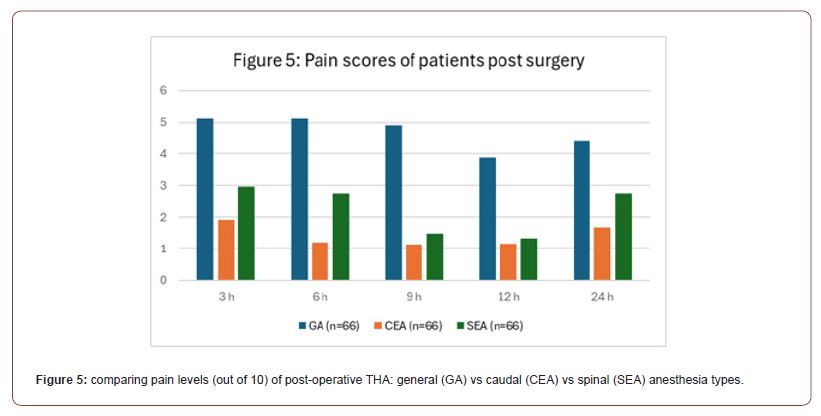
Table 4:Pain scores (out of 10) for patients undergoing THA using different types of anesthesia.
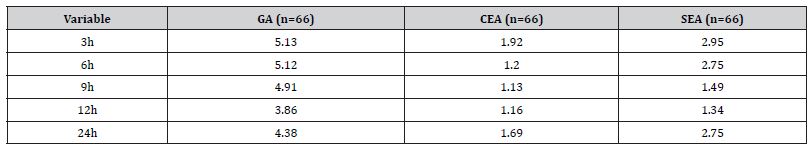
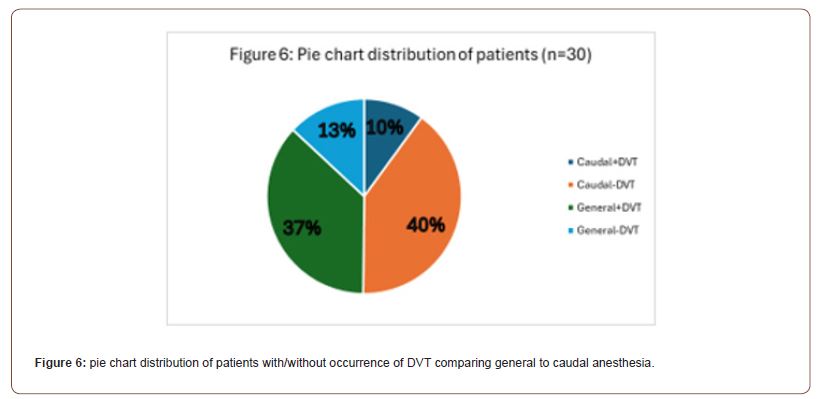
Table 5:Comparison of occurrence of deep vein thrombosis in patients undergoing THA using caudal vs general anesthesia.
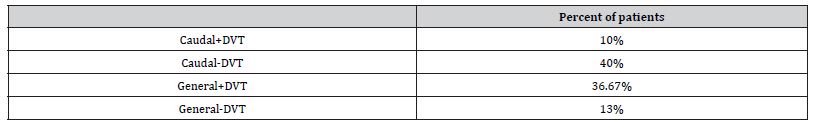
In the clinical trial aimed at assessing the incidence of deep vein thrombosis (DVT) in patients undergoing total hip arthroplasty (THA) with either caudal or general anesthesia, the results indicated a significant difference in DVT rates between the two groups. Out of the 30 patients studied, those who received caudal anesthesia exhibited a lower incidence of DVT, with only 10% of patients developing this complication postoperatively. In contrast, a notably higher percentage of patients who underwent general anesthesia, 36.67%, experienced DVT. The pie chart distribution emphasizes this disparity, showing that while the majority (40%) of patients who received caudal anesthesia did not develop DVT, a lesser proportion of patients in the general anesthesia group (13%) remained DVT-free (Figure 6). These findings suggest that regional anesthesia may be associated with a reduced risk of postoperative DVT compared to general anesthesia in the context of THA.
Conclusion
The series of randomized controlled trials and a clinical trial reviewed in this paper offer valuable insights into the comparative effects of general and regional anesthesia on postoperative outcomes in total hip arthroplasty (THA) and confirm the results of the Meta-Analysis performed in 2019. Collectively, the findings suggest that while general anesthesia may provide certain shortterm benefits, regional anesthesia techniques, including spinal and caudal epidural, appear to offer superior postoperative outcomes in several key areas.
From the first RCT, regional anesthesia showed promise in reducing the incidence of postoperative delirium and other complications, albeit with a slightly increased risk of hypotension. The second RCT highlighted the effectiveness of regional anesthesia in controlling immediate postoperative pain and enhancing discharge readiness, despite general anesthesia’s advantage in reducing hospital stay and later postoperative pain levels. The third RCT brought to light a potentially important consideration: the higher levels of beta-amyloid expression associated with general anesthesia, which may have implications for cognitive outcomes in the postoperative period.
Moreover, the clinical trial provided a critical perspective on the risk of deep vein thrombosis (DVT), a serious and common postoperative complication. The reduced incidence of DVT in patients receiving caudal anesthesia underscores the potential benefits of regional anesthesia in thromboembolic prophylaxis.
Taken together, these studies reinforce the necessity of individualized anesthesia management in THA. They emphasize the importance of considering a multitude of factors, including the patient’s risk profile for cognitive and thromboembolic complications, postoperative pain management needs, and overall recovery trajectory. While regional anesthesia techniques show considerable advantages in several domains, general anesthesia still has its place, particularly in scenarios where it may be specifically indicated or preferred.
It is important to consider a few limitations with this review. Notably, the sample size and heterogeneity of the anesthesia techniques could potentially create confounding variables that future studies can focus on mitigating. As suggested by the Meta- Analysis, future research should continue to refine these findings, integrating larger patient cohorts and diverse demographics to fully understand the long-term implications of anesthesia type on THA outcomes. For now, the evidence presented supports a nuanced approach to anesthesia in THA, advocating for patientcentered care that tailors anesthesia choice to the unique needs of each patient to optimize recovery and minimize complications.
Acknowledgement
None.
Conflict of Interest
Conflict of Interest
References
- Tsakiris, Violeta, Christu Tardei, Florentina Marilena Clicinschi (2021) Biodegradable Mg Alloys for Orthopedic Implants – A Review. Journal of Magnesium and Alloys 9(6): 1884-1905.
- Kotrych, Daniel, Andrea Angelini, Andrzej Bohatyrewicz, Pietro Ruggieri (2023) 3D Printing for Patient-Specific Implants in Musculoskeletal Oncology. EFORT Open Reviews 8(5): 331-339.
- Pérez, Mercedes, Diego Carou, Eva María Rubio, Roberto Teti (2020) Current Advances in Additive Manufacturing. Procedia CIRP 88: 439-444.
- Rendas, Pedro, Lígia Figueiredo, Ricardo Cláudio, Catarina Vidal, Bruno Soares, et al. (2023) Investigating the Effects of Printing Temperatures and Deposition on the Compressive Properties and Density of 3D Printed Polyether ketone. Progress in Additive Manufacturing.
- Meng, Meng, Jinzuo Wang, Huagui Huang, Xin Liu, Jing Zhang, et al. (2023) 3D Printing Metal Implants in Orthopedic Surgery: Methods, Applications and Future Prospects. Journal of Orthopaedic Translation 42: 94-112.
- Liverani, Erica, Giulia Rogati, Stefania Pagani, Silvia Brogini, et al. (2021) Mechanical Interaction between Additive-Manufactured Metal Lattice Structures and Bone in Compression: Implications for Stress Shielding of Orthopaedic Implants. Journal of the Mechanical Behavior of Biomedical Materials 121: 104608.
- Serrano-Aroca Ángel, Alba Cano-Vicent, Roser Sabater I Serra, Mohamed El-Tanani, Alaa AA Aljabali, et al. (2022) Scaffolds in the Microbial Resistant Era: Fabrication, Materials, Properties and Tissue Engineering Applications. Materials Today Bio 16:100412.
- Zhou, Keran, Farah Alwani Azaman, Zhi Cao, Margaret Brennan Fournet, and Declan M. Devine. 2023. Bone Tissue Engineering Scaffold Optimisation through Modification of Chitosan/Ceramic Composition. Macromol 3(2): 326-342.
- Jiang, Dayue, Fuda Ning, and Ying Wang (2021) Additive Manufacturing of Biodegradable Iron-Based Particle Reinforced Polylactic Acid Composite Scaffolds for Tissue Engineering. Journal of Materials Processing Technology 289: 116952.
- Shao Hanyu, Qiyue Zhang, Mingman Sun, Ming Wu, Xu Sun, et al. (2023) Effects of Hydroxyapatite-Coated Porous Titanium Scaffolds Functionalized by Exosomes on the Regeneration and Repair of Irregular Bone. Frontiers in Bioengineering and Biotechnology 11:1283811.
- Marin, Elia, and Alex Lanzutti (2024) Biomedical Applications of Titanium Alloys: A Comprehensive Review. Materials 17(1): 114.
- Kadi, Fatima, Ghasem Dini, S. Ali Poursamar, and Fatemeh Ejeian. (2024) Fabrication and Characterization of 3D-Printed Composite Scaffolds of Coral-Derived Hydroxyapatite Nanoparticles/Polycaprolactone/Gelatin Carrying Doxorubicin for Bone Tissue Engineering. Journal of Materials Science. Materials in Medicine 35(1): 7.
- Filippi, Miriam, Gordian Born, Mansoor Chaaban, Arnaud Scherberich (2020) Natural Polymeric Scaffolds in Bone Regeneration. Frontiers in Bioengineering and Biotechnology 8.
- Wu Yi-Fan, Ya-Ting Wen, Eisner Salamanca, Lwin Moe Aung, Yan-Qiao Chao, et al. (2024) 3D-Bioprinted Alginate-Based Bioink Scaffolds with β-Tricalcium Phosphate for Bone Regeneration Applications. Journal of Dental Sciences 19(2): 1116-1125.
- M Arshad, N Khoramshahi, G Shirani (2023) Additively custom‐made 3D‐printed subperiosteal implants for the rehabilitation of the severely atrophic maxilla (a case report). Clin. Case Reports 11(11): 1-8.
- P Balamurugan, N Selvakumar (2021) Development of patient specific dental implant using 3D printing. In: J Ambient, Intell Humaniz (Eds.,) Comput 12(3): 3549-3558.
- F P Moncayo-Matute, E Vázquez-Silva, P G Peña-Tapia, P B Torres-Jara, D P Moya-Loaiza, et al. (2023) Finite Element Analysis of Patient-Specific 3D-Printed Cranial Implant Manufactured with PMMA and PEEK: A Mechanical Comparative Study. Polymers (Basel) 15(17): 3620.
- F Danielli, L Ciriello, L La Barbera, J F Rodriguez Matas, G Pennati (2023) On the need of a scale-dependent material characterization to describe the mechanical behavior of 3D printed Ti6Al4V custom prostheses using finite element models. J Mech Behav Biomed Mater 140: 105707.
- M Rana, S Karmakar, A Bandyopadhyay, A Roychowdhury (2023) Design and manufacturing of patient-specific Ti6Al4V implants with inhomogeneous porosity. J Mech Behav Biomed Mater 143: 105925.
- S Ciklacandir, S Mihcin, Y Isler (2022) Detailed Investigation of Three-Dimensional Modeling and Printing Technologies from Medical Images to Analyze Femoral Head Fractures Using Finite Element Analysis. Irbm 43(6): 604-613.
- A Ouldyerou, L Aminallah, A Merdji, A Mehboob, H Mehboob (2023) Finite element analyses of porous dental implant designs based on 3D printing concept to evaluate biomechanical behaviors of healthy and osteoporotic bones. Mech Adv Mater Struct 30(11): 2328-2340.
- F Haque, A F Luscher, K A S Mitchell, A Sutradhar (2023) Optimization of Fixations for Additively Manufactured Cranial Implants: Insights from Finite Element Analysis. Biomimetics 8(6).
- A Vautrin, J Aw, E Attenborough, P Varga (2023) Fatigue life of 3D-printed porous titanium dental implants predicted by validated finite element simulations. Front Bioeng Biotechnol 11: 1-11.
- H Ma, S Xu, X Ju, A Tang, X Hu (2023) Finite Element Analysis of Renewable Porous Bones and Optimization of Additive Manufacturing Processes. Coatings 13(5).
- E Savran, OC Kalay, NB Alp, F Karpat (2023) Design and analysis of lattice structure applied humerus semi-prosthesis. Materials Testing 7(65).
- U L Lee, J Y Lim, S N Park, B H Choi, H Kang, et al. (2020) A clinical trial to evaluate the efficacy and safety of 3d printed bioceramic implants for the reconstruction of zygomatic bone defects. Materials (Basel) 13(20): 4515.
- F A De Souza, M C Blois, K Collares, M B F Dos Santos (2024) 3D-printed and conventional provisional single crown fabrication on anterior implants: A randomized clinical trial. Dent Mater 40(2): 340-347.
- C Anunmana, C Ueawitthayasuporn, S Kiattavorncharoen, P Thanasrisuebwong (2020) In vitro comparison of surgical implant placement accuracy using guides fabricated by three different additive technologies. Appl Sci 10(21): 1-11.
- C M De Almeida Malzoni, V Gonçalves, J Possari, E M Junior (2022) The use of 3D ceramic block graft compared with autogenous block graft for rehabilitation of the atrophic maxilla: a randomized controlled clinical trial. Trials 23(1): 903.
- B Liu, et al. (2022) Mechanical Distribution and New Bone Regeneration After Implanting 3D Printed Prostheses for Repairing Metaphyseal Bone Defects: A Finite Element Analysis and Prospective Clinical Study. Front Bioeng Biotechnol 10(6): 1-10.
-
Farhood Salehi*, Maamoon Mian and Cooper Phillips. Comparative Efficacy of General and Regional Anesthesia in Total Hip Arthroplasty: A Comprehensive Review. Anaest & Sur Open Access J. 5(1): 2024. ASOAJ.MS.ID.000603.
-
General anesthesia, Nausea, Regional Anesthesia, Orthopedic surgeon, Surgeries, Regional anesthesia, Postoperative pain, Total Hip Arthroplasty
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






