 Case Report
Case Report
Cefepime Induced Encephalopathy: A Case Report
Bouaiyda A*, Ababou M, Jeddab A, Chouikh C, Mounir KH and Balkhi H
Department of Anesthesiology and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Morocco
Bouaiyda Ayoub, Department of Anesthesiology and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Morocco.
Received Date: December 01, 2021; Published Date:January 03, 2022
Abstract
Cefepime is a 4th cephalosporin generally widely used in the treatment of nosocomial bacterial infections. However, despite its clinical and therapeutic efficacy, many adverse events have been reported since its use began, varying in severity and importance. We will report the case of a patient who presented a deterioration of his state of consciousness postoperatively of a subdural hematoma and whose diagnostic investigations came back in favor of a cefepime induced encephalopathy.
Keywords:Cefepime; Encephalopathy; Neurotoxicity
Abbreviations:INR: international Normalized Ratio; PT: Prothrombin Time; ICU: Intensive Care Unit; EEG: Electroencephalogram
Introduction
Cefepime is a 4th generation cephalosporin that is part of the therapeutic arsenal for nosocomial infections. Its broad spectrum allows it to neutralize the majority of gram-negative bacilli. Nevertheless, like any medication, it is not without undesirable effects. Drug-induced encephalopathy is one of the rare complications of cefepime administration. We will report the case of a patient admitted to the intensive care unit for postoperative management of a subdural hematoma who developed cefepime drug encephalopathy during his stay.
Case Presentation
This was an 85-year-old patient with a history of atrial fibrillation on acenocoumarol, who was admitted with an apyretic picture of consciousness. The history of the disease dates back to 3 days prior to his admission where the patient suffered a fall from his height in the bathroom with a cranial impact point without initial loss of consciousness. Two days later, the patient suddenly developed a disorder of consciousness and was admitted to the emergency room. The clinical examination of the patient found an unconscious patient with a Glasgow score of 9/15 on verbal and motor response, pupils in anisocoria, capillary blood glucose at 0.90 g/l, blood pressure at 190/110 mm Hg, and heart rate at 110 bpm, saturation at 98% on room air with auscultation a few snoring sounds on the right.
In view of this clinical picture, a cerebral CT scan without injection was requested, which came back in favor of an acute left fronto-parieto-occipital subdural hematoma with a meningeal hemorrhage and a subfalcoral involvement deviating the median line. Biological tests showed a hemoglobin level of 14.1 g/dl, a platelet count of 230,000 elements/mm3, a prothrombin level of 14% and an INR of 4. The patient received 10 mg of vitamin K, transfusion of 8 bags of fresh frozen plasma with an INR control of 1.2 and a PT of 68% and was admitted to the operating room. The procedure consisted of evacuation of the hematoma, careful hemostasis with placement of redon drains. He was then transferred to the intensive care unit for further management.
During his stay in the ICU, the patient remained intubated for 5 days, then extubated after a favorable control CT scan and a complete awakening after the sedation was stopped on the 6thèmeday. During his stay, the patient developed a pneumonia linked to multi-resistant Klebsiella pneumonia treated with cefepime 6g/d administered in an electric syringe pump. The patient was subsequently transferred to neurosurgery for further care.
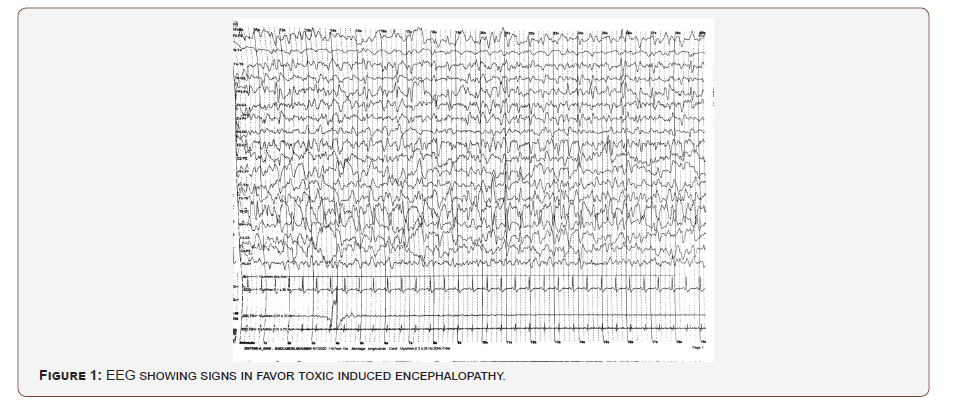
At D3 of his stay in neurosurgery the patient presented an alteration of his consciousness, hence his readmission in intensive care, a scanner to eliminate a recurrence came back stationary, the biological assessment was without anomalies, in front of this diagnostic dilemma an electroencephalogram was performed, and which objectified the presence of signs in favor of a drug-induced encephalopathy [Figure 1].
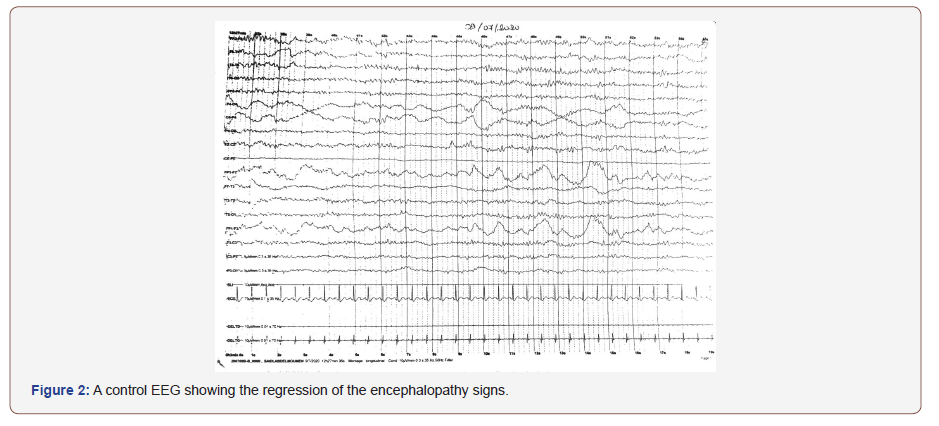
The patient was under cefepime, curative anticoagulation with enoxaparin and gastric protection with omeprazole. Thus, in view of these data and given the totality of 7 days of treatment, the clinical and biological improvement of the patient, it was decided to stop the antibiotic therapy. The evolution was marked by the improvement of the patient’s state of consciousness the next day with a favorable electroencephalographic control [Figure 2], and the diagnosis of cefepime drug-induced encephalopathy was thus retained.
Discussion
Cefepime is a 4th generation cephalosporin with a broad spectrum, it is active on the family of enterobacteria, pseudomonas aeruginosa as well as having an anti-gram positive activity comparable to that of 1st errand 2nd generation cephalosporins [1]. Unfortunately, despite its therapeutic efficacy, it is not without undesirable effects, particularly neurotoxicity [2].
The clinical presentations of neurotoxicity are polymorphic, with several clinical forms found in the literature: simple decreased consciousness, confusion, agitation, global aphasia, myoclonus, choreoathetoid movements, convulsions and coma [3]. Data suggest that up to 15% of intensive care unit patients treated with cefepime may experience these adverse events. Risk factors include renal dysfunction, excessive dose, pre-existing brain injury, and high serum cefepime concentrations [4]. The mechanism of neurotoxicity is not completely established, it is suggested that it is related to the concentration-dependent competitive antagonism of ϒ-aminobutyric acid (GABA) which leads to an overexcitation of the electrical activity of neurons and the appearance of neurological symptoms, including seizures [5]. Recently, hypocarnitinemia has been reported as a possible trigger for neurotoxicity, due to blockage of a renal transporter, OCTN2, which is a cation/carnitine pump that results in significant renal carnitine loss [6].
The diagnosis is based on a combination of arguments combining the presence of cefepime as a triggering factor, the presence of the risk factors mentioned and the signs of toxic metabolic encephalopathy on the EEG [7]. Discontinuation or reduction of the dose is sufficient to restore the situation. In the case of our patient, he had as a risk factor the subdural hematoma operated as a pre-existing lesion, the administration of cefepime at high dose, the EEG showed neurophysiological signs in favor with a total regression of the symptoms after the cessation of the administration observed also on his EEG of control
Conclusion
Cefepime-related encephalopathy remains a rare complication, most often related either to high-dose administration or in a patient with risk factors, the evolution is often favorable in the majority of cases after discontinuation of the administration but sometimes can be fatal, so in front of any patient on cefepime who presents a deterioration of his neurological state, it is always necessary to think about questioning its use or adapting the doses according to the benefit/risk.
Acknowledgements
AB, MA, and AJ examined the patient and drafted the manuscript. HB evaluated the findings and gave important clinical opinions. CC and MK participated in the design of the case report and helped to draft the manuscript. All author’s read and approved the final manuscript.
Conflict of interest
The authors declare no competing interests.
References
- Okamoto MP, Nakahiro RK, Chin A, Bedikian A (1993) Cefepime clinical pharmacokinetics. Clin Pharmacokinet 25(2): 88-102.
- Boschung-Pasquier L, Atkinson A, Kastner LK, Banholzer S, Haschke M, et al. (2020) Cefepime neurotoxicity: thresholds and risk factors. A retrospective cohort study. Clin Microbiol Infect 26(3): 333-339.
- Sonck J, Laureys G, Verbeelen D (2008) The neurotoxicity and safety of treatment with cefepime in patients with renal failure. Nephrology Dialysis Transplantation 23(3): 966-970.
- Je F, Ea K, Se H, Sl C, Ef W, et al. (2013) Cefepime neurotoxicity in the intensive care unit: a cause of severe, underappreciated encephalopathy. Critical care 17(6): R264.
- Durand-Maugard C, Lemaire-Hurtel A-S, Gras-Champel V, Hary L, Maizel J, et al. (2012) Blood and CSF monitoring of cefepime-induced neurotoxicity: nine case reports. J Antimicrob Chemother 67(5): 1297-1299.
- Fernández-Fernández FJ, Ameneiros-Lago E (2020) Cefepime-Induced Encephalopathy: Could Carnitine Deficiency Contribute to Neurotoxicity? Neurohospitalist 10(2): 81.
- Tamune H, Hamamoto Y, Aso N, Yamamoto N (2019) Cefepime-induced encephalopathy: Neural mass modeling of triphasic wave-like generalized periodic discharges with a high negative component (Tri-HNC). Psychiatry Clin Neurosci 73(1): 34-42.
-
Bouaiyda A, Ababou M, Jeddab A, Chouikh C, Mounir KH, Balkhi H. Cefepime Induced Encephalopathy: A Case Report. Anaest & Sur Open Access J. 3(1): 2022. ASOAJ.MS.ID.000554.
-
Bacterial infections, Neurosurgery, Cefepime, Gram-negative bacilli, Cephalosporins
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






