 Case Report
Case Report
Chronic Pacemaker Pocket Pain Treated Successfully with A Pectoralis Nerve Block
Sadie Smith* and Rajeev Dalal
Department of Anesthesiology & Perioperative Medicine, Penn State Health, USA
Sadie Smith, Department of Anesthesiology & Perioperative Medicine, Penn State Health, USA.
Received Date: December 08, 2021; Published Date:January 11, 2022
Introduction
The pectoralis nerve block (PECs I and II) was first described in 2011 to provide analgesia after breast surgery [1]. PECs I targets the plane between the pectoralis major and minor to anesthetize the medial and lateral pectoral nerves. PECs II targets the plane between the pectoralis minor and serratus anterior to anesthetize intercostal nerves, long thoracic nerve, and intercostobrachial nerve. The most common indication for a PECs block is postoperative analgesia for breast surgery, and very few case reports describes its use for treatment of chronic chest wall pain [1,2].
In this report, we will the use of a PECs I block to treat intractable neuropathic chronic pacemaker pocket pain. Late complications after pacemaker placements are low, and late development of chronic pacemaker pocket pain is an uncommon complication from pacemaker implantations. Chronic pacemaker pocket pain is theorized by some to be due fascial and skin erosion in sub adipose tissue pacemaker placements. For this reason, pacemaker pocket revision in favor of creating a subpectoral pacemaker pocket is often the treatment of pacemaker pocket pain [3,4].
We describe a patient with severe chronic pacemaker pocket pain, who had exhausted conservative treatments such as over the counter analgesics, topical agents, and gabapentinoids. His goal was to avoid a pacemaker pocket revision, as the pocket itself looked appropriate, despite his level of pain. We performed a successful PECs I block multiple times with significant pain relief, allowing for increased functionality and improved quality of life.
Case Report
A 67-year-old male with history of coronary artery disease status post coronary artery bypass graft and pacemaker placement in 2017 initially presented to his family physician with 4–5-month history of pain and redness at his pacemaker site located in the left infraclavicular space. He was given a course of antibiotics which did not improve his symptoms. He was trialed on gabapentin without relief. He was started on oxycodone-acetaminophen which mildly improved the pain. He was also referred to cardiology and electrophysiology who recommended a full workup including labs, blood cultures, CXR, cervical spine XR, SPECT CT, and TEE. His lab work revealed elevated ESR 32 and CRP 12.6. The rest of the workup was negative and was referred to the chronic pain management clinic for further evaluation.
Upon his initial chronic pain visit in November 2020, he described a 4-5 month history of sharp, stabbing, non-radiating, 9/10 pain and redness at his left sided pacemaker site. Certain movements particularly lifting his left arm aggravated the pain, and only oxycodone-acetaminophen relieved the pain. On physical examination, there was pain with raising his left arm above his shoulder, some allodynia overlying the pacemaker, few trigger points over his left trapezius, and tenderness over trapezius and left cervical paraspinal musculature. There was no erythema, increased skin warmth, or hair loss; the reminder of the exam was negative. He was advised to use heat overlying his shoulder and neck for significant myofascial pain, use over the counter topical lidocaine over the pacemaker site, and create a pain journal. He was also counseled on transitioning away from opioids and instead use Tylenol 1000 mg TID.
At his 4 week follow up, the lidocaine patch significantly improved his pacemaker pain while on his skin, but his pain returned to baseline when the patch was off. Heat helped with myofascial pain in his neck and shoulder, but this was not his primary concern. He continued to use Tylenol and no longer used oxycodone-acetaminophen. Due to his persistent and severe, chronic pacemaker pain, he was scheduled for an ultrasound guided left pectoralis nerve block with local anesthetic and steroid in January 2021.
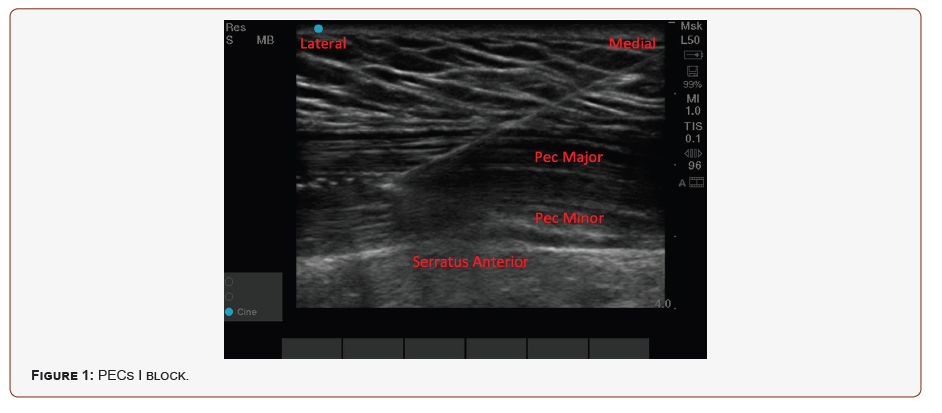
An informed consent was obtained. The patient was identified by the staff and attending physician. Appropriate patient monitors were placed for the procedure. The patient was positioned supine with left arm slightly abducted on the procedure bed. The skin over the left axilla and chest wall was prepped and draped in a sterile fashion using chlorhexidine. A surgical time-out was performed and agreed upon by members of the team. Ultrasound using the linear probe was used to identify the left chest wall and surrounding relevant structures including pectoralis major and pectoralis minor. The skin and subcutaneous tissues were anesthetized using 1% lidocaine and a 25-gauge 1-1/2 inch needle.
A 4” stimuplex needle was then inserted, visualized, and advanced in an in-plane fashion beneath the linear probe. It was visualized to reach the fascial plane between the pectoralis major and minor muscles, as shown in (Figure 1). After negative aspiration, a small amount of normal saline was injected for hydro dissection. After negative aspiration of blood, a mixture containing 10 mg of dexamethasone and 9mL of 0.25% bupivacaine (total 10 mL injectate) was injected in the sheath separating the pectoralis major from pectoralis minor muscle. The needle was then removed. The patient tolerated the procedure well and there were no complications.
The patient followed up about two months following his left sided PECs I nerve block in March 2021. It was a telephone visit due to the COVID-19 pandemic. He reported a 100% pain relief from his pacemaker pain and regained full range of motion in his left shoulder. He experienced a 5-6 month period of significant pain relief before the pain returned. Subsequently, he underwent a repeat procedure in July 2021. He underwent a repeat procedure and received a 3-4 day pain relief, but no longer had sharp pain or allodynia overlying his pacemaker pocket site. Instead, he developed new onset myofascial pain in his pectoralis major muscle between his pacemaker and clinic, which is being managed in our clinic. His pain unfortunately returned and a third block was performed in November 2021 and was set to follow up in 4-6 weeks.
Discussion
Here we describe a case of chronic pacemaker pocket pain successfully treated with PECs I block multiple times. Upon initial consultation, the patient was thought to suffer from severe myofascial pain that was exacerbated by his pacemaker, in addition to neuropathic burning pain overlaying the pacemaker. He continued to experience severe chest wall pain despite multiple treatment modalities on his follow up visit. He underwent a PECs I block to relieve his pain, which has not been performed before in this specific patient population. The block itself was technically challenging due to the pacemaker interfering with the position of the ultrasound probe and thus required patient cooperation and additional superficial local anesthetic. However, the patient received more than anticipated duration of pain relief with this block and regained his functional capabilities. In summary, PECs block can serve as an effective, opioid-sparing, treatment in patients with chest wall discomfort, including neuropathic chronic pacemaker pocket pain.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Blanco R (2011) The ‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia 66(9): 847-848.
- Blanco R, Fajardo M, Parras Maldonado T (2012) Ultrasound description of Pecs II (modified Pecs I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim 59(9): 470-475.
- Kistler PM, Fynn SP, Mond HG, Eizenberg N (2004) The subpectoral pacemaker implant: it isn’t what it seems!. Pacing Clin Electrophysiol PACE 27(3): 361-364.
- Harcombe AA, Newell SA, Ludman PF (1998) Late complications following permanent pacemaker implantation or elective unit replacement. Heart 80(3): 240-244.
-
Sadie Smith, Rajeev Dalal. Chronic Pacemaker Pocket Pain Treated Successfully with A Pectoralis Nerve Block. Anaest & Sur Open Access J. 3(1): 2022. ASOAJ.MS.ID.000555.
-
Pacemaker, Pain, Analgesia, Breast surgery, Pectoralis nerve block (PECs).
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






