 Case Report
Case Report
Asymptomatic Double Aortic Arch in An Adult That Progressed to Dysphagia
Obiora Ezeudemba*
Department of Internal Medicine, St Vincent medical center, Bridgeport Connecticut, USA
Obiora Ezeudemba, Department of Internal Medicine, Department of Internal Medicine, St Vincent medical center, Bridgeport Connecticut, USA.
Received Date: February 02, 2023; Published Date: February 16, 2023
Introduction
The double aortic arch (DAA) is a rare congenital vascular anomaly representing 1% of congenital heart disease [1]. It forms an anatomical vascular ring that encircles the thoracic portions of the trachea and esophagus. Typically, it is diagnosed in the neonatal period, often presenting with dyspnea or dysphagia due to tracheal and esophageal compression, respectively [1]. However, asympto matic DAA’s are known to persist into adulthood. In these cases, they are often incidentally diagnosed [2-5], but they can also reveal themselves with delayed onset of the compressive symptoms [6-8]. We report the case of a 49-year-old female with a previously diagnosed asymptomatic DAA that later became symptomatic with dysphagia requiring surgical relief.
Case Presentation
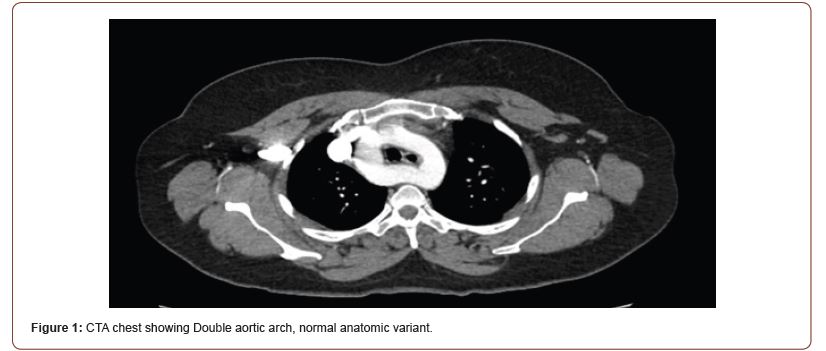
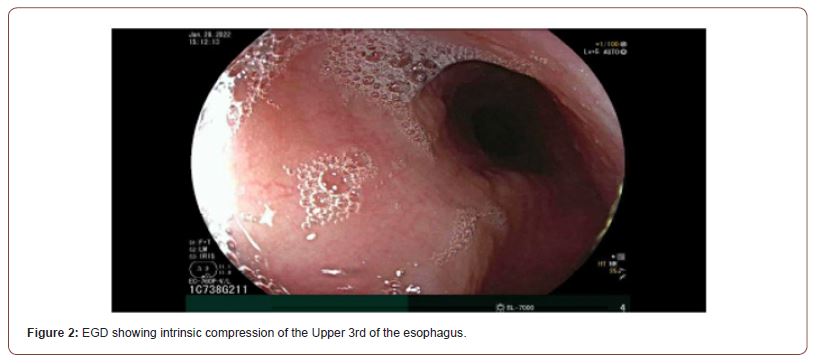
A 49-year-old female with a known history of DAA now presenting with dysphagia to solid food. The patient’s DAA was diagnosed incidentally when she presented with pleuritic chest pain and shortness of breath. At that time there were concerns for pulmonary embolism, so she underwent a CTA chest which revealed a DAA with co-dominance of the left and right aortic branches. Given the patient’s lack of symptoms, the decision was made to not pursue further work up or treatment [Figure 1]. However, over a course of years, the patient started having dysphagia with a sense of food getting stuck on her esophagus causing a persistent pain around the xiphoid area. She had an EGD, which showed extrinsic compression of the esophagus [Figure 2].
Discussion
Aortic arch anomalies include the vascular ring. DAA, a subtype representing 25-38% of rings therein [9-11], was first described by Wollman in 1939 and surgically corrected by Gross in 1945 [12, 13]. It results from improper embryologic development of the fourth aortic arches. Edwards’ Hypothetical Double Arch model illustrates how failure of the hypothetical right arch to involute results in persistence of the bifurcated ascending aorta. The left and right arch each course around opposite sides of the trachea and esophagus before rejoining to form the descending aorta, which is still typically left-sided [14]. Diagnosis is often made in the neonatal period, usually informed by respiratory symptoms such as stridor, wheezing, and coughing, which are almost always present, and in some cases, will co-present with gastrointestinal symptoms, primarily choking with feeds [1, 9, 15, 16]. Importantly, DAA usually occurs without associated cardiac anomalies [15, 16]. Accordingly, treatment outcomes are excellent in pediatric populations after surgical correction [15, 17].
The question of surgical treatment arises when DAA presents asymptomatically. In an era of widespread use of cross-sectional imaging modalities, these cases are becoming more common [2-5]. A conservative approach would be to monitor these patients for the development of compressive symptoms and only then surgically correct them. However, life-threatening complications of otherwise asymptomatic DAA have been described. Notably, prolonged nasogastric intubation in these patients can lead to ulceration and subsequent arterial-esophageal fistula formation [18-20]. These fistulae can harbor life-threatening infections and even lead to massive upper gastrointestinal bleeds with subsequent death by exsanguination. Thus, even a completely asymptomatic DAA can contribute to morbidity and mortality. The patient described in this case had her DAA incidentally diagnosed nearly ten years before it became symptomatic. Her close monitoring and follow-up within the same system facilitated targeted workup and prompt surgical correction once her compressive symptoms finally manifested.s
Conclusion
DAA is a diagnosis that is classically described within the context of pediatric cardiology. However, widespread use of cross-sectional imaging has identified an increasing number of asymptomatic adult cases. Thus, DAA remains relevant in fields of adult medicine, particularly gastroenterology. We have outlined a case wherein close monitoring and follow-up successfully mitigated dysphagia-related morbidity and avoided redundant workup. It highlights the importance of viewing asymptomatic DAA as more than a benign anatomical variant. Future studies into incidentally diagnosed DAA would be useful to explore a possible risk reduction in their morbidity and mortality through subsequent scheduled monitoring.
Acknowledgments
None.
Conflict of Interest
None.
References
- Licari A, Manca E, Rispoli GA, Mannarino S, Pelizzo G, et al. (2015) Congenital vascular rings: a clinical challenge for the pediatrician. Pediatr Pulmonol 50(5): 511-524.
- Akhondi A, Ruehm SG, Tabibiazar R, Yang EH (2014) Incidental diagnosis of a double aortic arch during an acute myocardial infarction. Tex Heart Inst J 41(5): 564-566.
- Iida Y, Ito T, Misumi T, Shimizu H (2017) Silent balanced double aortic arch with descending thoracic aneurysm in an elderly patient. J Vasc Surg 65(6): 1823.
- Settepani F, Cappai A, Basciu A, Barbone A, Tarelli G (2015) Balanced Double Aortic Arch in an Older Patient. Ann Thorac Surg 99(6): 2221.
- Seo HS, Park YH, Lee JH, Hur SC, Ko YJ, et al. (2011) A case of balanced type double aortic arch diagnosed incidentally by transthoracic echocardiography in an asymptomatic adult patient. J Cardiovasc Ultrasound 19(3): 163-166.
- Barbara DW, Broski SM, Patch RK, Pochettino A (2017) Double Aortic Arch Causing Severe Tracheal Compression. Anesthesiology 126(2): 326-326.
- Monica Fernandez-Valls, Javier Arnaiz, Dickson Lui, Maria Elena Arnaiz-Garcia, Ana Canga, et al. (2012) Double Aortic Arch Presents With Dysphagia as Initial Symptom. J Am Coll Cardiol 60(12): 1114.
- Olearchyk AS (2004) Right-sided double aortic arch in an adult. J Card Surg 19(3): 248-251.
- Humphrey C, Duncan K, Fletcher S (2006) Decade of experience with vascular rings at a single institution. Pediatrics 117(5): e903-908.
- Woods RK, Sharp RJ, Holcomb GW 3rd, Snyder CL, Lofland GK, et al. (2001) Vascular anomalies and tracheoesophageal compression: a single institution's 25-year experience. Ann Thorac Surg 72(2): 434-438; discussion 438-439.
- Yu D, Guo Z, You X, Peng W, Qi J, et al. (2022) Long-term outcomes in children undergoing vascular ring division: a multi-institution experience. Eur J Cardiothorac Surg 61(3): 605-613.
- Wolman IJ (1939) Syndrome of constricting double aortic arch in infancy: report of a case. J Pediatr 14: 527–533.
- Gross RE (1945) Surgical relief for tracheal obstruction from a vascular ring. N Engl J Med 233: 586-590.
- Stojanovska J, Cascade PN, Chong S, Quint LE, Sundaram B (2012) Embryology and imaging review of aortic arch anomalies. J Thorac Imaging 27(2): 73-84.
- Alsenaidi K, Gurofsky R, Karamlou T, Williams WG, McCrindle BW (2006) Management and outcomes of double aortic arch in 81 patients. Pediatrics 118(5): e1336-1341.
- Backer CL, Mavroudis C, Rigsby CK, Holinger LD (2005) Trends in vascular ring surgery. J Thorac Cardiovasc Surg 129(6): 1339-1347.
- Ruzmetov M, Vijay P, Rodefeld MD, Turrentine MW, Brown JW (2009) Follow-up of surgical correction of aortic arch anomalies causing tracheoesophageal compression: a 38-year single institution experience. J Pediatr Surg 44(7): 1328-1332.
- Edwards BS, Edwards WD, Connolly DC, Edwards JE (1984) Arterial-esophageal fistulae developing in patients with anomalies of the aortic arch system. Chest 86(5): 732-735.
- Massaad J, Crawford K (2008) Double aortic arch and nasogastric tubes: a fatal combination. World J Gastroenterol. 14(16): 2590-2592.
- Minyard AN, Smith DM (2000) Arterial-esophageal fistulae in patients requiring nasogastric esophageal intubation. Am J Forensic Med Pathol 21(1): 74-78.
-
Obiora Ezeudemba*. Asymptomatic Double Aortic Arch in An Adult That Progressed to Dysphagia. Anaest & Sur Open Access J. 3(5): 2023. ASOAJ.MS.ID.000575.
-
Double Aortic Arch, congenital heart disease, chest pain, shortness of breath, dysphagia, aortic arches
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






