 Research Article
Research Article
Total Knee Replacement Done by A Single Surgeon with a Single Implant Design
W. Andrew Hodge1*, Janelle Garnique2 and Ronald Gardner3
1Adjunct Professor, University of South Florida, Tampa, FL, USA
2Tampa, FL, USA
3Founder, Gardner Orthopedics, Ft Myers, FL, USA
W. Andrew Hodge, Adjunct Professor, University of South Florida, Tampa, USA
Received Date:February 15, 2025; Published Date:February 26, 2025
Abstract
Historically, patient satisfaction following knee replacement surgery (TKA) has been suboptimal, many times falling below 85%. This study hypothesized that with consistent surgical practices and implant selection, that not only would patient satisfaction improve, but in addition, patient reported outcome measures (PROMs=KOOS & KSS), implant survivorship, implant placement and radiolucency would also get better. This study (247 patients) analysed surgical outcomes and radiographic results of a single surgeon using a single knee implant design (Consensus Knee System-CKS) operated over a ten-year period (from 2007 thru 2017). The results demonstrated an excellent satisfaction rate of 94%, KOOS scores of 94 to 99, KSS scores (function & pain) both 85, implant survivorship of 97% at 10years, consistent implant placement using the standard TKA instruments, as well as zero implant loosening and no progressive radiolucent lines (RLLs) during the study period. This ten-year study of TKA results demonstrates the importance of a consistent surgical technique performed by a solo surgeon who used a single implant system.
Introduction
More than a million knee replacement surgeries are done each year in the US and studies have shown that patient satisfaction and patient reported outcome measures (PROMs) have been below the expected results [8,5]. Also, consistency of implant positioning has been reported as too variable by many authors [14,15] although now with robotics and virtual/augmented navigation systems some have reported improvement in surgical placement of implants. The number of failed total knee replacements have risen steeply with the increased surgical volumes and revision rates are reported as high as 5-10 % [7,8,9]. The purpose of this study was to test the hypothesis that when limiting surgical variables, such as the surgeon and pre- & post-op protocols, the specific surgical technique, the design and type of implant used will improve PROMs (including satisfaction rates), survivorship and consistency of implant placement compared to historic controls.
Methods
442 knees were operated using a single surgical technique, by a single, private practice surgeon utilizing a single implant design (Consensus Knee System) between 2007 and 2017. 247 0f these patients were available for study. Data was collected through patient phone interviews and in-clinic exams with radiographic evaluations at latest follow-up, and the results are presented in terms of implant survival rates, radiographic findings, and patient- reported outcomes. The implant design was a cruciateretaining, fixed bearing total knee replacement (Consensus Knee System) which had no design modifications over the time of these surgeries. Manual instrumentation (intramedullary femoral and tibial guidance for bone cuts) was used to establish mechanical knee alignment, with femoral and tibial components cemented in the methods described by the senior surgeon.
Clinical follow up was conducted comprising chart review, clinical in-person exams and phone follow-up to retrieve key clinical outcome data, as well as patient-reported outcomes. Patientreported outcomes included the Knee Society Score [1], Knee Injury and Osteoarthritis Outcome Score [2] and a self-administered satisfaction scale [3]. Radiographic ratings for radiolucency and component orientation were defined as per [4]. Data was collected and organized into a spreadsheet file for further analysis.
Analysis
The spreadsheet(s) were read into the RStudio environment
for further analysis. The data was prepared using functions
from tidy verse to reformat variables, as well as identify and
fix data transcription errors (e.g. date of birth with incorrect
year). Additional variables were created for survival analysis
and reformatting of variables to report radiographic findings.
Component orientation was converted from angular measurements
to deviation from neutral coronal alignment for the femur and
tibia, as well as tibial slope (negative=posterior slope) and femoral
flexion (positive=flexion). Radiological findings were categorized
based on the following;
• Presence of radiolucency >=1mm
• Coronal alignment
• Tibial; Target = 0°; Tolerance ±3°
• Femoral; Target = 5° valgus; Tolerance ±2°
• Sagittal alignment
• Tibial slope; Target = 5°; Tolerance ±3°
• Femoral flexion; Target = 0°; Tolerance ±5°
• Patellar tilt; Target = 0°; Tolerance ±5°
Patient characteristics were summarized for continuous variables (median and interquartile ranges) and proportions for categorical variables. Cumulative incidence functions were calculated for implant revision and patient mortality and CIF curves plotted with 95% confidence intervals and the upper limit compared to the ODEP Rating 10A [5]. Patient-reported outcomes were summarized and distributions of the KOOS subscales visualized with median and interquartile range with fixed thresholds for patient acceptable symptom state as reported for 3-year follow up of primary TKR [6].
Results
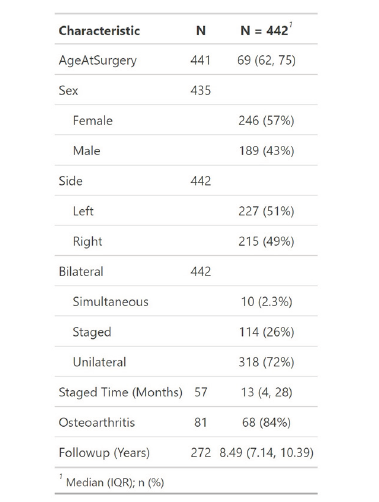
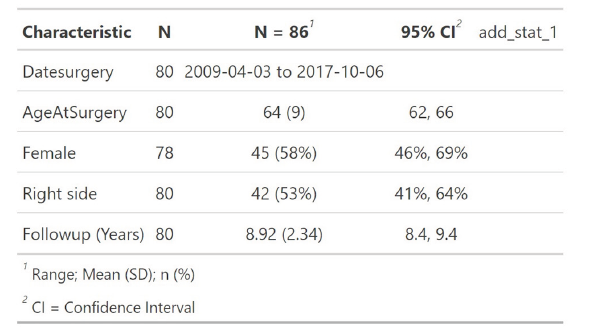
General population of the total eligible sample of 247 cases operated between 29-Jul-2007 to 28-Feb-2017 were available for the study with a subset of 92 of these patients submitting to follow-up exam in the clinic. Overall, the sample was predominantly female (57%), with a median age of 69 years at time of surgery and a diagnosis of isolated knee osteoarthritis. The majority of patients (72%) received a unilateral knee replacement (Table 1). No patients with previous open surgery or below the age of 18 years were considered.
Table 1:Baseline patient characteristics (All eligible).
Implant and patient survival
The competing risks regression identified mortality as a key competing risk for implant revision beyond 5 year follow up (Figure 1). Although the 10-year implant survival was estimated at 3.2%, the upper limit of the confidence limit exceeded the ODEP 10A rating of 5% (Table 2).
Table 2:Summary of competing risks incidence for the analysed sample.
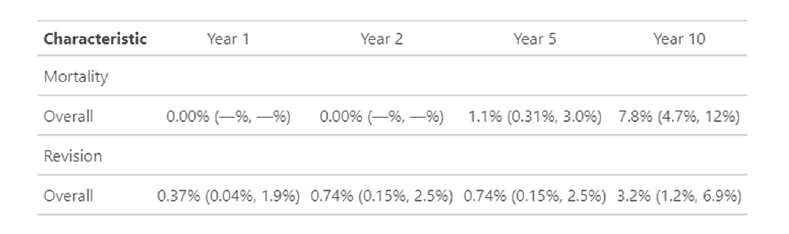
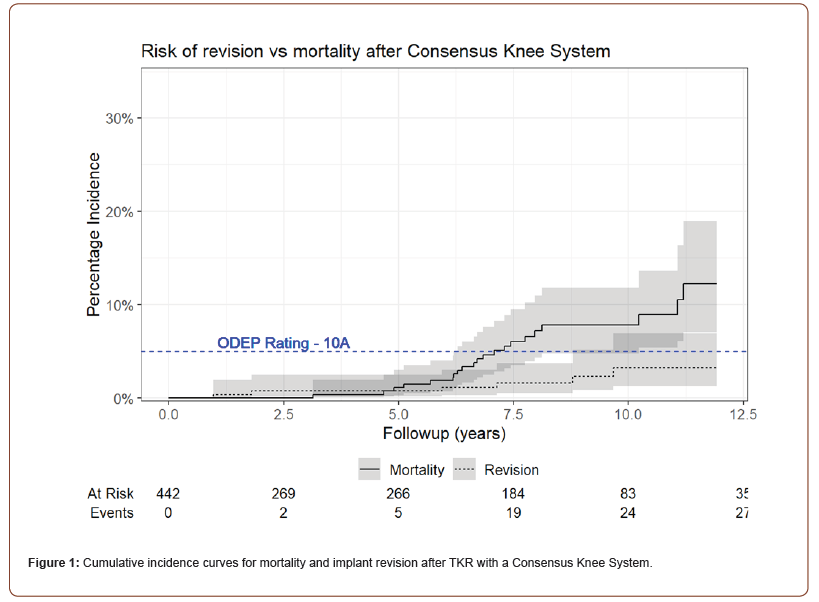
There were eight patients (3.2%) who had revision of their implants during this 10-year period. Of these, four (1.6%) were revised for chronic pain without loosening or infection but with positive nickel sensitivity, two (0.8%) had infections, one had severe poly wear (0.4%) and one had implant instability (0.4 %)
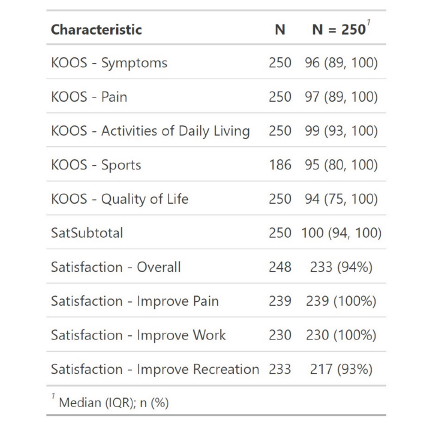
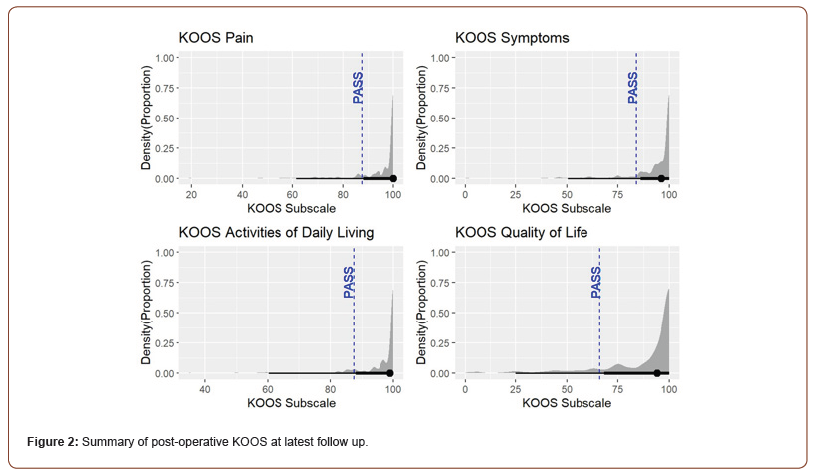
Patient-reported outcomes
Patients returning for their clinic visit returned median KOOS subscales >90 and more than 80% of patients contacted returned a rating of very satisfied or somewhat satisfied (Table 3). Visualization of the KOOS subscale distributions relative to the PASS threshold selected, illustrated the high proportion of patients returning patient acceptable symptoms (Figure 2).
Table 3:Summary of KOOS and patient satisfaction at latest follow up.
Satisfaction reflects proportion of patients responding with “Very satisfied” rating.
Clinical findings
The subset of patients attending clinic review (N = 86) scored >80 on the Knee Society score with a median maximum flexion angle of >120° (Table 4).
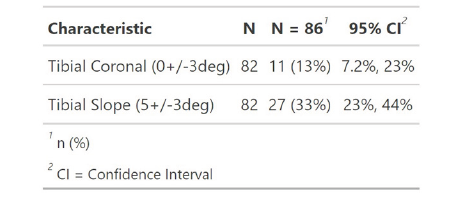
Radiolucency (1mm minimum) was observed in 5 - 39% of cases available for review (Table 5). The majority of femoral components were orientated within tolerance of neutral in the sagittal plane, as well as valgus, the patella component remained in neutral tilt (Table 6), while the majority of tibial components were within tolerance of neutral (Table 7), although the incidence of deviation from target posterior slope was higher.
Table 4a:
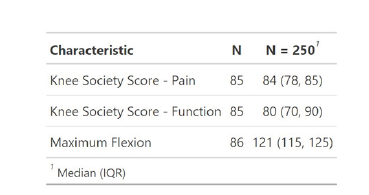
Table 4:Summary of Knee Society Score and maximum flexion assessed in clinic.
Radiological findings
Table 5:Summary of radiolucency at latest follow up.
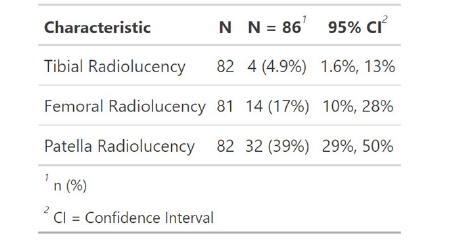
Table 6:Incidence of femoral and patella component orientation outside tolerance at latest follow up.
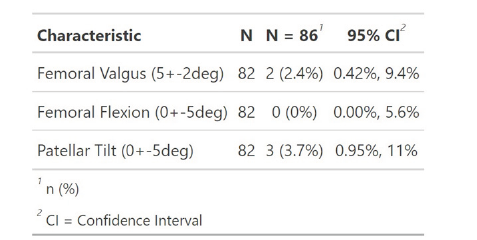
Table 7:Incidence of tibial component orientation outside tolerance at latest follow up.
Discussion
This study demonstrates that a single surgeon using a consistent surgical technique and a single implant design can produce 10- year survival of 97% of cases operated in addition to high patientreported pain relief, function and satisfaction. These high outcome scores exceed published patient acceptable symptom rates.
This study reports implant survival of 97% at 10 years (a lower confidence limit of 93.1%). The majority of revisions (n=8) in this study were for pain and nickel sensitivity without loosening or infection (n= 4), infection (n=2), poly wear (n=1) and implant instability (n=1). These results compare favourably with equivalent implants in both discrete series involving one center or one surgeon, or registry data from the Australian, Swedish, US, UK or European national registries. A cohort of 462 cruciateretaining fixed bearing TKA (Triathlon, Stryker) implanted in Scotland, UK were followed up to 15 years postoperatively [7], with only 42% implant survivorship (retention) at last follow up. A larger retrospective institutional review from Minnesota (USA) of cruciate-retaining fixed bearing TKA (PFC, Depuy), predominantly cemented (96%) (N = 5389, N = 3325 at 10 years) reported allcause implant survival of 92.2% (95%CI 91.0 - 93.4), which is also comparable to the present analysis, particularly with respect to the lower bound of the confidence interval. The most recent report of the Australian Orthopaedic Association National Joint Replacement Registry [8] (Table KT9) reported cemented cruciate-retaining TKA with >3000 procedures with 10-year implant survival ranging from 94.1% (lower CI 93.5) to 97.1% (upper CI 97.3). The present results also compare favourably to this data, although loss to follow up should be considered as a limitation in the estimation process. Patient-Reported Outcomes. A multi-surgeon database study (N = 621, N = 308 at latest follow-up) from Scotland (UK) reported an all-cause implant survival for a posterior-stabilized cemented TKA with selective patella resurfacing at 14 years of 96.5% (no confidence limits reported) [9].
Mortality after TKA at 90-days reported in the literature has displayed a linear decrease over the course of implant usage in this single-surgeon practice (2007 - 2017) [10]. The annualized estimate of mortality has decreased from 1.6% in 2005 to 0.76% in 2015 based on a meta-regression. This provides an overall estimate of mortality at 10 years that ranges from 7.6% to 16%. The estimated upper confidence limit for the present series is 12%, which is well within the boundaries estimated from the meta-regression.
This study reported overall patient satisfaction of 94% at 10 years. Scott et al in 2023 reported satisfaction amongst 88% of the sample at 10 year follow up, which was comparable to the 94% overall satisfaction in the present analysis.
PROMs in this study were both KOOS and KSS. Our reported KOOS varied between 94-99 points, while KSS pain and function were both at 85% at the 10 year mark.
A small New Zealand RCT of fixed (N = 46) vs mobile bearing (N = 39) cruciate-retaining TKA (PFC Sigma, Depuy) [11] reported KOOS scores at 10-year follow up (Table 8). Crude differences between the mean subscales and the median reported in the present analysis reveal superiority of the present series for Symptoms, but the differences for the remaining subscales were smaller than the anchor-based minimal clinically important difference (MCID) for TKA [12].
Table 8:Summary of KOOS findings for fixed-bearing TKA at 10 years follow up.
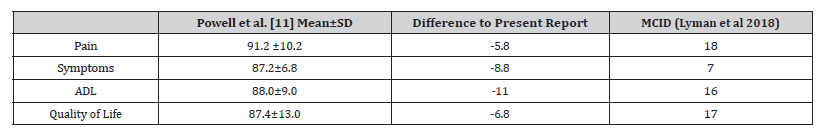
The New Zealand cohort reported an overall KSS score of 87.4 (14.9) and the multi-surgeon cohort from Scotland () reported overall KSS of 89.0 at 10 years. In addition, a prospective cohort of cementless cruciate-retaining fixed-bearing TKA from New York (N = 114) reported a KSS pain score of 93 points.
Radiolucent lines between bone and cement were found in 4.9% of tibial implants, 17% of femoral implants and 39% of patellar implants, but no radiolucencies were progressive suggesting that the cases in this study will continue to remain asymptomatic.
A prospective cohort of cementless cruciate-retaining fixedbearing TKA from New York (N = 114) reported 2.8% incidence of radiolucency (but their criteria and measurements were not as inclusive as the present study) at their 8-year follow up but did not report the information about progression [13]. However, the presence of radiolucency alone has not been associated with future adverse clinical or implant survival outcomes if it is stable [14]. It should be noted also that the incidence of radiolucency varies widely in the literature, regardless of the length of follow up, with others [15] reporting incidence as high as 48% at one year follow up (N = 135), in cemented TKA.
Implant positioning was found to be very consistent in this
study, falling within standard tolerance guidelines (ref) for each
implant component:
Femoral implant AP= 97.6% Femoral implant LAT=100% Tibial
implant AP=87% Tibial implant slope=67%
Recent studies comparing computer navigation, robotic
surgery compared to standard instrumentation have found implant
position variance from standards in 5% to 65%(ref) of patients.
The limitations of this study are length of follow up, percentage of patients lost-to-follow up, and selection bias.
Conclusions
This study found that when consistent surgical techniques & clinical practices were followed with a single implant design (Concensus Knee System), that patient satisfaction was improved compared to historic reports. In addition, patient reported outcome measures (PROMs=KOOS & KSS), implant survivorship, implant placement and measured bone/cement radiolucencies were also improved over other studies found in the literature. In addition, with this implant design over a ten-year period (from 2007 thru 2017) the implant survivorship was 97% at 10years.
These results demonstrate the importance of using both a consistent surgical technique and a single implant system. These factors were shown to be of crucial importance for obtaining excellent patient outcomes and survivorship in TKA.
Conflict of Interest
No conflict of interest.
Acknowledgement
None.
References
- Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, et al. (2012) Development of a new Knee Society scoring system. Clinical Orthopaedics and Related Research 470(1): 20-32.
- Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. The Journal of Orthopaedic and Sports Physical Therapy 28(2): 88-96.
- Mahomed N, Gandhi R, Daltroy L, Katz JN (2011) The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis 591253.
- Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, et al. (2015). Development of a Modern Knee Society Radiographic Evaluation System and Methodology for Total Knee Arthroplasty. The Journal of Arthroplasty 30(12): 2311-2314.
- Methodology for Total Knees. (2020, October 14). Orthopaedic Data Evaluation Panel.
- Connelly JW, Galea VP, Rojanasopondist P, Matuszak SJ, Ingelsrud LH, et al. (2019) Patient Acceptable Symptom State at 1 and 3 Years After Total Knee Arthroplasty: Thresholds for the Knee Injury and Osteoarthritis Outcome Score (KOOS). The Journal of Bone and Joint Surgery. American 101(11): 995-1003.
- Scott CEH, Snowden GT, Cawley W, Bell KR, MacDonald DJ, et al. (2023) Fifteen-year prospective longitudinal cohort study of outcomes following single radius total knee arthroplasty: patient-reported outcome measures, response attrition, and survival. Bone & Joint Open 4(10): 808-816.
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) (2022) Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty.
- Arikupurathu OM, Johnston L, MacInnes A, Nicol G, Nassif M (2019) Medium- to Long-Term Results of the Nexgen Legacy Posterior Stabilized Fixed-Bearing Knee Replacement. The Journal of Knee Surgery 32(06): 554-559.
- Berstock JR, Beswick AD, López-López JA, Whitehouse MR, Blom AW (2018) Mortality After Total Knee Arthroplasty: A Systematic Review of Incidence, Temporal Trends, and Risk Factors. The Journal of Bone and Joint Surgery. American 100(12): 1064-1070.
- Powell AJ, Crua E, Chong BC, Gordon R, McAuslan A, et al. (2018) A randomized prospective study comparing mobile-bearing against fixed-bearing PFC Sigma cruciate-retaining total knee arthroplasties with ten-year minimum follow-up. The Bone & Joint Journal 100-B (10): 1336–1344.
- Lyman S, Lee YY, McLawhorn AS, Islam W, MacLean CH (2018) What Are the Minimal and Substantial Improvements in the HOOS and KOOS and JR Versions After Total Joint Replacement? Clinical Orthopaedics and Related Research 476(12): 2432-2441.
- Harwin SF, Levin JM, Khlopas A, Ramkumar PN, Piuzzi NS, et al. (2018) Cementless Posteriorly Stabilized Total Knee Arthroplasty: Seven-Year Minimum Follow-Up Report. The Journal of Arthroplasty 33(5): 1399-1403.
- Garabano G, Pesciallo CA, Rodriguez J, Perez Alamino L, Tillet F, et al. (2023). Early appearance of radiolucent lines around total knee arthroplasty in rheumatoid arthritis patients. How does it impact the aseptic failure rate and functional outcomes at 13 years of follow-up? Revista Española de Cirugía Ortopédica Y Traumatología 68(3): 239-246.
- Ng HJH, Tan GKY, Tan RG, Kau CY (2022) Incidence of Radiolucent Lines after Cemented Total Knee Arthroplasty. The Archives of Bone and Joint Surgery 10(1): 85-91.
-
W. Andrew Hodge*, Janelle Garnique and Ronald Gardner. Total Knee Replacement Done by A Single Surgeon with a Single Implant Design. Anaest & Sur Open Access J. 6(2): 2025. ASOAJ.MS.ID.000631.
-
Cleft Lip, Cleft Palate, Intravenous Fluids, Repair surgery, Congenital syndrome, ear infections, Anaesthetists
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






